Abstract
Background:
Extremely preterm birth is associated with subsequent behavioral problems. We hypothesized that perinatal systemic inflammation, a risk factor for cerebral white matter injury and cognitive impairment, is associated with behavior problems observed at 2 y.
Methods:
In a cohort of 600 children born before 28 wk gestation, we measured 25 inflammation-related proteins in blood collected on postnatal days 1, 7, and 14, and identified behavior problems using parent responses to the Child Behavior Checklist for Ages 1.5–5 (CBCL/1.5–5) at 2 y of age. A persistent or recurrent protein elevation was defined as a concentration in the highest quartile (for gestational age and postnatal age) on at least 2 d ~1 wk apart. Behavior problems were defined by CBCL/1.5–5 subscale scores at or above the 93rd percentile.
Results:
A single-day elevation of intercellular adhesion molecule-3 was associated with an increased risk of an attention problem, as were persistent or recurrent elevations of myeloperoxidase, interleukin-6, tumor necrosis factor-RI, interleukin-8, intercellular adhesion molecule-3, vascular endothelial growth factor-R1, and vascular endothelial growth factor-R2. These associations persisted among infants without white matter injury and cognitive impairment.
Conclusion:
Among children born extremely prematurely, recurrent, or persistent elevations of inflammation-related proteins in blood during in the first two postnatal weeks are associated with an attention problem at age 2 y.
Similar content being viewed by others
Introduction
Premature and low birth weight newborns are at increased risk for hyperactivity and attention deficit (1). Compared to their peers, children who have an attention deficit disorder are more likely than others to have other behavior problems (2), cognitive impairment (1), do less well in school, (3) and earn less during their employment years (4). The increased risk of attention problems among extremely preterm infants might be explained, in part, by social disadvantage (5), a risk factor for preterm birth, as well as medical complications of preterm birth, such as chronic lung disease, necrotizing enterocolitis, and cerebral white matter injury (1).
Prevention of behavior problems among extremely preterm infants requires an improved understanding of the causal mechanism(s). In this study, we explored a mechanism of perinatal brain injury, i.e., inflammation, which has been associated with cerebral white matter injury (6), impaired early cognitive functioning (7), and cerebral palsy (8). Thus, we hypothesized that perinatal inflammation increases the risk of behavior problems during childhood, and that some of this increase is mediated by cerebral white matter damage.
Results
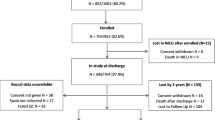
Characteristics of Study Participants
Of the 1,506 newborns enrolled between April 2002 and August 2004, 1,200 survived to 24 mo of postnatal age. The Child Behavior Checklist for Ages 1.5–5 (CBCL/1.5–5) was available for 691 children, and blood protein measurements were available for 600 of these children (50% of surviving participants). The 600 children included in this study differed minimally from the 339 children whose blood proteins were measured, but whose parent did not provide a completed CBCL/1.5–5, except that included children were more likely to have bacteria recovered from their blood after the first postnatal week (30 vs. 19%; Supplementary Tables S1–S3 online).
Possible prenatal initiators of inflammation that were present frequently among study participants included the presence of microorganisms in the placenta and preterm premature rupture of the fetal membranes (Supplementary Table S2 online). The most prevalent postnatal initiator of inflammation was chronic lung disease (Supplementary Table S3 online).
An attention problem was the most prevalent behavior problem, with a frequency of 10%, followed by the withdrawn problem (7%), the somatic problem (6%), and the aggressive behavior problem (5%). Other problems identified with the CBCL/1.5–5 were less prevalent in our sample and are not presented. Each of the behavioral problems occurred 3–12 times more commonly among children who had another behavior problem as among children who did not have that other problem ( Table 1 ).
Protein Elevations and Behavior Problems
Infants with elevated intercellular adhesion molecule (ICAM)-3 on 1 d were more likely than others to have an attention problem, and those with elevated ICAM-1 were less likely to be withdrawn ( Table 2 ). Infants with elevations on two or more days of myeloperoxidase, interleukin-6, tumor necrosis factor-RI, interleukin-8, ICAM-3, vascular endothelial growth factor-R1, and vascular endothelial growth factor-R2 were about twice as likely to have an attention problem as children with lower concentrations of these proteins. An elevation of VEGF-R1 on two or more days was associated with a fourfold increase of a somatic problem. No other problem behaviors were associated with protein elevations on two or more days ( Table 3 ).
