Key Points
-
Despite many advances in medicine, phantom limb pain — pain in a no longer existing or deafferented limb — still occurs in 50–80% of all amputees.
-
Pathological neuronal activity in the residual limb or the dorsal root ganglion, which can be enhanced by sympathetic activation, could be one important factor in phantom limb pain.
-
Spinal changes include reorganization of the body map as well as sensitization of spinal transmission neurons.
-
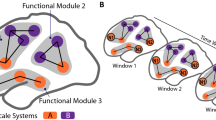
Supraspinal changes seem to be important and might have a special focus in the cortex, where maladaptive map reorganization has been found to be closely related to the magnitude of phantom pain.
-
Similarities of phantom limbs and phantom pain to other abnormal sensory phenomena such as somatosensory and body image-related illusions suggest that frontal and parietal brain regions might be important in the generation of phantom limbs and phantom pain.
-
Previous painful experience could culminate in a pain memory that might have a role in phantom pain and involve both sensory and affective components.
-
Behavioural interventions such as use of a mirror, imagery, sensory discrimination training or use of a myoelectric prosthesis could reduce maladaptive plastic changes and subsequently phantom limb pain; pharmacological interventions and stimulation methods might be similarly effective.
Abstract
Phantom pain refers to pain in a body part that has been amputated or deafferented. It has often been viewed as a type of mental disorder or has been assumed to stem from pathological alterations in the region of the amputation stump. In the past decade, evidence has accumulated that phantom pain might be a phenomenon of the CNS that is related to plastic changes at several levels of the neuraxis and especially the cortex. Here, we discuss the evidence for putative pathophysiological mechanisms with an emphasis on central, and in particular cortical, changes. We cite both animal and human studies and derive suggestions for innovative interventions aimed at alleviating phantom pain.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hunter, J. P., Katz, J. & Davis, K. D. The effect of tactile and visual sensory inputs on phantom limb awareness. Brain 126, 579–589 (2003).
Nikolajsen, L. J. & Jensen, T. S. in Wall and Melzack's Textbook of Pain (eds Koltzenburg, M. & McMahon, S. B.) 961–971 (Elsevier, Amsterdam, 2005). A comprehensive overview of factors that contribute to phantom limbs, and treatment options.
Rothemund, Y., Grüsser, S. M., Liebeskind, U., Schlag, P. M. & Flor, H. Phantom phenomena in mastectomized patients and their relation to chronic and acute pre-mastectomy pain. Pain 107, 140–146 (2004).
Melzack, R. & Loeser, J. D. Phantom body pain in paraplegics: evidence for a 'central pattern generating mechanism' for pain. Pain 4, 195–210 (1978).
Waxman, S. G. & Hains, B. C. Fire and phantoms after spinal cord injury: Na+ channels and central pain. Trends Neurosci. 29, 207–215 (2006). An overview of molecular mechanisms of pain after spinal cord injury.
Hill, A. Phantom limb pain: a review of the literature on attributes and potential mechanisms. J. Pain Symptom Manage. 17, 125–142 (1999).
Houghton, A. D., Nicholls, G., Houghton, A. L., Saadah, E. & McColl, L. Phantom pain: natural history and association with rehabilitation. Ann. R. Coll. Surg. Engl. 76, 22–25 (1994).
Ephraim, P. L., Wegener, S. T., MacKenzie, E. J., Dillingham, T. R. & Pezzin, L. E. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch. Phys. Med. Rehabil. 86, 1910–1919 (2005).
Lacoux, P. A., Crombie, I. K. & Macrae, W. A. Pain in traumatic upper limb amputees in Sierra Leone. Pain 99, 309–312 (2002).
Wilkins, K. L., McGrath, P. J., Finley, G. A. & Katz, J. Phantom limb sensation and phantom limb pain in child and adolescent amputees. Pain 78, 7–12 (1998).
Saadah, E. S. M. & Melzack, R. Phantom limb experiences in congenital limb-deficient adults. Cortex 30, 479–485 (1994).
Sherman, R. A., Arena, J. G., Sherman, C. J. & Ernst, J. L. The mystery of phantom limb pain: growing evidence for psychophysiological mechanisms. Biofeedback Self Regul. 14, 267–280 (1989).
Jensen, T. S., Krebs, B., Nielsen, J. & Rasmussen, P. Immediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain 21, 267–278 (1985).
Yarnitski, D., Barron, S. A. & Bental, E. Disappearance of phantom pain after focal brain infarction. Pain 32, 285–287 (1988).
