Abstract
Hormones regulate all aspects of male reproduction, from sperm production to sexual drive. Although emerging evidence from animal models and small clinical studies in humans clearly point to a role for several hormones in controlling the ejaculatory process, the exact endocrine mechanisms are unclear. Evidence shows that oxytocin is actively involved in regulating orgasm and ejaculation via peripheral, central and spinal mechanisms. Associations between delayed and premature ejaculation with hypothyroidism and hyperthyroidism, respectively, have also been extensively documented. Some models suggest that glucocorticoids are involved in the regulation of the ejaculatory reflex, but corresponding data from human studies are scant. Oestrogens regulate epididymal motility, whereas testosterone can affect the central and peripheral aspects of the ejaculatory process. Overall, the data of the endocrine system in regulating the ejaculatory reflex suggest that widely available endocrine therapies might be effective in treating sexual disorders in these men. Indeed, substantial evidence has documented that treatments of thyroid diseases are able to improve some ejaculatory difficulties.
Key Points
-
Oxytocin is actively involved in regulating orgasm and ejaculation via peripheral, central and spinal mechanisms
-
Peripheral prolactin levels might mirror central serotonergic tone
-
Associations between delayed ejaculation and premature ejaculation with hypothyroidism and hyperthyroidism, respectively, have been extensively documented
-
Animal models suggest that glucocorticoids might be involved in the regulation of the ejaculatory reflex, but data in human are scant
-
The epididymis is a male target for oestrogens that regulate epididymal motility by conditioning the responsiveness of the contractile hormones and local peptides
-
Hypogonadal symptoms and low testosterone levels might reduce the ability to ejaculate, which suggests that androgens have a central and peripheral role in the ejaculation reflex
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Truitt, A. & Coolen, L. M. Identification of a potential ejaculation generator in the spinal cord. Science 297, 1566–1569 (2002).
Carro-Juárez, M. & Rodríguez-Manzo, G. The spinal pattern generator for ejaculation. Brain Res. Rev. 58, 106–120 (2008).
Mouras, H. et al. Brain processing of visual sexual stimuli in healthy men: a functional magnetic resonance imaging study. NeuroImage 20, 855–869 (2003).
Korenman, S. G. in Williams Textbook of Endocrinology, 9th edn (eds Wilson, J. D., Foster, D. W., Kronenberg, H. M. & Larsen, P. R.) 928–930 (Saunders & Co., Philadelphia, 1998).
Giuliano, F. Neurophysiology of erection and ejaculation. J. Sex. Med. 8 (Suppl. 4), 310–315 (2011).
Peeters, M. & Giuliano, F. Central neurophysiology and dopaminergic control of ejaculation. Neurosci. Biobehav. Rev. 32, 438–453 (2008).
de Jong, T. R., Veening, J. G., Waldinger, M. D., Cools, A. R. & Olivier, B. Serotonin and the neurobiology of the ejaculatory threshold. Neurosci. Biobehav. Rev. 30, 893–907 (2006).
Pattij, T., Olivier, B. & Waldinger, M. D. Animal models of ejaculatory behavior. Curr. Pharm. Des. 11, 4069–4077 (2005).
Foreman, M. M., Hall, J. L. & Love, R. L. The role of the 5-HT2 receptor in the regulation of sexual performance of male rats. Life Sci. 45, 1263–1270 (1989).
Waldinger, M. D. The neurobiological approach to premature ejaculation. J. Urol. 168, 2359–2367 (2002).
Bhasin, S. & Basson, R. in Williams Textbook of Endocrinology, 11th edn (eds Larsen, P. R., Kronenberg, H. R., Melmed, S. & Polonsky, K. S.) 707–717 (Saunders & Co., Philadelphia, 2008).
Althof, S. E. et al. International Society for Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation. J. Sex. Med. 7, 2947–2969 (2010).
Rowland, D. et al. Disorders of orgasm and ejaculation in men. J. Sex. Med. 7, 1668–1686 (2010).