Analyses Excluding Infants With Cerebral White Matter Injury or Early Cognitive Impairment
To assess the extent to which an association between elevated concentrations of inflammation-related proteins and an attention problem was a consequence of brain damage or early cognitive impairment, we evaluated the relationship between elevated concentrations of myeloperoxidase, interleukin-6, tumor necrosis factor-RI, interleukin-8, intercellular adhesion molecule-3, vascular endothelial growth factor-R1, and vascular endothelial growth factor-R2 and an attention problem among children who did not have sonographic evidence of brain damage and among children who did not have an mental development index (MDI) <70 (two SD below the reference sample mean). The odds ratios in these two subsamples differed minimally from those in the entire sample ( Table 4 ).
Discussion
Our primary finding is that children born extremely prematurely who had elevated concentrations of inflammation-related proteins in their blood during the first two postnatal weeks are more likely to have an attention problem at 24 postnatal months than are those who did not have recurrently or persistently elevated concentrations. With few exceptions, protein elevations on a single day were not associated with any of the behavior problems measured by the CBCL/1.5–5. In contrast, recurrent or persistent elevations of six proteins were associated with an attention problem. A secondary finding is that the relationships between elevated concentrations of inflammation-related proteins and an attention problem were not a consequence of observable brain damage or early cognitive impairment.
In agreement with prior studies of preterm and low birth weight infants (9,10), we found that the most prevalent abnormal CBCL/1.5–5 symptom scale was an attention problem, with a prevalence of 10%, and this was the only CBCL/1.5–5 scale associated with elevated concentrations of inflammation-related proteins. While other CBCL/1.5–5 scales might not be related to perinatal inflammation, it is also possible that the latent interval between brain injury and clinical signs is longer for other behavioral problems assessed with the CBCL/1.5–5 or that selective vulnerability to inflammation exists in regions of the brain involved in attention. Prior studies in extremely preterm neonates have identified associations between inflammation biomarkers and both structural (6) and functional (7,8) brain abnormalities, but the relationship of such biomarkers specifically to behavior problems has not been studied previously.
As has been the case for other brain disorders (6,7,11), the risk of an attention problem was increased primarily when protein elevations were present on more than 1 d. This suggests that protein elevations that are recurrent or persistent are more highly associated with brain injury than those that are transient. One possibility is that sustained protein elevations reflect systemic inflammation, not specific to the brain. Another possibility is that brain damage is the source of inflammation-related proteins, and that sustained protein elevations reflect continued production of inflammation-related proteins resulting from brain damage.
A synoptic view of the experimental and epidemiologic literature suggests that perinatal exposure to inflammation does indeed lead to abnormalities in brain structure and function, as well as behavioral abnormalities (6,7,11,12). The most recent finding in neonatal mice that repeated exposure to low levels of interleukin-1 results in a reduction in the number of myelinated neurons and of neuronal diameter, as well as long-term memory deficits (13) is in keeping with our major finding of an association between intermittent or sustained systemic inflammation and developmental delay (7) and attention problems as reported in this paper. One neuropathologic mechanism likely to be involved in this scenario is the migration of neurons through a “minefield” of activated microglia on their way from the ventricular zone towards the developing cortex (14). Although attention impairment is highly heritable (15), perinatal inflammation could be an important risk factor, since in a murine model; the detrimental effect of perinatal inflammation on attention is accentuated by a mutation affecting dopaminergic neurons (16).
In our sample, the association between elevated concentrations of inflammation-related proteins during the first two postnatal weeks and a CBCL/1.5-5-defined attention problem at age 2 y does not appear to be a consequence of sonographically detectable brain damage. This finding should be viewed with caution because detection of cerebral white matter damage by ultrasound has modest sensitivity for white matter abnormalities (17). Others, however, by using more sensitive imaging techniques, found structural correlates of attention problems, especially in the frontostriatal fiber tracts (18,19). Because we could not assess fiber tract integrity, we could not evaluate the possibility that our associations of inflammation with attention dysfunction reflect disordered structure of the tract in the frontal lobe or other components of attention networks.
