Abstract
Background:
The aim of this work was to investigate in a prospective study whether moderate hyperbilirubinemia in healthy term neonates is associated with an increase of minor neurological dysfunction (MND) and behavioral problems up to 18 mo.
Method:
We enrolled 43 healthy term infants with a bilirubin level ≥220 µmol/l (BILI group) at 72–96 h postnatally at the University Medical Center Groningen (UMCG), including eight referrals for hyperbilirubinemia. Seventy healthy term infants born at the UMCG with bilirubin level <220 µmol/l served as comparisons (COMP group). We evaluated the neurologic condition neonatally and at 3 and 18 mo; behavior was evaluated at birth and 18 mo.
Results:
Rates of MND in BILI and COMP groups were similar at all ages. However, bilirubin levels of ≥300 µmol/l (n = 10) were associated with an increased risk of complex MND (odds ratio: 4.21; 95% confidence interval: 1.02–17.37). Neonatally, BILI infants were more often lethargic than COMP infants (odds ratio: 3.54; 95% confidence interval: 1.32–9.51); at 18 mo, they had higher hyperactivity scores (effect: 0.32; 95% confidence interval: 0.08–0.56).
Conclusion:
Occurrence of complex MND at 18 mo in infants with moderate hyperbilirubinemia was not different from that in comparison infants, but bilirubin level ≥300 was associated with an increased risk of complex MND. This study also suggests that minor behavioral effects of moderate hyperbilirubinemia cannot be excluded.
Similar content being viewed by others
Main
Hyperbilirubinemia in newborn infants is treated according to an algorithm in which neonates >35 wk of gestational age without jaundice or without risk factors for the development of severe hyperbilirubinemia are considered as having low risk for hyperbilirubinemia and they may be discharged >72 h after birth. When postnatal age is <72 h or if risk factors are present, discharge is allowed if follow-up ensured. Otherwise, a predischarge total serum bilirubin or transcutaneous bilirubin measurement should be performed. Subsequently, the bilirubin level is plotted in an hour-specific nomogram according to the infant’s age in hours. Treatment will be started if the infants fulfill the criteria for treatment. For instance, at 72 h, phototherapy is started in the lower-risk group (≥38 wk and well) at 300 μmol/l. In the Netherlands, an adapted version, which takes into account the relatively large number of home deliveries, was developed in 2009 (1). The Dutch adaptation does not include an obligatory observational period in the hospital and age at discharge but takes two structured clinical evaluations during the first 4 d as a starting point. In case of suspicion of hyperbilirubinemia, total serum bilirubin/transcutaneous bilirubin is measured (1).
We previously reported in a small group of term babies a strong dose–response relationship between the degree of hyperbilirubinemia and the severity of minor neurological dysfunction (MND) at 12 mo. The data suggested that in healthy term neonates, bilirubin levels should not exceed 335 μmol/l (2). The primary aim of the current study is to replicate the previous study in a larger sample size and evaluate whether moderate hyperbilirubinemia in healthy term infants is associated with an increase of MND at 18 mo. Moreover, in addition to being a replication study in a larger sample at a somewhat older age, the current study evaluated behavior with standardized tools. Secondary aims are to evaluate whether moderate hyperbilirubinemia is associated with an increase of (i) neonatal neurobehavioral dysfunction, (ii) MND at 3 mo, or (iii) behavioral problems at 18 mo.
Results
The bilirubin level of the BILI group varied from 220 to 366 µmol/l, including 10 infants who had levels ≥300 µmol/l. None of the infants, however, had received treatment for hyperbilirubinemia. We paid special attention to the subgroup with bilirubin levels ≥300 µmol/l, because these infants should receive phototherapy according to the treatment guidelines.
The BILI and COMP groups differ not only in the level of bilirubin levels but also in gestational age, maternal age, the prevalence of birth weight below the 10th percentile, and use of cesarean section ( Table 1 ). All children had the neonatal assessments, but for three who missed the assessments at 3 and 18 mo. Attrition was because of the loss of parental interest in the study for two infants (one BILI infant and one COMP infant) and because of the diagnosis of cystic fibrosis in one COMP infant ( Figure 1 ).