Jannini, E. A. & Lenzi, A. Ejaculatory disorders: epidemiology and current approaches to definition, classification and subtyping. World J. Urol. 23, 68–75 (2005).
Jannini, E. A., Gravina, G. L., Maggi, M., Vignozzi, L. & Lenzi, L. in Advances in Sexual Medicine: Drug Discovery Issues (ed. Abdel-Hamid, I. A.) 27–46 (Research Signpost, Kerala, 2009).
Amann, R. P. & Howards, S. S. Daily spermatozoal production and epididymal spermatozoal reserves of the human male. J. Urol. 124, 211–215 (1980).
El-Badawi, A. & Schenk, E. A. The distribution of cholinergic and adrenergic nerves in the mammalian epididymis: a comparative histochemical study. Am. J. Anat. 121, 1–14 (1967).
Nicholson, H. D., Parkinson, T. J. & Lapwood, K. R. Effects of oxytocin and vasopressin on sperm transport from the cauda epididymis in sheep. J. Reprod. Fertil. 117, 299–305 (1999).
Kempinas, W. D. et al. Fertility of rat epididymal sperm after chemically and surgically induced sympathectomy. Biol. Reprod. 59, 897–904 (1998).
Ishunina, T. A. & Swaab, D. F. Vasopressin and oxytocin neurons of the human supraoptic and paraventricular nucleus: size changes in relation to age and sex. J. Clin. Endocrinol. Metab. 84, 4637–4644 (1999).
Thackare, H., Nicholson, H. D. & Whittington, K. Oxytocin: its role in male reproduction and new potential therapeutic uses. Hum. Reprod. Update 12, 437–448 (2006).
Dale, H. H. On some physiological action of ergot. J. Physiol. 34, 163–206 (1906).
Ott, I. & Scott, J. C. The action of infundibulin upon the mammary secretion. Proc. Soc. Exp. Biol. 8, 48–49 (1910).
Debackere, M., Peeters, G. & Tuyittens, N. Reflex release of an oxytocic hormone by stimulation of genital organs in male and female sheep studied by a cross-circulation technique. J. Endocrinol. 22, 321–334 (1961).
Carmichael, M. S. et al. Plasma oxytocin increases in the human sexual response. J. Clin. Endocrinol. Metab. 64, 27–31 (1987).
Carmichael, M. S., Warburton, V. L., Dixen, J. & Davidson, J. M. Relationships among cardiovascular, muscular, and oxytocin responses during human sexual activity. Arch. Sex. Behav. 23, 59–79 (1994).
Murphy, M. R., Seckl, J. R., Burton, S., Checkley, S. A. & Lightman, S. L. Changes in oxytocin and vasopressin secretion during sexual activity in men. J. Clin. Endocrinol. Metab. 65, 738–774 (1987).
Murphy, M. R., Checkley, S. A., Seckl, J. R. & Lightman, S. L. Naloxone inhibits oxytocin release at orgasm in man. J. Clin. Endocrinol. Metab. 71, 1056–1058 (1990).
Ogawa, S., Kudo, S., Kitsunai, Y. & Fukuchi, S. Increase in oxytocin secretion at ejaculation in male. Clin. Endocrinol. 13, 95–97 (1980).
Uckert, S. et al. Oxytocin plasma levels in the systemic and cavernous blood of healthy males during different penile conditions. World J. Urol. 20, 323–326 (2003).
Krüger, T. H. et al. Specificity of the neuroendocrine response to orgasm during sexual arousal in men. J. Endocrinol. 177, 57–64 (2003).
Peeters, G. et al. Release of neurophysin I and oxytocin by stimulation of the genital organs in bulls. J. Endocrinol. 99, 161–171 (1983).
Stoneham, M. D., Everitt, B. J., Hansen, S., Lightman, S. L. & Todd, K. Oxytocin and sexual behavior in the male rat and rabbit. J. Endocrinol. 107, 97–106 (1985).
Veronesi, M. C. et al. Oxytocin, vasopressin, prostaglandin F(2α), luteinizing hormone, testosterone, estrone sulfate, and cortisol plasma concentrations after sexual stimulation in stallions. Theriogenology 73, 460–467 (2010).