Among children born extremely premature, attention deficit is associated with cognitive impairment (20). In the extremely low gestational age newborn (ELGAN) cohort, cognitive impairment has been associated with elevations of inflammation-related proteins (7). However, in this study we found an association between inflammation and an attention problem even when infants with cognitive impairment were excluded from our analyses.
Extremely preterm infants frequently are exposed to prenatal and postnatal initiators of inflammation. In the sample studied here, the group of pregnancy disorders identified as spontaneous indications for preterm delivery have each been shown to be associated with histologic inflammation of the placenta and the recovery of bacteria from the placenta (21). These pregnancy disorders (22), histologic inflammation of the placenta (23), and recovery of microorganisms from the placenta (24) have each been associated with early systemic inflammation in very preterm newborns. Consequently, antenatal inflammatory stimuli can contribute to a systemic fetal inflammatory response. On the other hand, in this sample, postnatal bacteremia (25), necrotizing enterocolitis (26), and assisted ventilation for two or more weeks (27) have preceded or accompanied systemic inflammation. Both prenatal and postnatal inflammation might be attenuated by pharmacological interventions (28,29).
A possible limitation of our study is that only 50% of our cohort of extremely preterm survivors had both data elements required for this study, which could be a source of bias. Cohort members who were included were less likely to be born to mothers eligible for public assistance. However, it is unlikely that our findings are attributable to selection bias because social disadvantage, which was slightly underrepresented among study participants, would be expected to add to (30) or accentuate (31) the associations we found between biological risk factors and developmental impairments among preterm infants. A second limitation is that the primary outcomes in this study, parent-reported behavioral problems, are only moderately stable over time. The correlation coefficient for CBCL scores for attention problems assessed 8 y apart has been found to be 0.37 (32).
Our finding that elevated levels of inflammation-related proteins are associated with attention problems at 2 y could have implications for efforts to improve the quality of life for extremely preterm infants. Immunomodulatory interventions might decrease the risk of attention problems. Infants with indicators of perinatal inflammation could be targeted for special assessment of attention, followed by interventions to improve attention, when appropriate.
In conclusion, among children born extremely preterm, recurrently or persistently elevated blood levels of inflammation-related proteins in the first two postnatal weeks are associated with an increased risk of an attention problem at 24 mo of age. Observable brain damage and significantly limited early cognitive functioning do not appear to be an intermediary between early systemic inflammation and a later attention problem.
Methods
Subjects
The ELGAN study is a multicenter observational study of the antecedents of brain disorders in extremely preterm infants (33). During the years 2002–2004, women delivering before 28 wk gestation at 1 out of 14 participating institutions in 11 cities in 5 states were asked to enroll in the study. The sample for this report consists of the 600 newborns enrolled in the ELGAN study for whom protein measurements on at least two of the three protocol days (days 1, 7, and 14) and T scores derived from the CBCL/1.5–5 were available. The enrollment and consent processes were approved by the Institutional Review Board at Wake Forest School of Medicine and the Institutional Review Boards at all participating institutions. The parents of all participants provided informed consent.
Clinical Data
Mothers were interviewed about their reproductive health and medications taken during pregnancy. Their medical records were reviewed to obtain information about complications and treatments during pregnancy, labor, and delivery.
Gestational age (GA) estimates were based on a hierarchy of the quality of available information. Most estimates were based on the dates of embryo retrieval, intrauterine insemination, or fetal ultrasound before the 14th wk (62%). When these data were not available, estimates were made, sequentially, on a fetal ultrasound at 14 or more weeks (29%), last menstrual period without fetal ultrasound (7%), and GA) recorded in the log of the neonatal intensive care unit (1%).
The birth weight was obtained from infant’s medical record and the birth weight Z-score was defined as the number of standard deviations the infant’s birth weight was above or below the median weight of infants of the same GA in referent samples not delivered for preeclampsia or fetal indications.
Protocol ultrasound scans were obtained between the first and fourth day, between the fifth and fourteenth day, and between the fifteenth day and the 40th wk postmenstrual age (i.e., postconceptional age). Each set included the six standard quasi-coronal views and five sagittal views using the anterior fontanel as the sonographic window. Efforts to increase reliability of ultrasound interpretations are described in detail elsewhere (34).