At the age of 18 mo, none of the children showed frank neurologic pathology. Logistic regression analysis confirmed that the rate of complex MND was similar in the two groups ( Table 2 ). Subgroup analysis carried out with logistic regression analysis revealed that children with a bilirubin level of ≥300 µmol/l showed complex MND significantly more often than children with a bilirubin level <300 µmol/l ( Tables 2 and 3 ). Most children with complex MND showed abnormalities in muscle tone regulation in combination with postural and reflex dysfunction.
In the neonatal period, none of the infants showed a definitely abnormal neurologic condition. Moreover, according to the results of logistic regression analysis, the rate of MND in the BILI group did not differ significantly from that in the COMP group. Behaviorally, neonates of the BILI group showed lethargy more often than the COMP ( Table 2 ). Logistic regression analysis confirmed this. None of the lethargic infants showed signs of dehydration.
At the age of 3 mo, one infant in the COMP group showed definitely abnormal general movements. Mildly abnormal general movements occurred with a similar frequency in both cohorts, which was confirmed by multivariable analysis ( Table 2 ).
Seven children had mildly abnormal assessments at all ages. Three of them had a bilirubin level ≥220 µmol/l and two had a bilirubin level ≥300 µmol/l.
At 18 mo, the infants of the BILI group showed a higher activity level than those of the COMP group, as confirmed by the linear regression analysis ( Table 2 ). The differences in behavior could not be attributed to the infants with a bilirubin level ≥300 µmol/l ( Table 3 ).
Discussion
The current study showed that up to 18 mo of age, term infants with moderate degrees of hyperbilirubinemia have rates of MND similar to those of comparison infants. The findings of our study, which used sensitive measures for neurodevelopmental outcome, are in line with the results of three previous studies that indicated that moderate hyperbilirubinemia (<342 µmol/l) in healthy term infants does not affect neurological outcome (3,4,5).
However, we found some minor behavioral differences; neonatally, the infants with moderate hyperbilirubinemia showed lethargy more often than the comparison infants. This corresponds to the notion that lethargy is one of the signs of acute neonatal hyperbilirubinemia (6). At 18 mo, the children with moderate hyperbilirubinemia were more active than the infants without moderate hyperbilirubinemia. The latter finding is at variance with previous studies (2,7,8,9). However, Jangaard et al. (8) found a relationship between a bilirubin level of ≥325 µmol/l and attention-deficit disorder and an association of bilirubin level ≥230 µmol/l with autism. The differences between the various studies may be because of the differences in age at which behavior was assessed and the method by which behavior was evaluated.
The fact that we enrolled infants with bilirubin levels above the criterion for “moderate” hyperbilirubinemia illustrates that theoretically sound guidelines do not always function appropriately in daily clinical life. The children with bilirubin levels ≥300 μmol/l at 72–96 h postpartum showed complex MND more frequently than the others. This suggests that these bilirubin levels contribute even more to the development of complex MND than other perinatal and environmental factors. This finding is in agreement with other studies that reported an excess of minor motor problems in infants with bilirubin levels of ≥342 μmol/l (3,10), 342–375 μmol/l (11), or 335–444 μmol/l (2). Other studies did not find an effect of bilirubin levels of ≥427 μmol/l (12), 342–513 μmol/l (13), or ≥428 µmol/l (9) on developmental outcome. The study by Vandborg et al. (12) evaluated the developmental outcome between 1 and 5 y according to the parent-completed Ages and Stages Questionnaire; the study conducted by Heimler et al. (13) applied the Bayley Scales of Infant Development–2 at 3 y; and the study by Newman et al. (9) conducted standard neurologic examinations with an overall impression at a five-point scale. All three instruments are, however, less sensitive to minor neurodevelopmental abnormalities than the assessment of MND (14). Studies that used intelligence quotient as an outcome measure (3,4,5,9) also did not find an association with moderate hyperbilirubinemia (<342 µmol/l) or bilirubin levels ≥428 µmol/l. However, intelligence quotient is a relatively insensitive measure of cognition (15). Therefore, it is conceivable that bilirubin levels >300 µmol/l are associated with subtle neuromotor and cognitive problems (2,15).