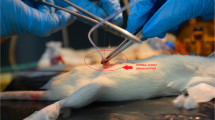
Filippi, S. et al. Role of oxytocin in the ejaculatory process. J. Endocrinol. Invest. 26, 82–86 (2003).
Filippi, S. et al. Identification, localization and functional activity of oxytocin receptors in epididymis. Mol. Cell Endocrinol. 193, 89–100 (2002).
Hib, J. The in vitro effects of oxytocin and vasopressin on spontaneous contractility of the mouse cauda epididymidis. Biol. Reprod. 11, 436–439 (1974).
Hib, J. The 'in vivo' effects of oxytocin and vasopressin on spontaneous contractility of the rat epididymis. Int. J. Fertil. 22, 63–64 (1977).
Fibbi, B. et al. Estrogens regulate humans and rabbit epididymal contractility through the RhoA/Rho-kinase pathway. J. Sex. Med. 6, 2173–2186 (2009).
Maggi, M., Kassis, S., Malozowski, S., Guardabasso, V. & Rodbard, D. Identification and characterization of a vasopressin isoreceptor in porcine seminal vesicles. Proc. Natl Acad. Sci. USA 83, 8824–8828 (1986).
Maggi, M., Kassis, S., Malozowski, S., Guardabasso, V. & Rodbard, D. Identification and characterization of two classes of receptors for oxytocin and vasopressin in porcine tunica albuginea, epididymis, and vas deferens. Endocrinology 120, 986–994 (1987).
Einspanier, A. & Ivell, R. Oxytocin and oxytocin receptor expression in reproductive tissues of the male marmoset monkey. Biol. Reprod. 56, 416–422 (1997).
Frayne, J. & Nicholson, H. D. Localization of oxytocin receptors in the human and macaque monkey male reproductive tracts: evidence for a physiological role of oxytocin in the male. Mol. Hum. Reprod. 4, 527–532 (1998).
Filippi, S. et al. Estrogens, but not androgens, regulate expression and functional activity of oxytocin receptor in rabbit epididymis. Endocrinology 143, 4271–4280 (2002).
Mewe, M., Wulfsen, I., Middendorff, R. & Bauer, C. K. Differential modulation of bovine epididymal activity by oxytocin and noradrenaline. Reproduction 134, 493–501 (2007).
Whittington, K., Assinder, S. J., Parkinson, T., Lapwood, K. R. & Nicholson, H. D. Function and localization of oxytocin receptors in the reproductive tissue of rams. Reproduction 122, 317–325 (2001).
Peri, A. et al. Gene expression of endothelin-1, endothelin-converting enzyme-1, and endothelin receptors in human epididymis. J. Clin. Endocrinol. Metab. 82, 3797–3806 (1997).
Peri, A. et al. Endothelin-1 is synthesized and biologically active in human epididymis via a paracrine mode of action. Steroids 63, 294–298 (1998).
Filippi, S. et al. Oxytocin mediates the estrogen-dependent contractile activity of endothelin-1 in human and rabbit epididymis. Endocrinology 146, 3506–3517 (2005).
Studdard, P. W., Stein, J. L. & Cosentino, M. J. The effects of oxytocin and arginine vasopressin in vitro on epididymal contractility in the rat. Int. J. Androl. 25, 65–71 (2002).
Nicholson, H. D., Parkinson, T. J. & Lapwood, K. R. Effects of oxytocin and vasopressin on sperm transport from the cauda epididymis in sheep. J. Reprod. Fertil. 117, 299–305 (1999).
Vignozzi, L. et al. Regulation of epididymal contractility during semen emission, the first part of the ejaculatory process: a role for estrogen. J. Sex. Med. 5, 2010–2016 (2008).
Melis, M. R., Argiolas, A. & Gessa, G. L. Oxytocin-induced penile erection and yawning: site of action in the brain. Brain Res. 398, 259–265 (1986).