Measurement of Inflammation-Related Proteins
Drops of blood were collected on filter paper (Schleicher & Schuell 903, Whatman International, Florham Park, NJ) on the first postnatal day (range: 1–3 d), the 7th postnatal day (range: 5–8 d), and the 14th postnatal day (range: 12–15 d). These drops of blood remained after specimens were obtained for clinical indications. Dried blood spots were stored at −70 °C in sealed bags with desiccant until processed.
For protein elution, 12 mm punched biopsies of the frozen blood spots were submerged in 300 μl phosphate-buffered saline containing 0.1% Triton X100 (Sigma-Aldrich, St Louis, MO) and 0.03% Tween-20 (Fisher, Hampton, NH), vortexed for 30 s, and incubated on a shaker for 1 h at 4 °C. The buffer and biopsy were then transferred over the filter of a SpinX tube (Corning, Fisher), centrifuged at 2,000×g followed by collection of the filtered eluted blood. An additional wash of the punch was performed in 100 μl for a final elution volume of 400 μl.
Proteins were measured in duplicate in the Laboratory of Genital Tract Biology of the Department of Obstetrics, Gynecology, and Reproductive Biology at Brigham and Women’s Hospital, Boston, MA with an electrochemiluminescence multiplex detection system (MSD multiplex platform, Sector Imager 2400, Discovery Workbench Software, both from Meso Scale Siscovery (MSD), Gaithersburg, MD) that has been validated by comparisons with traditional enzyme-linked immunosorbent assay (35,36).
The multiplex assays were optimized to allow detection of each biomarker within the linearity range of the eluted samples. Consequently, the 25 proteins were measured on three separate multiplex platforms allowing assessment of each protein within the assay sensitivity and the linearity range of the samples. The low limit of detection of each protein is calculated as the mean + 2.5 SD of the blank of each detection antibody. The Meso Scale Discovery technology and software eliminate any interspot cross talk within the linearity range. Split quality control blood pools tested on each plate showed interassay variation of below 20% for each protein.
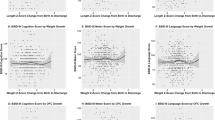
The total protein concentration in each eluted sample was determined by bicinchoninic acid assay (Thermo Scientific, Rockford, IL) using a multi-label Victor 2 counter (Perkin Elmer, Boston, MA) and measurements made in duplicate of each analyte normalized to mg total protein. The concentrations of all proteins were measured as picograms/mg total protein, but all analyses classified children by the quartile in which each protein concentration fell.
We measured the following 25 proteins: c-reactive protein (CRP), serum amyloid A (SAA), myeloperoxidase (MPO), interleukin-1β (IL β-1), interleukin-6 (IL-6), interleukin-6 receptor (IL-6R), tumor necrosis factor-α (TNF-α), tumor necrosis factor receptor-1 (TNF-R1), tumor necrosis factor receptor-2 (TNF-R2), interleukin-8 (IL-8; CXCL8), monocyte chemotactic protein-1 (MCP-1; CCL2), monocyte chemotactic protein-4 (MCP-4; CCL13), macrophage inflammatory protein-1β (MIP-1β; CCL4), regulated upon activation, normal T-cell expressed, and [presumably] secreted (RANTES; CCL5), interferon-inducible T cell α-chemoattractant (I-TAC; CXCL11), intercellular adhesion molecule-1 (ICAM-1; CD54), intercellular adhesion molecule-3 (ICAM-3; CD50), vascular cell adhesion molecule-1 VCAM-1; CD106), E-selectin (CD62E), matrix metalloproteinase-1 (MMP-1), matrix metalloproteinase-9 (MMP-9), vascular endothelial growth factor (VEGF), vascular endothelial growth factor receptor-1(VEGF-R1; Flt-1), vascular endothelial growth factor receptor-2 (VEGF-R2; KDR), insulin-like growth factor binding protein-1 (IGFBP-1).
Because protein concentrations varied with GA at delivery and with the postnatal day of collection, we divided our sample into nine groups defined by three GA categories (23–24, 25–26, 27 wk) crossed with the 3 d (1,7,14) of blood collection. Because we were interested in the contribution of high protein concentrations, and none of them followed a normal distribution, we dichotomized between the highest quartile and the lower three quartiles of the distribution of each protein’s concentration within each of the nine groups.