The concept of MND is debated (16). This is reflected by Newman and Klebanoff’s opinion that the finding of MND in children with moderate hyperbilirubinemia is clinically irrelevant (3). The recently introduced categorization of MND into simple and complex forms improved the understanding of MND. It is particularly the complex form that has clinical significance (16,17). MND is affected by the child’s age, social background, and prenatal and perinatal history (17). This may explain the difference in the incidence of complex MND in our previous study on infants at 12 mo of age (2).
The finding that healthy term neonates with bilirubin levels <300 μmol/l at 72–96 h postpartum do not show MND more often than comparison infants is reassuring. This finding corresponds to the actual treatment guidelines, i.e., to start phototherapy for infants with bilirubin levels ≥300 μmol/l at 72 h of postpartum age (1,18).
Children with complex MND mainly showed abnormalities in muscle tone regulation. This may be regarded as a minor form of bilirubin-induced neurologic dysfunction (19). This is compatible with the fact that bilirubin encephalopathy is caused by neuronal injury in subcortical areas, the dendate nucleus of the cerebellum, and various brain stem nuclei (20,21). The increased activity level at 18 mo in the study group children may be a reflection of minor dysfunction in these subcortical circuitries, especially in the networks involving basal ganglia and cerebellum.
The strengths of this study are (i) the assessment of bilirubin levels in all the infants, including comparison infants, at 72–96 h postpartum, (ii) the detailed neurological follow-up until the age of 18 mo, and (iii) the low attrition rate. The main limitation was the difference in perinatal characteristics between the BILI and COMP groups. For instance, the BILI group had a lower gestational age and showed lower birth weights more often than the COMP group. Lower gestational age and low birth weight are not only risk factors for hyperbilirubinemia but also for unfavorable neurodevelopmental outcome. We therefore applied multivariable statistics in all comparisons, including the subgroup analyses, to adjust for the potentially confounding effect of these differences. Another limitation of this study is that the majority of infants had been delivered by cesarean section in a Dutch University Medical Centre, implying that our findings cannot be extrapolated to the general population. The long enrollment period reflects that in the Netherlands, it is uncommon for healthy term infants to stay a couple of days in the hospital. Furthermore, we realize that the measurement of bilirubin levels performed only once at 72–96 h was another drawback because presumably this was not the time point at which the infants bilirubin levels peaked. However, Bhutani et al. (22) reported in a monogram of the bilirubin levels of healthy term and near-term neonates that the peak bilirubin level is nearly reached at 96 h, after which a plateau phase takes place. We did not measure the duration of this phase, but according to the monogram, it remains more or less stable during the first week of life. Nevertheless, we think that it is hazardous to base therapeutic guidelines on one measurement.
In conclusion, our study indicates that moderate hyperbilirubinemia (220–300 μmol/l) in healthy full-term newborns does not result in an increase of MND up to 18 mo of age. Yet bilirubin levels ≥300 μmol/l are associated with increased risk of complex MND, suggesting that these bilirubin levels should not be exceeded. This means that our study supports the current guidelines for the treatment of hyperbilirubinemia in healthy term newborns. However, to determine the possibility of subtle cognitive and behavioral outcomes, proper follow-up at school age is needed.
Methods
Subjects
All subjects were healthy term (≥37 wk) neonates born between September 2002 and March 2007. On Mondays and Tuesdays, parents of neonates born at the University Medical Center Groningen (UMCG) who were scheduled to stay in the hospital for at least 3 d, were asked to participate in the current study. Virtually, all parents asked agreed to participate. We excluded children in case of congenital anomaly, hemolytic disease, sepsis, meningitis, metabolic derangement, or an Apgar score <7 at 5 min. After parental consent, we measured the infant’s total serum bilirubin in the blood sampled at their newborn screening, which is routinely performed at 72–96 h postpartum. If the bilirubin level was ≥220 µmol/l, the infant was enrolled in the group with moderate hyperbilirubinemia (BILI group; n = 35), bilirubin level <220 µmol/l implied inclusion in the comparison group (COMP; n = 70). Furthermore, regional midwives were asked to refer neonates with a bilirubin level ≥220 µmol/l (n = 8). No upper limits for bilirubin level were set for inclusion in the BILI group.