Hughes, A. M., Everitt, B. J., Lightman, S. L. & Todd, K. Oxytocin in the central nervous system and sexual behaviour in male rats. Brain Res. 414, 133–137 (1987).
Arletti, R., Bazzani, C., Castelli, M. & Bertolini, A. Oxytocin improves male copulatory performance in rats. Horm. Behav. 19, 14–20 (1985).
Argiolas, A. et al. Apomorphine stimulation of male copulatory behavior is prevented by the oxytocin antagonist d(CH2)5Tyr(Me)-Orn8-vasotocin in rats. Pharmacol. Biochem. Behav. 33, 81–83 (1988).
Pattij, T. et al. Individual differences in male rat ejaculatory behaviour: searching for models to study ejaculation disorders. Eur. J. Neurosci. 22, 724–734 (2005).
Young, K. A., Gobrogge, K. L., Liu, Y. & Wang, Z. The neurobiology of pair bonding: insights from a socially monogamous rodent. Front. Neuroendocrinol. 32, 53–69 (2011).
Gordon, I., Zagoory-Sharon, O., Leckman, J. F. & Feldman, R. Oxytocin and the development of parenting in humans. Biol. Psychiatr. 68, 377–382 (2010).
Yang, J. et al. Oxytocin in the rat caudate nucleus influences pain modulation. Peptides 32, 2104–2107 (2011).
Yang, J. et al. Oxytocin in the periaqueductal grey regulates nociception in the rat. Regul. Pept. 169, 39–42 (2011).
Yang, J. et al. Oxytocin in the periaqueductal gray participates in pain modulation in the rat by influencing endogenous opiate peptides. Peptides 32, 1255–1261 (2011).
Wagner, C. K. & Clemens, L. G. Projections of the paraventricular nucleus of the hypothalamus to the sexually dimorphic lumbosacral region of the spinal cord. Brain Res. 539, 254–262 (1991).
Ackerman, A. E., Lange, G. M. & Clemens, L. G. Effects of paraventricular lesions on sex behavior and seminal emission in male rats. Physiol. Behav. 63, 49–53 (1997).
Clément, P. et al. Brain oxytocin receptors mediate ejaculation elicited by 7-hydroxy-2-(di-N-propylamino) tetralin (7-OH-DPAT) in anaesthetized rats. Br. J. Pharmacol. 154, 1150–1159 (2008).
de Jong, T. R., Veening, J. G., Olivier, B. & Waldinger, M. D. Oxytocin involvement in SSRI-induced delayed ejaculation: a review of animal studies. J. Sex. Med. 4, 14–28 (2007).
Burri, A., Heinrichs, M., Schedlowski, M. & Kruger, T. H. The acute effects of intranasal oxytocin administration on endocrine and sexual function in males. Psychoneuroendocrinology 33, 591–600 (2008).
Ishak, W. W., Berman, D. S. & Peters, A. Male anorgasmia treated with oxytocin. J. Sex. Med. 5, 1022–1024 (2008).
Guay, A. T., Sabharwal, P., Varma, S. & Malarkey, W. B. Delayed diagnosis of psychological erectile dysfunction because of the presence of macroprolactinemia. J. Clin. Endocrinol. Metab. 81, 2512–2514 (1996).
Fahie-Wilson, M. N., John, R. & Ellis, A. R. Macroprolactin; high molecular mass forms of circulating prolactin. Ann. Clin. Biochem. 42, 175–192 (2005).
Melmed, S. et al. Diagnosis and treatment of hyperprolactinemia: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96, 273–288 (2011).
Bachelot, A. & Binart, N. Reproductive role of prolactin. Reproduction 133, 361–369 (2007).
Bole-Feysot, C., Goffin, V., Edery, M., Binart, N. & Kelly, P. A. Prolactin (PRL) and its receptor: actions, signal transduction pathways and phenotypes observed in PRL receptor knockout mice. Endocr. Rev. 19, 225–268 (1998).
Sobrinho, L. G. Prolactin, psychological stress and environment in humans: adaptation and maladaptation. Pituitary 6, 35–39 (2003).