Jänig, W. & McLachlan, E. On the fate of sympathetic and sensory neurons projecting into a neuroma of the superficial peroneal nerve in the cat. J. Comp. Neurol. 225, 302–311 (1984).
Fried, K., Govrin-Lippman, R., Rosenthal, F., Ellisman, M. H. & Devor, M. Ultrastructure of afferent axon endings in a neuroma. J. Neurocytol. 20, 682–701 (1991).
Wall, P. D. & Gutnick, M. Ongoing activity in peripheral nerves: the physiology and pharmacology of impulses originating from a neuroma. Exp. Neurol. 43, 580–593 (1974).
Devor, M. in Wall and Melzack's Textbook of Pain (eds Koltzenburg, M. & McMahon, S. B.) 905–927 (Elsevier, Amsterdam, 2005).
Devor, M. Sodium channels and mechanisms of neuropathic pain. J. Pain 7, S3–S12 (2006).
Gorodetskaya, N., Constantin, C. & Jänig, W. Ectopic activity in cutaneous regenerating afferent nerve fibers following nerve lesion in the rat. Eur. J. Neurosci. 18, 2487–2497 (2003).
Blumberg, H. & Jänig, W. Activation of fibers via experimentally produced stump neuromas of skin nerves: ephaptic transmission or retrograde sprouting? Exp. Neurol. 76, 468–482 (1982).
Nyström, B. & Hagbarth, K. E. Microelectrode recordings from transected nerves in amputees with phantom limb pain. Neurosci. Lett. 27, 211–216 (1981).
Chen, Y., Michaelis, M., Jänig, W. & Devor, M. Adrenoreceptor subtype mediating sympathetic-sensory coupling in injured sensory neurons. J. Neurophysiol. 76, 3721–3730 (1996).
Katz, J. Psychophysiological contributions to phantom limbs. Can. J. Psychiatry 37, 282–298 (1992). A comprehensive discussion of psychophysiological factors in phantom pain.
Chabal, C., Jacobson, L., Russell, L. C. & Burchiel, K. J. Pain response to perineuromal injection of normal saline, epinephrine, and lidocaine in humans. Pain 49, 9–12 (1992).
Fagius, J., Nordin, M. & Wall, M. Sympathetic nerve activity to amputated lower leg in humans. Evidence of altered skin vasoconstrictor discharge. Pain 98, 37–45 (2002).
Birbaumer, N. et al. Effects of regional anesthesia on phantom limb pain are mirrored in changes in cortical reorganization. J. Neurosci. 17, 5503–5508 (1997).
Baron, R. & Maier, C. Phantom limb pain: are cutaneous nociceptors and spinothalamic neurons involved in the signaling and maintenance of spontaneous and touch-evoked pain? A case report. Pain 60, 223–228.
Schmidt, A. P., Takahashi, M. E. & de Paula Posso, I. Phantom limb pain induced by spinal anesthesia. Clinics 60, 263–264 (2005).
Woolf, C. J. & Salter, M. W. in Wall and Melzack's Textbook of Pain (eds Koltzenburg, M. & McMahon, S. B.) 91–105 (Elsevier, Amsterdam, 2005).
Woolf, C. J. Dissecting out mechanisms responsible for peripheral neuropathic pain: implications for diagnosis and therapy. Life Sci. 74, 2605–1510 (2004).
Moore, K. A. et al. Partial peripheral nerve injury promotes a selective loss of GABAergic inhibition in the superficial dorsal horn of the spinal cord. J. Neurosci. 22, 6724–6731 (2002).
Coull, J. A. et al. BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain. Nature 438, 1017–1021 (2005).
Wang, S. et al. A rat model of unilateral hindpaw burn injury: slowly developing rightwards shift of the morphine dose-response curve. Pain 116, 87–95 (2005).
Wiesenfeld-Hallin, Z, Xu, X. J. & Hökfelt, T. The role of spinal cholecystokinin in chronic pain states. Pharmacol. Toxicol. 91, 398–403 (2002).
Torsney, C. & MacDermott, A. B. Disinhibition opens the gate to pathological pain signaling in superficial neurokinin 1 receptor-expressing neurons in rat spinal cord. J. Neurosci. 26, 1833–1843 (2006).
Ueda, H. Molecular mechanisms of neuropathic pain-phenotypic switch and initiation mechanisms. Pharmacol. Ther. 109, 57–77 (2006).