Identification of Behavior Problems
Approximately 2 y from each infant’s expected date of delivery, we obtained parent or guardian’s ratings on the CBCL/1.5–5. According to the CBCL/1.5–5 test manual, T scores between the 93rd and 97th percentile are in the borderline range and T scores above the 97th percentile are in the significant range of clinical concern (37). For our analyses, we considered infants with T scores at or above the 93rd percentile to have a behavior problem. Seven symptom scales (emotionally reactive, anxious/depressed, somatic complaints, withdrawn, sleep problems, attention problems, and aggressive behavior) and two broad symptom clusters (internalizing and externalizing) were considered. The internalizing cluster consisted of emotionally reactive, anxious/depressed, somatic complaints, and withdrawn; the externalizing cluster consisted of attention problems and aggressive behavior.
Identification of Impaired Early Cognitive Functioning
Each infant was evaluated with the Bayley Scales of Infant Development-II (BSID-II), a standardized assessment of infant cognitive and motor function, which yields a MDI (38) that is modestly predictive of intelligence quotient (39). The BSID-II manual defines a significant delay as a MDI below 70, i.e., 2 SD below the mean in the standardization sample. In this study, we used MDI <70 to classify children as having significantly limited early cognitive functioning. When a child’s visual or neurological impairments precluded assessment with the BSID-II, or more than two items were omitted or judged to be “unscorable,” the child was classified as not testable on that scale. The Adaptive Behavioral Composite of the Vineland Adaptive Behavior Scales (40) was used to approximate the mental scale score of children who were considered not testable with the BSID-II. Certified examiners administered and scored the BSID-II. All examiners were experienced users of the BSID-II and, specifically for the ELGAN study, attended a 1-d workshop to review published guidelines for test administration and videotaped examinations. Examiners were aware of the child’s enrollment in the ELGAN study and corrected age, but not the child’s medical history, brain ultrasound abnormalities, or blood levels of inflammation-related proteins.
Statistical Analysis
We defined an elevation of an inflammation-related protein as a concentration in the top quartile for infant GA and the postnatal day the specimen was obtained. We evaluated the null hypotheses that elevations of inflammation-related proteins on days 1, 7, and 14, and persistent or recurrent elevations of these proteins, defined as elevated concentrations of a protein on at least 2 d ~1 wk apart, are not associated with behavior problems, as defined above.
We expressed the strength of association between elevated concentrations of inflammation-related proteins and each behavior problem with odds ratios and 99% confidence intervals. We selected the 99% confidence interval, rather than the conventional 95% interval, to account for multiple comparisons (25 proteins measured at three times), while not appreciably increasing the risk of a Type II (false negative) error. To estimate odds ratios and 99% confidence intervals, we used logistic regression models which adjusted for GA, birth weight Z-score, first pregnancy, and multifetal pregnancy. These variables were selected as potential confounders because in preliminary analyses they were associated with both a protein elevation and a behavior problem at a significance level of P < 0.2.
We explored the possibilities that either cerebral white matter damage or significantly delayed early cognitive functioning was an intermediary between elevated concentrations of inflammation-related proteins and a behavior problem by repeating our analyses after excluding the 91 children who had an echolucent lesion in the cerebral white matter or moderate-to-severe ventricular enlargement or the 158 infants with an MDI below 70.
Statement of Financial Support
This study was supported by cooperative agreements with the National Institute of Neurological Disorders and Stroke, Bethesda, Maryland (5U01NS040069-05; 2R01NS040069 - 06A2) and a center grant award from the National Institute of Child Health and Human Development, Bethesda, Maryland (5P30HD018655-28).
Disclosure
The authors state that they have no conflicts of interest.
References
O’Shea TM, Downey LC, Kuban KK . Extreme prematurity and attention deficit: epidemiology and prevention. Front Hum Neurosci 2013;7:578.
Kirkhaug B, Drugli MB, Lydersen S, Mørch WT . Associations between high levels of conduct problems and co-occurring problems among the youngest boys and girls in schools: a cross-sectional study. Nord J Psychiatry 2013;67:225–32.
Polderman TJ, Boomsma DI, Bartels M, Verhulst FC, Huizink AC . A systematic review of prospective studies on attention problems and academic achievement. Acta Psychiatr Scand 2010;122:271–84.
Knapp M, King D, Healey A, Thomas C . Economic outcomes in adulthood and their associations with antisocial conduct, attention deficit and anxiety problems in childhood. J Ment Health Policy Econ 2011;14:137–47.