The BILI group consisted of 43 infants ( Table 1 ). We enrolled 35 infants at the UMCG. Eight infants had been referred to our study because of jaundice, four from home and four from a regional hospital. They were included at 72–96 h in order to make it possible to get a blood sample for bilirubin estimation at the puncture of the neonatal screening. The COMP group consisted of 70 infants born at the UMCG.
Most infants were Caucasian; four were of Somalian origin (two BILI and two COMP infants) and one COMP infant was of Chinese origin. Because most infants were included on the basis of extra blood sampling during the screening at 72–96 h postpartum, in the UMCG many of the children were born by cesarean section. By that time, most vaginally born infants delivered in a Dutch hospital have been discharged. All parents gave informed consent, and the procedures were approved by the medical ethics committees of the UMCG and Wilhelmina Hospital, Assen.
Measurements
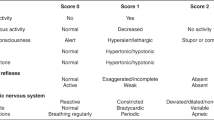
Neurological evaluation consisted of three age-specific neurological assessments. Neonatally (day 3–8), we used Prechtl’s standardized technique (23). Children were classified as definitely abnormal in case of clear neurological syndromes such as marked hypertonia, a hemisyndrome or a hyperexcitability, or apathy syndrome. They were classified as MND when they showed mild abnormalities such as mild deviancies in muscle tone regulation or mild asymmetries in infantile reactions and tendon reflexes. The neonatal neurological assessment was performed by a team of assessors, including the authors, trained in the Prechtl examination (see Acknowledgments). Assessors were masked, but of course in case of evident hyperbilirubinemia, the infants’ color revealed group membership during the neonatal examination.
At 3 mo, we evaluated the neurological condition by means of an assessment of the quality of general movements (24). We made a video recording of 20 min of spontaneous motility in the supine position. These recordings were assessed by M.H.-A. and R.J.L., who were blinded to the study. The quality of movements was classified as normal–optimal and suboptimal (perfectly and acceptably complex, variable and fluent general movements, respectively), mildly abnormal (insufficiently complex and variable movements, which are not fluent), and definitely abnormal (virtual lack of complexity, variation, and fluency). General movements quality can be assessed reliably (κ > 0.80) (25).
When the infants had reached the age of 18 mo, the authors, who were blinded to history and bilirubin level, carried out the standardized, age-specific neurologic examination of Hempel (26). In the Hempel assessment, five domains of function are assessed: fine motor function, gross motor function, posture and muscle tone, reflexes, and visuomotor function. Children were classified as being neurologically normal, having simple MND, having complex MND, or being neurologically abnormal. Simple MND denotes the presence of one deviant domain. It is regarded as a nonoptimal yet normal form of brain function (17). Complex MND means the presence of more than one domain of dysfunction. It represents the clinically relevant form (17,27). Neurologically abnormal implies the presence of a distinct neurological syndrome such as cerebral palsy. Reliability of the Hempel examination is satisfactory (κ 0.62–1.00) (28).
Behavioral evaluation of the newborn consisted of the screening method of Amiel-Tison et al. (29). This test was developed for anesthetists to detect central nervous system depression in newborns. It consists of 20 items scored on a three-point scale. It has a high interobserver reliability. We selected three items, i.e., consolability, alertness, and crying, because abnormal scores of these items (irritability, moderate stupor, and high-pitched crying) are considered to be clinical signs of an elevated bilirubin level (18). At 18 mo, we evaluated behavior by means of a parental questionnaire, the Toddler Behavior Assessment Questionnaire. The Toddler Behavior Assessment Questionnaire consists of 111 items evaluating temperament. The answers were coded on a scale from 1 to 7: 1, never; 2, very rarely; 3, less than half of the time; 4, about half of the time; 5, more than half of the time; 6, almost always; 7, always; NA, not applicable. We calculated scales of temperament: activity level, pleasure level, falling reactivity and soothability, interest, anger, and sadness. The internal consistency reliability estimates of the scales exceed 0.8 (30).