Devor, M. & Wall, P. D. Reorganisation of spinal cord sensory map after peripheral nerve injury. Nature 276, 75–76 (1978).
Swanson, L. W. Mapping the human brain: past present, and future. Trends Neurosci. 18, 471–474 (1995).
Florence, S. L., Taub, H. B. & Kaas, J. H. Large-scale sprouting of cortical connections after peripheral injury in adult macaque monkeys. Science 282, 1117–1121 (1998).
Davis, K. D. et al. Phantom sensations generated by thalamic microstimulation. Nature 391, 385–387 (1998). In this study phantom sensation was elicited by thalamic stimulation in human amputees.
Jones, E. G. & Pons, T. P. Thalamic and brainstem contributions to large-scale plasticity of primate somatosensory cortex. Science 282, 1121–1125 (1998).
Wu, C. W. & Kaas, J. H. The effects of long-standing limb loss on anatomical reorganization of the somatosensory afferents in the brainstem and spinal cord. Somatosens. Mot. Res. 19, 153–163 (2002).
Kaas, J. H., Florence, S. L. & Jain, N. Subcortical contributions to massive cortical reorganization. Neuron 22, 657–660 (1999).
Jain, N., Florence, S. L., Qi, H. X. & Kaas, J. H. Growth of new brainstem connections in adult monkeys with massive sensory loss. Proc. Natl Acad. Sci. USA 97, 5546–5550 (2000).
Ergenzinger, E. R., Glasier, M. M., Hahm, J. O. & Pons, T. P. Cortically induced thalamic plasticity in the primate somatosensory system. Nature Neurosci. 1, 226–229 (1998).
Kaas, J. H. Is most of neural plasticity in the thalamus cortical? Proc. Natl Acad. Sci. USA 96, 7622–7623 (1999).
Merzenich, M. M. et al. Somatosensory cortical map changes following digit amputation in adult monkeys. J. Comp. Neurol. 224, 591–605 (1984).
Pons, T. P. et al. Massive cortical reorganization after sensory deafferentation in adult macaques. Science 252, 1857–1860 (1991). Revealed massive changes in the cortical map related to dorsal rhizotomies in adult monkeys.
Ramachandran, V. S., Rogers-Ramachandran, D. & Stewart, M. Perceptual correlates of massive cortical reorganization. Science 258, 1159–1160 (1992).
Cronholm, B. Phantom limbs in amputees. A study of changes in the integration of centripetal impulses with special reference to referred sensations. Acta Psychiatr. Neurol. Scand. Suppl. 72, 1–310 (1951).
Halligan, P. W., Marshall, J. C., Wade, D. T., Davey, J. & Morrisson, D. Thumb in cheek? Sensory reorganization and perceptual plasticity after limb amputation. Neuroreport 4, 233–236 (1993).
Grüsser, S. M. et al. Remote activation of referred phantom sensation and cortical reorganization in human upper extremity amputees. Exp. Brain Res. 154, 97–102 (2004).
Grüsser, S. M. et al. The relationship of perceptual phenomena and cortical reorganization in upper extremity amputees. Neuroscience 102, 263–272 (2001).
Halligan, P. W., Marshall, J. C. & Wade, D. T. Sensory disorganization and perceptual plasticity after limb amputation: a follow-up study. Neuroreport 27, 1341–1345 (1994).
Yang, T. T. et al. Sensory maps in the human brain. Nature 368, 592–593 (1994).
Elbert, T. R. et al. Extensive reorganization of the somatosensory cortex in adult humans after nervous system injury. Neuroreport 5, 2593–2597 (1994).
Flor, H. et al. Phantom-limb pain as a perceptual correlate of cortical reorganization following arm amputation. Nature 375, 482–484 (1995). Showed a close association between the magnitude of map changes in the SI cortex and the severity of phantom limb pain.
Flor, H. et al. Cortical reorganization and phantom phenomena in congenital and traumatic upper-extremity amputees. Exp. Brain Res. 119, 205–212 (1998).
Wu, C. W. & Kaas, J. H. Reorganization in primary motor cortex of primates with long-standing therapeutic amputations. J. Neurosci. 19, 7679–7697 (1999).
Cohen, L. G., Bandinelli, S., Findley, T. W. & Hallett, M. Motor reorganization after upper limb amputation in man. A study with focal magnetic stimulation. Brain 114, 615–627 (1991).