Reiss F . Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 2013;90:24–31.
Leviton A, Kuban K, O’Shea TM, et al. The relationship between early concentrations of 25 blood proteins and cerebral white matter injury in preterm newborns: the ELGAN study. J Pediatr 2011;158:897–903.e1–5.
O’Shea TM, Allred EN, Kuban KC, et al.; Extremely Low Gestational Age Newborn (ELGAN) Study Investigators. Elevated concentrations of inflammation-related proteins in postnatal blood predict severe developmental delay at 2 years of age in extremely preterm infants. J Pediatr 2012;160:395–401.e4.
Kuban K, O’Shea TM, Allred EN, et al. Systemic inflammation and cerebral palsy risk in extremely preterm infants. J Child Neurol 2014; e-pub ahead of print 18 March 2014.
Reijneveld SA, de Kleine MJ, van Baar AL, et al. Behavioural and emotional problems in very preterm and very low birthweight infants at age 5 years. Arch Dis Child Fetal Neonatal Ed 2006;91:F423–8.
Scott MN, Taylor HG, Fristad MA, et al. Behavior disorders in extremely preterm/extremely low birth weight children in kindergarten. J Dev Behav Pediatr 2012;33:202–13.
Leviton A, Kuban KC, Allred EN, Fichorova RN, O’Shea TM, Paneth N ; ELGAN Study Investigators. Early postnatal blood concentrations of inflammation-related proteins and microcephaly two years later in infants born before the 28th post-menstrual week. Early Hum Dev 2011;87:325–30.
Meyer U, Feldon J, Dammann O . Schizophrenia and autism: both shared and disorder-specific pathogenesis via perinatal inflammation? Pediatr Res 2011;69(5 Pt 2):26R–33R.
Favrais G, van de Looij Y, Fleiss B, et al. Systemic inflammation disrupts the developmental program of white matter. Ann Neurol 2011;70:550–65.
Leviton A, Gressens P . Neuronal damage accompanies perinatal white-matter damage. Trends Neurosci 2007;30:473–8.
Elia J, Sackett J, Turner T, et al. Attention-deficit/hyperactivity disorder genomics: update for clinicians. Curr Psychiatry Rep 2012;14:579–89.
Vuillermot S, Joodmardi E, Perlmann T, Ögren SO, Feldon J, Meyer U . Prenatal immune activation interacts with genetic Nurr1 deficiency in the development of attentional impairments. J Neurosci 2012;32:436–51.
Miller SP, Cozzio CC, Goldstein RB, et al. Comparing the diagnosis of white matter injury in premature newborns with serial MR imaging and transfontanel ultrasonography findings. AJNR Am J Neuroradiol 2003;24:1661–9.
de la Fuente A, Xia SG, Branch C, Li XB . A review of attention-deficit/hyperactivity disorder from the perspective of brain networks. Front Hum Neurosci 2013; 7:192.
Shang CY, Wu YH, Gau SS, Tseng WY . Disturbed microstructural integrity of the frontostriatal fiber pathways and executive dysfunction in children with attention deficit hyperactivity disorder. Psychol Med 2013;43:1093–107.
Johnson S, Hollis C, Kochhar P, Hennessy E, Wolke D, Marlow N . Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J Am Acad Child Adolesc Psychiatry 2010;49:453–63.e1.
McElrath TF, Hecht JL, Dammann O, et al.; ELGAN Study Investigators. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol 2008;168:980–9.
McElrath TF, Fichorova RN, Allred EN, et al.; ELGAN Study Investigators. Blood protein profiles of infants born before 28 weeks differ by pregnancy complication. Am J Obstet Gynecol 2011;204:418.e1–418.e12.
Hecht JL, Fichorova RN, Tang VF, Allred EN, McElrath TF, Leviton A ; Elgan Study Investigators. Relationship Between Neonatal Blood Protein Concentrations and Placenta Histologic Characteristics in Extremely Low GA Newborns. Pediatr Res 2011;69:68–73.
Fichorova RN, Onderdonk AB, Yamamoto H, et al.; Extremely Low Gestation Age Newborns (ELGAN) Study Investigators. Maternal microbe-specific modulation of inflammatory response in extremely low-gestational-age newborns. MBio 2011;2:e00280–10.