We performed total and direct-reacting bilirubin measurements with a Beckman Coulter Analyzer (Beckman Coulter, Brea, CA) and documented obstetrical and neonatal conditions, including the Clinical Risk Index for Babies score (31) and data on diseases that occurred during the first 18 mo of life on standardized forms.
Data Analyses
Power calculation was based on the prevalence of MND at 12 mo in our previous study (42% in the group with moderate hyperbilirubinemia vs. 10% in the comparison group (2)). It indicated that at least 32 children per group had to be included to achieve a power of 90% (α set at 0.05). Because we assessed MND at the age of 18 mo, and MND is sensitive to change with age, we decided to include more infants. We analyzed differences in background factors with t-test or nonparametric tests when appropriate ( Table 1 ). We evaluated the differences in the rates of neurologic and behavioral problems between the BILI and COMP group with nonparametric tests, such as Fisher exact test and χ2 test. We used logistic or linear regression analysis to evaluate the contribution of possibly confounding factors. We considered variables for which groups differed at a 5% significance level in the univariate analyses as confounding factors. Throughout the analyses, we considered differences with a P value ≤ 0.05 to be statistically significant (two-tailed testing).
Statement of Financial Support
This study was supported by a grant of the J. K. de Cock Stichting, a local private fund aiming to stimulate research at the medical faculty of the University of Groningen, implying that the grant was a university-administered grant.
Disclosure
The authors declare no conflict of interest.
References
Dijk PH, de Vries TW, de Beer JJ ; Dutch Pediatric Association. [Guideline ‘Prevention, diagnosis and treatment of hyperbilirubinemia in the neonate with a gestational age of 35 or more weeks’]. Ned Tijdschr Geneeskd 2009;153:A93.
Soorani-Lunsing I, Woltil HA, Hadders-Algra M . Are moderate degrees of hyperbilirubinemia in healthy term neonates really safe for the brain? Pediatr Res 2001;50:701–5.
Newman TB, Klebanoff MA . Neonatal hyperbilirubinemia and long-term outcome: another look at the Collaborative Perinatal Project. Pediatrics 1993;92:651–7.
Newman TB, Maisels MJ . Does hyperbilirubinemia damage the brain of healthy full-term infants? Clin Perinatol 1990;17:331–58.
Seidman DS, Paz I, Stevenson DK, Laor A, Danon YL, Gale R . Neonatal hyperbilirubinemia and physical and cognitive performance at 17 years of age. Pediatrics 1991;88:828–33.
Sgro M, Campbell D, Barozzino T, Shah V . Acute neurological findings in a national cohort of neonates with severe neonatal hyperbilirubinemia. J Perinatol 2011;31:392–6.
Ebbesen F, Ehrenstein V, Traeger M, Nielsen GL . Neonatal non-hemolytic hyperbilirubinemia: a prevalence study of adult neuropsychiatric disability and cognitive function in 463 male Danish conscripts. Arch Dis Child 2010;95:583–7.
Jangaard KA, Fell DB, Dodds L, Allen AC . Outcomes in a population of healthy term and near-term infants with serum bilirubin levels of >or=325 micromol/L (>or=19 mg/dL) who were born in Nova Scotia, Canada, between 1994 and 2000. Pediatrics 2008;122:119–24.
Newman TB, Liljestrand P, Jeremy RJ, et al.; Jaundice and Infant Feeding Study Team. Outcomes among newborns with total serum bilirubin levels of 25 mg per deciliter or more. N Engl J Med 2006;354:1889–900.
Grimmer I, Berger-Jones K, Bührer C, Brandl U, Obladen M . Late neurological sequelae of non-hemolytic hyperbilirubinemia of healthy term neonates. Acta Paediatr 1999;88:661–3.
Ozmert E, Erdem G, Topçu M, et al. Long-term follow-up of indirect hyperbilirubinemia in full-term Turkish infants. Acta Paediatr 1996;85:1440–4.
Vandborg PK, Hansen BM, Greisen G, Jepsen M, Ebbesen F . Follow-up of neonates with total serum bilirubin levels = 25 mg/dL: a Danish population-based study. Pediatrics 2012;130:61–6.