Karl, A., Birbaumer, N., Lutzenberger, W., Cohen, L. G. & Flor, H. Reorganization of motor and somatosensory cortex in upper extremity amputees with phantom limb pain. J. Neurosci. 21, 3609–3618 (2001).
Karl, A., Mühlnickel, W., Kurth, R. & Flor, H. Neuroelectric source imaging of steady-state movement-related cortical potentials in human upper extremity amputees with and without phantom limb pain. Pain 110, 90–102 (2004).
Lotze, M., Flor, H., Grodd, W., Larbig, W. & Birbaumer, N. Phantom movements and pain: an fMRI study in upper limb amputees. Brain 124, 2268–2277 (2001).
Spitzer, M., Böhler, P., Weisbrod, M. & Kischka, U. A neural network model of phantom limbs. Biol. Cybern. 72, 197–206 (1995).
Calford, M. B. & Tweedale, R. C-fibres provide a source of masking inhibition to primary somatosensory cortex. Proc. Biol. Sci. 243, 269–275 (1991).
Bowlus, T. H. et al. Comparison of reorganization of the somatosensory system in rats that sustained forelimb removal as neonates and as adults. J. Comp. Neurol. 465, 335–348 (2003).
Churchill, J. D., Muja, N., Myers, W. A., Besheer, J. & Garraghty, P. E. Somatotopic consolidation: a third phase of reorganization after peripheral nerve injury in adult squirrel monkeys. Exp. Brain Res. 118, 189–196 (1998).
Churchill, J. D., Tharp, J. A., Wellman, C. L., Sengelaub, D. R. & Garraghty, P. E. Morphological correlates of injury-induced reorganization in primate somatosensory cortex. BMC Neurosci. 5, 43 (2004).
Kaas, J. H. & Florence, S. L. Mechanisms of reorganization in sensory systems of primates after peripheral nerve injury. Adv. Neurol. 73, 147–158 (1997).
Levy, L. M., Ziemann, U., Chen, R. & Cohen, L. G. Rapid modulation of GABA in sensorimotor cortex induced by acute deafferentation. Ann. Neurol. 52, 755–761 (2005).
Canu, M. H. et al. Concentration of amino acid neurotransmitters in the somatosensory cortex of the rat after surgical or functional deafferentation. Exp. Brain Res. 173, 623–628 (2006).
Larbig, W. et al. Evidence for a change in neural processing after amputation. Pain 67 275–283 (1996).
Karl, A., Diers, M. & Flor, H. P300-amplitudes in upper limb amputees with and without phantom limb pain in a visual oddball paradigm. Pain 110, 40–46 (2004).
Elbert, T. et al. Input-increase and input-decrease types of cortical reorganization after upper extremity amputation in humans. Exp. Brain Res. 117, 161–164 (1997).
Ehrsson, H. H., Spence, C. & Passingham, R. E. That's my hand! Activity in premotor cortex reflects feeling of ownership of a limb. Science 305, 875–877 (2004).
Harris, A. J. Cortical origin of pathological pain. Lancet 354, 1464–1466 (1999).
McCabe, C. S., Haigh, R. C., Halligan, P. W. & Blake, D. R. Simulating sensory-motor incongruence in healthy volunteers: implications for a cortical model of pain. Rheumatology 44, 509–516 (2005).
Moseley, G. L. & Gandevia, S. C. Sensory-motor incongruence and reports of 'pain'. Rheumatology 44, 1083–1085 (2005).
Chen, L. M., Friedman, R. M. & Roe, A. W. Optical imaging of a tactile illusion in area 3b of the primary somatosensory cortex. Science 302, 881–885 (2003).
Katz, J. & Melzack, R. Pain 'memories' in phantom limbs: review and clinical observations. Pain 43, 319–336 (1990). These authors were the first to describe the concept of pain memories in phantom limbs.
Nikolajsen, L., Ilkjaer, S., Kroner, K., Christensen, J. H. & Jensen, T. S. The influence of preamputation pain on postamputation stump and phantom pain. Pain 72, 393–405 (1997).
Flor, H. Phantom-limb pain: characteristics, causes, and treatment. Lancet Neurol. 1, 182–189 (2002).
Flor, H. The functional organization of the brain in chronic pain. Prog. Brain Res. 129, 313–322 (2000).
Flor, H., Braun, C., Elbert, T. & Birbaumer, N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci. Lett. 224, 5–8 (1997).
Soros, P. et al. Functional reorganization of the human primary somatosensory cortex after acute pain demonstrated by magnetoencephalography. Neurosci. Lett. 298, 195–198 (2001).