Ra, S. et al. In vitro contraction of the canine corpus cavernosum penis by direct perfusion with prolactin or growth hormone. J. Urol. 156, 522–525 (1996).
Buvat, J. Hyperprolactinemia and sexual function in men: a short review. Int. J. Impot. Res. 15, 373–377 (2003).
Ciccarelli, A. et al. PRL secreting adenomas in male patients. Pituitary 8, 39–42 (2005).
Corona, G. et al. Effect of hyperprolactinemia in male patients consulting for sexual dysfunction. J. Sex. Med. 4, 1485–1493 (2007).
Corona, G. et al. The impotent couple: low desire. Int. J. Androl. 28 (Suppl. 2), 46–52 (2005).
Corona, G. et al. Psycho-biological correlates of hypoactive sexual desire in patients with erectile dysfunction. Int. J. Impot. Res. 16, 275–281 (2004).
Balercia, G. et al. Sexual symptoms in endocrine diseases: psychosomatic perspectives. Psychother. Psychosom. 76, 134–140 (2007).
Krüger, T. H., Haake, P., Hartmann, U., Schedlowski, M. & Exton, M. S. Orgasm-induced prolactin secretion: feedback control of sexual drive? Neurosci. Biobehav. Rev. 26, 31–44 (2002).
Exton, M. S. et al. Coitus-induced orgasm stimulates prolactin secretion in healthy subjects. Psychoneuroendocrinology 26, 287–294 (2001).
Bancroft, J. The endocrinology of sexual arousal. J. Endocrinol. 186, 411–427 (2005).
Rohn, R. D. Benign galactorrhea/breast discharge in adolescent males probably due to breast self-manipulation. J. Adolesc. Health Care 5, 210–212 (1984).
El-Sakka, A. I., Hassoba, H. M., Sayed, H. M. & Tayeb, K. A. Pattern of endocrinal changes in patients with sexual dysfunction. J. Sex. Med. 2, 551–558 (2005).
Low, M. J. in Williams Textbook of Endocrinology, 11th edn (eds Larsen, P. R., Kronenberg, H. R., Melmed, S. & Polonsky, K. S.) 85–154 (Saunders & Co., Philadelphia, 2008).
Van de Kar, L. D. & Bethea, C. L. Pharmacological evidence that serotonergic stimulation of prolactin secretion is mediated via the dorsal raphe nucleus. Neuroendocrinology 35, 225–230 (1982).
Corona, G. et al. Selective serotonin reuptake inhibitor-induced sexual dysfunction. J. Sex. Med. 6, 1259–1269 (2009).
Giuliano, F. & Hellstrom, W. J. The pharmacological treatment of premature ejaculation. BJU Int. 102, 668–675 (2008).
Kennedy, S. H. & Rizvi, S. Sexual dysfunction, depression, and the impact of antidepressants. J. Clin. Psychopharmacol. 29, 157–164 (2009).
Rosen, R. C., Lane, R. M. & Menza, M. Effects of SSRIs on sexual function: a critical review. J. Clin. Psychopharmacol. 19, 67–85 (1999).
Waldinger, M. D., Hengeveld, M. W. & Zwinderman, A. H. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. Am. J. Psychiatr. 151, 1377–1379 (1994).
Pryor, J. L. et al. Efficacy and tolerability of dapoxetine in treatment of premature ejaculation: an integrated analysis of two double-blind, randomised controlled trials. Lancet 368, 929–937 (2006).
Muldoon, M. F. et al. The metabolic syndrome is associated with reduced central serotonergic responsivity in healthy community volunteers. J. Clin. Endocrinol. Metab. 91, 718–721 (2006).
Muldoon, M. F. et al. Low central nervous system serotonergic responsivity is associated with the metabolic syndrome and physical inactivity. J. Clin. Endocrinol. Metab. 89, 266–271 (2004).
Muldoon, M. F. et al. Lower central serotonergic responsivity is associated with preclinical carotid artery atherosclerosis. Stroke 38, 2228–2223 (2007).