Leviton A, O’Shea TM, Bednarek FJ, Allred EN, Fichorova RN, Dammann O ; ELGAN Study Investigators. Systemic responses of preterm newborns with presumed or documented bacteraemia. Acta Paediatr 2012;101:355–9.
Martin CR, Bellomy M, Allred EN, Fichorova RN, Leviton A . Systemic inflammation associated with severe intestinal injury in extremely low gestational age newborns. Fetal Pediatr Pathol 2013;32:222–34.
Bose CL, Laughon MM, Allred EN, et al.; ELGAN Study Investigators. Systemic inflammation associated with mechanical ventilation among extremely preterm infants. Cytokine 2013;61:315–22.
Beloosesky R, Ginsberg Y, Khatib N, et al. Prophylactic maternal N-acetylcysteine in rats prevents maternal inflammation-induced offspring cerebral injury shown on magnetic resonance imaging. Am J Obstet Gynecol 2013;208:213.e1–6.
Gitto E, Reiter RJ, Sabatino G, et al. Correlation among cytokines, bronchopulmonary dysplasia and modality of ventilation in preterm newborns: improvement with melatonin treatment. J Pineal Res 2005;39:287–93.
Leonard CH, Clyman RI, Piecuch RE, Juster RP, Ballard RA, Behle MB . Effect of medical and social risk factors on outcome of prematurity and very low birth weight. J Pediatr 1990;116:620–6.
Thompson RJ Jr, Goldstein RF, Oehler JM, Gustafson KE, Catlett AT, Brazy JE . Developmental outcome of very low birth weight infants as a function of biological risk and psychosocial risk. J Dev Behav Pediatr 1994;15:232–8.
Anselmi L, Barros FC, Teodoro ML, et al. Continuity of behavioral and emotional problems from pre-school years to pre-adolescence in a developing country. J Child Psychol Psychiatry 2008;49:499–507.
O’Shea TM, Allred EN, Dammann O, et al.; ELGAN study Investigators. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum Dev 2009;85:719–25.
Kuban K, Adler I, Allred EN, et al. Observer variability assessing US scans of the preterm brain: the ELGAN study. Pediatr Radiol 2007;37:1201–8.
Fichorova RN, Richardson-Harman N, Alfano M, et al. Biological and technical variables affecting immunoassay recovery of cytokines from human serum and simulated vaginal fluid: a multicenter study. Anal Chem 2008;80:4741–51.
Fichorova RN, Trifonova RT, Gilbert RO, et al. Trichomonas vaginalis lipophosphoglycan triggers a selective upregulation of cytokines by human female reproductive tract epithelial cells. Infect Immun 2006;74:5773–9.
Achenbach TM, Rescorla LA . 2000 Manual for the ASEBA Preschool Forms and Profiles. Burlington, Vermont: University of Vermont, Research Center for Children, Youth, and Families, 2000.
Bayley N . Bayley Scales of Infant Development-Second Edition. San Antonio, TX: Psychological Corporation, 1993.
Roberts G, Anderson PJ, Doyle LW ; Victorian Infant Collaborative Study Group. The stability of the diagnosis of developmental disability between ages 2 and 8 in a geographic cohort of very preterm children born in 1997. Arch Dis Child 2010;95:786–90.
Sparrow SS, Balla DA, Cicchetti DV . Vineland Adaptive Behavioral Scales. Circle Pines, MN: American Guidance Service, 1984.