Kenshalo, D. R. & Willis, W. D. in Pain and the Cerebral Cortex (ed. Peters, A.) 153–212 (Plenum, New York, 1991).
Head, H. & Holmes, G. Sensory disturbances from cerebral lesions. Brain 34, 102–254 (1911).
Appenzeller, O. & Bicknell, J. M. Effects of nervous system lesions on phantom experience in amputees. Neurology 19, 141–146 (1969).
Doetsch, G. S. Perceptual significance of somatosensory cortical reorganization following peripheral denervation. NeuroReport 9, 29–35 (1998).
Hanley, M. A. et al. Preamputation pain and acute pain predict chronic pain after lower extremity amputation. J. Pain (in the press).
Jensen, T. S. & Nikolajsen, L. Pre-emptive analgesia in postamputation pain: an update. Prog Brain Res. 129, 493–503 (2000).
Woolf, C. J. & Chong, M. S. Preemptive analgesia — treating postoperative pain by preventing the establishment of central sensitization. Anesth. Analg. 77, 362–379 (1993).
Nikolajsen, L., Ilkjaer, S., Christensen, J. H., Krøner, K. & Jensen, T. S. Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet 350, 1353–1357 (1997). This controlled study showed no added effect of pre-emptive analgesia for the prevention of phantom limb pain.
Wiech, K. et al. Prevention of phantom limb pain and cortical reorganization in the early phase after amputation in humans. Soc. Neurosci. Abstr. 28, 163.9 (2001).
Nikolajsen, L., Ilkjaer, S. & Jensen, T. S. Relationship between mechanical sensitivity and postamputation pain: a prospective study. Eur. J. Pain 4, 327–334 (2000).
Ruda, M. A., Ling, Q. D., Hohmann, A. G., Peng, Y. B. & Tachibana, T. Altered nociceptive neuronal circuits after neonatal peripheral inflammation. Science 289, 628–631 (2000). Showed that neonatal pain leads to the alteration of nociceptive circuits, therefore supporting the idea of pain memories.
Hermann, C., Hohmeister, J., Demirakca, S., Zohsel, K. & Flor, H. Long-term alteration of sensory perception and pain sensitivity in school-aged children with early pain experiences. Pain (in the press).
Wilder-Smith, O. H. & Arendt-Nielsen, L. Postoperative hyperalgesia: its clinical importance and relevance. Anesthesiology 104, 601–607 (2006).
Rosen, G. et al. Different brain areas activated during imagery of painful and non-painful 'finger movements' in a subject with an amputated arm. Neurocase 7, 255–260 (2001).
Willoch, F. et al. Phantom limb pain in the human brain: unraveling neural circuitries of phantom limb sensations using positron emission tomography. Ann. Neurol. 48, 842–849 (2000).
Wei, F. & Zhuo, M. Potentiation of sensory responses in the anterior cingulate cortex following digit amputation in the anaesthetised rat. J. Physiol. 532, 823–833 (2001).
Recanzone, G. H., Merzenich, M. M., Jenkins, W. M., Grajski, K. A. & Dinse, H. R. Topographic reorganization of the hand representation in cortical area 3b owl monkeys trained in a frequency-discrimination task. J. Neurophysiol. 67, 1031–1056 (1992).
Elbert, T., Pantev, C., Wienbruch, C., Rockstroh, B. & Taub, E. Increased cortical representation of the fingers of the left hand in string players. Science 270, 305–307 (1995).
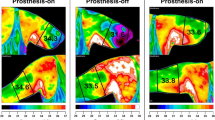
Lotze, M. et al. Does use of a myoelectric prosthesis reduce cortical reorganization and phantom limb pain? Nature Neurosci. 2, 501–502 (1999).
Flor, H., Denke, C., Schaefer, M. & Grüsser, S. Effect of sensory discrimination training on cortical reorganisation and phantom limb pain. Lancet 357, 1763–1764 (2001).
Huse, E., Preissl, H., Larbig, W. & Birbaumer, N. Phantom limb pain. Lancet 358, 1015 (2001).
Giraux, P. & Sirigu, A. Illusory movements of the paralyzed limb restore motor cortex activity. Neuroimage 20, 107–111 (2003).
Ramachandran, V. S. & Rogers-Ramachandran, D. Synesthesia in phantom limbs induced with mirrors. Proc. R. Soc. Lond. B Biol. Sci. 263, 377–386 (1996).