Corona, G. et al. Hypoprolactinemia: a new clinical syndrome in patients with sexual dysfunction. J. Sex. Med. 6, 1457–1466 (2009).
Yatham, L. N. & Steiner, M. Neuroendocrine probes of serotonergic function: a critical review. Life Sci. 53, 447–463 (1993).
Carani, C. et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J. Clin. Endocrinol. Metab. 90, 6472–6479 (2005).
McIntosh, T. K. & Barfield, R. J. Brain monoaminergic control of male reproductive behavior. I. Serotonin and the post-ejaculatory refractory period. Behav. Brain Res. 12, 255–265 (1984).
Sadeghi-Nejad, H. & Watson, R. Premature ejaculation: current medical treatment and new directions (CME). J. Sex. Med. 5, 1037–1050 (2008).
Ballenger, J. C. Current treatments of the anxiety disorders in adults. Biol. Psychiatr. 46, 1579–1594 (1999).
Pergamin-Hight, L., Bakermans-Kranenburg, M. J., van Ijzendoorn, M. H. & Bar-Haim, Y. Variations in the promoter region of the serotonin transporter gene and biased attention for emotional information: a meta-analysis. Biol. Psychiatr. 71, 373–379 (2012).
Corona, G. et al. SIEDY Scale 3, a new instrument to detect psychological component in subjects with erectile dysfunction. J. Sex. Med. http://dx.doi.org/10.1111/j.1743-6109.2012.02762.x.
Corona, G. et al. Autoeroticism, mental health, and organic disturbancies in patients with erectile dysfunction. J. Sex. Med. 7, 182–191 (2010).
Corona, G. et al. Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J. Androl. 27, 453–458 (2006).
Corona, G. et al. Psycho-biological correlates of rapid ejaculation in patients attending an andrologic unit for sexual dysfunctions. Eur. Urol. 46, 615–622 (2004).
Corona, G. et al. Different testosterone levels are associated with ejaculatory dysfunction. J. Sex. Med. 5, 1991–1998 (2008).
Carosa, E. et al. Ontogenetic profile of the expression of thyroid hormone receptors in rat and human corpora cavernosa of the penis. J. Sex. Med. 7, 1381–1390, (2010).
Cihan, A. et al. The relationship between premature ejaculation and hyperthyroidism. J. Urol. 181, 1273–1280 (2009).
Cahangirov, A. et al. Investigation of the neural target level of hyperthyroidism in premature ejaculation in a rat model of pharmacologically induced ejaculation. J. Sex. Med. 8, 90–96 (2011).
Cihan, A. et al. An experimental approach to the interrelationship between hyperthyroidism and ejaculation latency time in male rats. J. Urol. 181, 907–912 (2009).
Oztürk, M. I. et al. Hormonal evaluation in premature ejaculation. Urol. Int. 88, 454–458 (2012).
Waldinger, M. D., Zwinderman, A. H., Olivier, B. & Schweitzer, D. H. Thyroid-stimulating hormone assessments in a Dutch cohort of 620 men with lifelong premature ejaculation without erectile dysfunction. J. Sex. Med. 2, 865–870 (2005).
Corona, G. et al. Age-related changes in general and sexual health in middle-aged and older men: results from the European Male Ageing Study (EMAS). J. Sex. Med. 7, 1362–1380 (2010).
Corona, G. et al. Thyroid hormones and male sexual function. Int. J. Androl. (in press).
Corona, G. et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int. J. Androl. 34, 41–48 (2011).
Kharlip, J. & Cooper, D. S. Recent developments in hyperthyroidism. Lancet 373, 1930–1932 (2009).
Rabb, M. H. et al. Effects of sexual stimulation, with and without ejaculation, on serum concentrations of, LH, FSH, testosterone, cortisol and prolactin in stallions. J. Anim. Sci. 67, 2724–2729 (1989).
Borg, K. E., Esbenshade, K. L. & Johnson, B. H. Cortisol, growth hormone, and testosterone concentrations during mating behavior in the bull and boar. J. Anim. Sci. 69, 3230–3240 (1991).