Acknowledgements
The authors gratefully acknowledge the contributions of their subjects, and their subjects’ families, as well as those of their colleagues. The participating institutions and ELGAN Study collaborators who made this report possible are: Children’s Hospital, Boston, Massachusetts: Kathleen Lee, Anne McGovern, Jill Gambardella, Susan Ursprung, Ruth Blomquist Kristen Ecklund, Haim Bassan, Samantha Butler, Adré Duplessis, Cecil Hahn, Catherine Limperopoulos, Omar Khwaja, Janet S. Soul; Baystate Medical Center, Springfield, Massachusetts: Karen Christianson, Frederick Hampf, Herbert Gilmore, Susan McQuiston; Beth Israel Deaconess Medical Center, Boston, Massachusetts: Camilia R. Martin, Colleen Hallisey, Caitlin Hurley, Miren Creixell, Jane Share; Brigham & Women’s Hospital, Boston, Massachusetts: Linda J. Van Marter, Sara Durfee; Massachusetts General Hospital, Boston, Massachusetts: Robert M. Insoft, Jennifer G. Wilson, Maureen Pimental, Sjirk J. Westra, Kalpathy Krishnamoorthy; Floating Hospital for Children at Tufts Medical Center, Boston, Massachusetts: Cynthia Cole, John M. Fiascone, Janet Madden, Ellen Nylen, Anne Furey, Roy McCauley, Paige T. Church, Cecelia Keller, Karen J. Miller; U Mass Memorial Health Care, Worcester, Massachusetts: Francis Bednarek (deceased), Mary Naples, Beth Powers, Jacqueline Wellman, Robin Adair, Richard Bream, Alice Miller, Albert Scheiner, Christy Stine; Yale University School of Medicine, New Haven, Connecticut: Richard Ehrenkranz, Joanne Williams, Elaine Romano; Wake Forest University Baptist Medical Center and Forsyth Medical Center, Winston-Salem, North Carolina: T. Michael O’Shea, Debbie Gordon, Teresa Harold, Barbara Specter, Deborah Allred, Robert Dillard, Don Goldstein, Deborah Hiatt (deceased), Gail Hounshell, Ellen Waldrep, Lisa Washburn, Cherrie D. Welch; University Health Systems of Eastern Carolina, Greenville, North Carolina: Stephen C. Engelke, Sherry Moseley, Linda Pare, Donna Smart, Joan Wilson, Ira Adler, Sharon Buckwald, Rebecca Helms, Kathyrn Kerkering, Scott S. MacGilvray, Peter Resnik; North Carolina Children’s Hospital, Chapel Hill, North Carolina: Carl Bose, Gennie Bose, Lynn A. Fordham, Lisa Bostic, Diane Marshall, Kristi Milowic, Janice Wereszczak; Helen DeVos Children’s Hospital, Grand Rapids, Michigan: Mariel Poortenga, Dinah Sutton, Bradford W. Betz, Steven L. Bezinque, Joseph Junewick, Wendy Burdo-Hartman, Lynn Fagerman, Kim Lohr, Steve Pastyrnak; Sparrow Hospital, Lansing, Michigan: Carolyn Solomon, Ellen Cavenagh, Victoria J. Caine, Nicholas Olomu, Joan Price; Michigan State University, East Lansing, Michgan: Nigel Paneth, Padmani Karna, Madeleine Lenski; University of Chicago Medical Center, Chicago, Illinois: Michael D. Schreiber, Grace Yoon, Kate Feinstein, Leslie Caldarelli, Sunila E. O’Connor, Michael Msall, Susan Plesha-Troyke; William Beaumont Hospital, Royal Oak, Michigan: Daniel Batton, Beth Kring, Karen Brooklier, Melisa J. Oca, Katherine M. Solomon; Arkansas Children’s Hospital, Little Rock, Arkansas: Joanna J. Seibert; Children’s Healthcare of Atlanta: Robert Lorenzo.
Author information
Authors and Affiliations
Consortia
Corresponding author
Supplementary information
Supplementary Table S1
(DOC 43 kb)
Supplementary Table S2
(DOC 41 kb)
Supplementary Table S3
(DOC 57 kb)
Rights and permissions
About this article
Cite this article
O’Shea, T., Joseph, R., Kuban, K. et al. Elevated blood levels of inflammation-related proteins are associated with an attention problem at age 24 mo in extremely preterm infants. Pediatr Res 75, 781–787 (2014). https://doi.org/10.1038/pr.2014.41
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2014.41
This article is cited by
-
Environmental influences on child health outcomes: cohorts of individuals born very preterm
Pediatric Research (2023)
-
Cortisol and inflammatory biomarker levels in youths with attention deficit hyperactivity disorder (ADHD): evidence from a systematic review with meta-analysis
Translational Psychiatry (2021)
-
COVID-19 threatens maternal mental health and infant development: possible paths from stress and isolation to adverse outcomes and a call for research and practice
Child Psychiatry & Human Development (2021)
-
In-line filtration in very preterm neonates: a randomized controlled trial
Scientific Reports (2020)
-
Early Motor Differences in Infants at Elevated Likelihood of Autism Spectrum Disorder and/or Attention Deficit Hyperactivity Disorder
Journal of Autism and Developmental Disorders (2020)