MacLachlan, M., McDonald, D. & Waloch, J. Mirror treatment of lower limb phantom pain: a case study. Disabil. Rehabil. 26, 901–904 (2004).
Moseley, G. L. Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain 114, 54–61 (2005). Showed specific effects on pain related to hand laterality recognition, imagined movement and mirror training in complex regional pain syndrome.
Fregni, F. et al. A sham-controlled, phase II trial of transcranial direct current stimulation for the treatment of central pain in traumatic spinal cord injury. Pain 122, 197–209 (2006).
Ehrsson, H. H., Holmes, N. P. & Passingham, R. E. Touching a rubber hand: feeling of body ownership is associated with activity in multisensory brain areas. J. Neurosci. 25, 10564–10573 (2005).
Fink, G. R. et al. The neural consequences of conflict between intention and the senses. Brain 122, 497–512 (1999).
Craig, A. D. How do you feel? Interoception: the sense of the physiological condition of the body. Nature Rev. Neurosci. 3, 655–666 (2002).
Acknowledgements
This article is dedicated to the memory of T. Pons, whose work inspired many of the findings reported here. This work was supported by the Deutsche Forschungsgemeinschaft, the Bundesministerium für Bildung und Forschung (German Neuropathic Pain Network) and the Lundbeck Foundation, Denmark. The authors would like to thank W. Jänig for helpful comments on an earlier version of this article and M. Lotze for help with the figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Glossary
- Neuroma
-
When a limb is severed, a terminal swelling or 'endbulb' is formed and axonal sprouting occurs. In the case of an amputation, sprouting and endbulb formation lead to a neuroma, a tangled mass that forms when the axons cannot reconnect or can only partially reconnect, as is the case in partial lesions. These neuromas generate abnormal activity that is called ectopic because it does not originate from the nerve endings.
- Dorsal root ganglion
-
A nodule on a dorsal root that contains cell bodies of afferent spinal neurons, which convey somatosensory input to the CNS.
- Paraesthesia
-
An abnormal skin sensation such as tingling or itching.
- Microglia
-
Glial cells are the 'glue' of the nervous system, and support and protect the neurons. Microglia are a special form of small glial cells; they have immune functions and can be involved in inflammatory actions.
- Substance P
-
A neuropeptide that plays an important role in nociception and is released by the primary somatosensory afferents in the spinal cord.
- C-afferents
-
Unmyelinated fibres, 0.4–1.2 μm in diameter, conducting nerve impulses at a velocity of 0.7–2.3 ms−1. They conduct secondary, delayed pain.
- Aδ afferents
-
Thinly myelinated nerve fibres with a conduction velocity of 10–30 ms−1 that convey nociceptive information to the spinal cord. These receptors convey first, sharp, pricking pain and are located mainly on hairy skin.
- Aβ fibres
-
Large-diameter myelinated fibres that have a conduction velocity of ∼40 ms−1 and normally carry non-nociceptive information.
- Myoelectric prosthesis
-
A motor-driven prosthesis that can, for example, be used for grip movements and is operated through the use of electromyographic signals from muscles.
- Complex regional pain syndrome
-
(CRPS). A chronic neuropathic pain syndrome of two types. CRPS1 occurs most often in the arms or legs after a minor or major injury and is accompanied by severe pain, swelling, oedema, sudomotor abnormalities and increased sensitivity to touch. CRPS2 is related to an identified nerve injury.
Rights and permissions
About this article
Cite this article
Flor, H., Nikolajsen, L. & Staehelin Jensen, T. Phantom limb pain: a case of maladaptive CNS plasticity?. Nat Rev Neurosci 7, 873–881 (2006). https://doi.org/10.1038/nrn1991
Issue Date:
DOI: https://doi.org/10.1038/nrn1991
This article is cited by
-
Prevalence, temporal course and risk factors for phantom eye symptoms in uveal melanoma
Eye (2024)
-
A new perspective on positive symptoms: expression of damage or self-defence mechanism of the brain?
Neurological Sciences (2024)
-
Managing acute phantom limb pain with transcutaneous electrical nerve stimulation: a case report
Journal of Medical Case Reports (2023)
-
Integration of proprioception in upper limb prostheses through non-invasive strategies: a review
Journal of NeuroEngineering and Rehabilitation (2023)
-
The medial prefrontal cortex and the cardiac baroreflex activity: physiological and pathological implications
Pflügers Archiv - European Journal of Physiology (2023)