Bishop, J. D., Malven, P. V., Singleton, W. L. & Weesner, G. D. Hormonal and behavioural correlates of emotional states in sexually trained boars. J. Anim. Sci. 77, 3339–3345 (1999).
Veronesi, M. C. et al. PGF(2α), LH, testosterone, oestrone sulphate, and cortisol plasma concentrations around sexual stimulation in jackass. Theriogenology 75, 1489–1498 (2011).
Wildt, D. E. et al. A comparative analysis of ejaculate and hormonal characteristics of the captive male cheetah, tiger, leopard, and puma. Biol. Reprod. 38, 245–255 (1988).
Brown, J. L. et al. Adrenal-pituitary-gonadal relationships and ejaculate characteristics in captive leopards (Panthera pardus kotiya) isolated on the island of Sri Lanka. J. Reprod. Fertil. 85, 605–613 (1989).
Phoenix, C. H., Dixson, A. F. & Resko, J. A. Effects of ejaculation on levels of testosterone, cortisol, and luteinizing hormone in peripheral plasma of rhesus monkeys. J. Comp. Physiol. Psychol. 91, 120–127 (1977).
Kathleen, C. & Phoenix, C. H. Diurnal patterns of testosterone, dihydrotestosterone, estradiol, and cortisol in serum of rhesus males: relationship to sexual behavior in aging males. Horm. Behav. 15, 416–426 (1981).
Carani, C. et al. The endocrine effects of visual erotic stimuli in normal men. Psychoneuroendocrinology 15, 207–216 (1990).
Krüger, T. et al. Neuroendocrine and cardiovascular response to sexual arousal and orgasm in men. Psychoneuroendocrinology 23, 401–411 (1998).
Exton, N. G. et al. Neuroendocrine response to film-induced sexual arousal in men and women. Psychoneuroendocrinology 25, 187–199 (2000).
Ismail, A. A. A., Davidson, D. W., Loraine, J. A. & Fox, C. A. Relationship between plasma cortisol and human sexual activity. Nature 237, 288–289 (1972).
Valassi, E. et al. The European Registry on Cushing's syndrome: 2-year experience. Baseline demographic and clinical characteristics. Eur. J. Endocrinol. 165, 383–392 (2011).
Granata, A. et al. Sexual dysfunctions in men affected by autoimmune addison's disease before and after short-term gluco- and mineralocorticoid replacement therapy. J. Sex. Med. http://dx.doi.org/10.1111/j.1743-6109.2012.02673.x
Hess, R. A. et al. Estrogens and epididymal function. Reprod. Fertil. Dev. 13, 273–283 (2001).
O'Donnell, L., Robertson, K. M., Jones, M. E. & Simpson, E. R. Estrogen and spermatogenesis. Endocr. Rev. 22, 289–318 (2001).
Pereyra-Martinez, A. C., Roselli, C. E., Stadelman, H. L. & Resko, J. A. Cytochrome P450 aromatase in testis and epididymis of male rhesus monkeys. Endocrine 16, 15–19 (2001).
Wiszniewska, B. Primary culture of the rat epididymal epithelial cells as a source of oestrogen. Andrologia 34, 180–187 (2002).
Carpino, A., Romeo, F. & Rago, V. Aromatase immunolocalization in human ductuli efferentes and proximal ductus epididymis. J. Anat. 204, 217–220 (2004).
Zhou, Q. et al. Localization of androgen and estrogen receptors in adult male mouse reproductive tract. J. Androl. 23, 870–881 (2002).
Hess, R. A. Estrogen in the adult male reproductive tract: a review. Reprod. Biol. Endocr. 1, 52–66 (2003).
Comhaire, F. Treatment of oligospermia with tamoxifen. Intern. J. Fertil. 21, 232–238 (1976).
Rowe, P., Comhaire, F., Hargreave, B. & Mahmoud, A. WHO Manual for the standardized investigation, diagnosis and management of the infertile male (Cambridge University Press, Cambridge, 2000).