Heimler R, Sasidharan P . Neurodevelopmental and audiological outcome of healthy term newborns with moderately severe non-haemolytic hyperbilirubinemia. J Paediatr Child Health 2010;46:588–91.
Bouwstra H, Dijck-Brouwer J, Decsi T, et al. Neurologic condition of healthy term infants at 18 months: positive association with venous umbilical DHA status and negative association with umbilical trans-fatty acids. Pediatr Res 2006;60:334–9.
Johnson L, Bhutani VK . The clinical syndrome of bilirubin-induced neurologic dysfunction. Semin Perinatol 2011;35:101–13.
Hadders-Algra M . Examination of the Child with Minor Neurological Dysfunction, 3rd edn. London: Mac Keith Press, 2010:1–168.
Hadders-Algra M . Two distinct forms of minor neurological dysfunction: perspectives emerging from a review of data of the Groningen Perinatal Project. Dev Med Child Neurol 2002;44:561–71.
American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. Clinical practice guideline: management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316.
Shapiro SM . Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND). J Perinatol 2005;25:54–9.
Connolly AM, Volpe JJ . Clinical features of bilirubin encephalopathy. Clin Perinatol 1990;17:371–9.
Turkel SB . Autopsy findings associated with neonatal hyperbilirubinemia. Clin Perinatol 1990;17:381–96.
Bhutani VK, Johnson L, Sivieri EM . Predictive ability of a predischarge hour-specific serum bilirubin for subsequent significant hyperbilirubinemia in healthy term and near-term newborns. Pediatrics 1999;103:6–14.
Prechtl HFR . The Neurological Examination of the Full Term Newborn Infant. Clinics in Developmental Medicine No. 63, 2nd edn. London: Heinemann, 1977:1–68.
Prechtl HF, Einspieler C, Cioni G, Bos AF, Ferrari F, Sontheimer D . An early marker for neurological deficits after perinatal brain lesions. Lancet 1997;349:1361–3.
Hadders-Algra M, Klip-Van den Nieuwendijk A, Martijn A, van Eykern LA . Assessment of general movements: towards a better understanding of a sensitive method to evaluate brain function in young infants. Dev Med Child Neurol 1997;39:88–98.
Hempel MS . Neurological development during toddling age in normal children and children at risk of developmental disorders. Early Hum Dev 1993;34:47–57.
Batstra L, Neeleman J, Hadders-Algra M . The neurology of learning and behavioural problems in pre-adolescent children. Acta Psychiatr Scand 2003;108:92–100.
Hadders-Algra M . The neuromotor examination of the preschool child and its prognostic significance. Ment Retard Dev Disabil Res Rev 2005;11:180–8.
Amiel-Tison C, Barrier G, Shnider SM, Levinson G, Hughes SC, Stefani SJ . A new neurologic and adaptive capacity scoring system for evaluating obstetric medications in full-term newborns. Anesthesiology 1982;56:340–50.
Goldsmith HH . Studying temperament via construction of the Toddler Behavior Assessment Questionnaire. Child Dev 1996;67:218–35.
International Neonatal Network. The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing the performance of neonatal intensive care units. Lancet 1993;342:193–8.
Acknowledgements
We thank the families whose participation made the project possible and Agnes Hornstra, Christa N. van der Veere, and Krijn T. Verbruggen for assistance in the neonatal neurological assessments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lunsing, R., Pardoen, W. & Hadders-Algra, M. Neurodevelopment after moderate hyperbilirubinemia at term. Pediatr Res 73, 655–660 (2013). https://doi.org/10.1038/pr.2013.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.28
This article is cited by
-
Perinatal Factors in Newborn Are Insidious Risk Factors for Childhood Autism Spectrum Disorders: A Population-based Study
Journal of Autism and Developmental Disorders (2022)
-
The effect of hyperbilirubinemia on motor repertoire of infants between 3 and 5 months of age
European Journal of Pediatrics (2022)
-
Long-term neurodevelopmental outcomes of significant neonatal jaundice in Taiwan from 2000–2003: a nationwide, population-based cohort study
Scientific Reports (2020)