Orgebin-Crist, M. C., Eller, B. C. & Danzo, B. J. The effects of estradiol, tamoxifen, and testosterone on the weights and histology of the epididymis and accessory sex organs of sexually immature rabbits. Endocrinology 113, 1703–1715 (1983).
Kotoulas, I. G., Cardamakis, E., Michopoulos, J., Mitropoulos, D. & Dounis, A. Tamoxifen treatment in male infertility. I. Effect on spermatozoa. Fertil. Steril. 61, 911–914 (1994).
Corona, G. & Maggi, M. The role of testosterone in erectile dysfunction. Nat. Rev. Urol. 7, 46–56 (2010).
Morelli, A. et al. Androgens regulate phosphodiesterase type 5 expression and functional activity in corpora cavernosa. Endocrinology 145, 2253–2263 (2004).
Mancina, R. et al. Expression and functional activity of phosphodiesterase type 5 in human and rabbit vas deferens. Mol. Hum. Reprod. 11, 107–115 (2005).
Carosa, E. et al. The ontogenetic expression pattern of type 5 phosphodiesterase correlates with androgen receptor expression in rat corpora cavernosa. J. Sex. Med. 6, 388–396 (2009).
Corona, G. et al. Perceived ejaculate volume reduction in patients with erectile dysfunction: psychobiologic correlates. J. Androl. 32, 333–339 (2011).
Swaab, D. F. Sexual differentiation of the brain and behavior. Best Pract. Res. Clin. Endocrinol. Metab. 21, 431–444 (2007).
Keleta, Y. B., Lumia, A. R., Anderson, G. M. & McGinnis, M. Y. Behavioral effects of pubertal anabolic androgenic steroid exposure in male rats with low serotonin. Brain Res. 1132, 129–138 (2007).
Hart, B. L. Alteration of quantitative aspects of sexual reflexes in spinal male dogs by testosterone. J. Comp. Physiol. Psychol. 66, 726–730 (1968).
Sakamoto, H. et al. Androgen regulates the sexually dimorphic gastrin-releasing peptide system in the lumbar spinal cord that mediates male sexual function. Endocrinology 150, 3672–3679 (2009).
Sakamoto, H. et al. Sexually dimorphic gastrin releasing peptide system in the spinal cord controls male reproductive functions. Nat. Neurosci. 11, 634–636 (2008).
Kicman, A. T. Pharmacology of anabolic steroids. Br. J. Pharmacol. 154, 502–521 (2008).
Carosa, E. et al. Sexual inactivity results in reversible reduction of LH bioavailability. Int. J. Impot. Res. 14, 93–99 (2002).
Waldinger, M. D. & Olivier, B. Animal models of premature and retarded ejaculation. World J. Urol. 23, 115–118 (2005).
Author information
Authors and Affiliations
Contributions
G. Corona, L. Vignozzi, G. Rastrelli and M. Maggi researched the data for the article. G. Corona, E. A. Jannini, L. Vignozzi and M. Maggi contributed substantially to the discussion of the article content. G. Corona and M. Maggi wrote the article. G. Corona, E. A. Jannini, L. Vignozzi and M. Maggi edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Corona, G., Jannini, E., Vignozzi, L. et al. The hormonal control of ejaculation. Nat Rev Urol 9, 508–519 (2012). https://doi.org/10.1038/nrurol.2012.147
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2012.147
This article is cited by
-
Thyroid disorders and male sexual dysfunction
International Journal of Impotence Research (2023)
-
Alterazioni tiroidee nella fecondazione medicalmente assistita
L'Endocrinologo (2023)
-
High incidence of sexual dysfunction and timed intercourse was found only in infertile males who with known impairment of sperm quality for a long period: evidence from a hospital-based cross-sectional study
Reproductive Biology and Endocrinology (2022)
-
No evidence for prolactin’s involvement in the post-ejaculatory refractory period
Communications Biology (2021)
-
Management of premature ejaculation: a clinical guideline from the Italian Society of Andrology and Sexual Medicine (SIAMS)
Journal of Endocrinological Investigation (2021)