Key Points
-
Cardiac resynchronization therapy (CRT) is widely used to improve cardiac pump function and prolong life in patients with heart failure, but 30–50% do not respond to treatment
-
Appropriate selection of patients, careful positioning of pacing leads, and optimization of resynchronization settings can notably improve response to CRT
-
Patients with left bundle branch block (LBBB), a QRS duration >150 ms, or both, benefit most from CRT; whether mechanical dyssynchrony provides additional useful diagnostic information is disputed
-
Optimal left ventricular lead positions vary considerably between individuals, but scarred regions should be avoided, and selection of a late-activated region is particularly important in patients with non-LBBB morphology
-
The greatest benefit from CRT might come from the optimal placement of one left ventricular pacing lead, rather than the combined effects of pacing at multiple sites
-
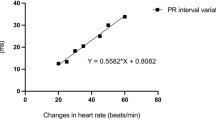
Optimization of atrioventricular and interventricular intervals increases acute haemodynamic response, but the lack of an accurate method to measure synchronization has hampered assessment of long-term effects
Abstract
Cardiac resynchronization therapy (CRT) emerged 2 decades ago as a useful form of device therapy for heart failure associated with abnormal ventricular conduction, indicated by a wide QRS complex. In this Review, we present insights into how to achieve the greatest benefits with this pacemaker therapy. Outcomes from CRT can be improved by appropriate patient selection, careful positioning of right and left ventricular pacing electrodes, and optimal timing of electrode stimulation. Left bundle branch block (LBBB), which can be detected on an electrocardiogram, is the predominant substrate for CRT, and patients with this conduction abnormality yield the most benefit. However, other features, such as QRS morphology, mechanical dyssynchrony, myocardial scarring, and the aetiology of heart failure, might also determine the benefit of CRT. No single left ventricular pacing site suits all patients, but a late-activated site, during either the intrinsic LBBB rhythm or right ventricular pacing, should be selected. Positioning the lead inside a scarred region substantially impairs outcomes. Optimization of stimulation intervals improves cardiac pump function in the short term, but CRT procedures must become easier and more reliable, perhaps with the use of electrocardiographic measures, to improve long-term outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Bakker, P. F. et al. Biventricular pacing in end-stage heart failure improves functional capacity and left ventricular function. J. Interv. Cardiac Electrophysiol. 4, 395–404 (2000).
Vernooy, K. et al. Left bundle branch block induces ventricular remodelling and functional septal hypoperfusion. Eur. Heart. J. 26, 91–98 (2005).
Aiba, T. et al. Electrophysiological consequences of dyssynchronous heart failure and its restoration by resynchronization therapy. Circulation 119, 1220–1230 (2009).
Spragg, D. D. & Kass, D. A. Pathobiology of left ventricular dyssynchrony and resynchronization. Prog. Cardiovasc. Dis. 49, 26–41 (2006).
Van Deursen, C. et al. Left ventricular endocardial pacing improves resynchronization therapy in canine left bundle-branch hearts. Circ. Arrhythm. Electrophysiol. 2, 580–587 (2009).
Strik, M. et al. Transseptal conduction as an important determinant for cardiac resynchronization therapy, as revealed by extensive electrical mapping in the dyssynchronous canine heart. Circ. Arrhythm. Electrophysiol. 6, 682–689 (2013).
Auricchio, A. et al. Effect of pacing chamber and atrioventricular delay on acute systolic function of paced patients with congestive heart failure. Circulation 99, 2993–3001 (1999).
Kass, D. A. et al. Improved left ventricular mechanics from acute VDD pacing in patients with dilated cardiomyopathy and ventricular conduction delay. Circulation 99, 1567–1573 (1999).
Nelson, G. S. et al. Left ventricular or biventricular pacing improves cardiac function at diminished energy cost in patients with dilated cardiomyopathy and left bundle-branch block. Circulation 102, 3053–3059 (2000).
Abraham, W. T. et al. Cardiac resynchronization in chronic heart failure. N. Engl. J. Med. 346, 1845–1853 (2002).
Bristow, M. R. et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. N. Engl. J. Med. 350, 2140–2150 (2004).
Cleland, J. G. et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 352, 1539–1549 (2005).
Abraham, W. T. & Smith, S. A. Devices in the management of advanced, chronic heart failure. Nat. Rev. Cardiol. 10, 98–110 (2013).
St John Sutton, M. et al. Cardiac resynchronization induces major structural and functional reverse remodeling in patients with New York Heart Association class I/II heart failure. Circulation 120, 1858–1865 (2009).
Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 361, 1329–1338 (2009).
Tang, A. S. et al. Cardiac resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 363, 2385–2395 (2010).
Daubert, J. C. et al. 2012 EHRA/HRS expert consensus statement on cardiac resynchronization therapy in heart failure: implant and follow-up recommendations and management. Europace 14, 1236–1286 (2012).
Prinzen, F. W., Hunter, W. C., Wyman, B. T. & McVeigh, E. R. Mapping of regional myocardial strain and work during ventricular pacing: experimental study using magnetic resonance imaging tagging. J. Am. Coll. Cardiol. 33, 1735–1742 (1999).
Ludwig, D. R., Tanaka, H., Friehling, M., Gorcsan, J. 3rd & Schwartzman, D. Further deterioration of LV ejection fraction and mechanical synchrony during RV apical pacing in patients with heart failure and LBBB. J. Cardiovasc. Transl. Res. 6, 425–429 (2013).
Mills, R. W. et al. Left ventricular septal and left ventricular apical pacing chronically maintain cardiac contractile coordination, pump function and efficiency. Circ. Arrhythm. Electrophysiol. 2, 571–579 (2009).
Prinzen, F. W., Vernooy, K., DeBoeck, B. W. & Delhaas, T. Mechano-energetics of the asynchronous and resynchronized heart. Heart Fail. Rev. 16, 215–224 (2011).
Sachse, F. B. et al. Subcellular structures and function of myocytes impaired during heart failure are restored by cardiac resynchronization therapy. Circ. Res. 110, 588–597 (2012).
Kirk, J. A. & Kass, D. A. Electromechanical dyssynchrony and resynchronization of the failing heart. Circ. Res. 113, 765–776 (2013).
Spragg, D. D. et al. Regional alterations in protein expression in the dyssynchronous failing heart. Circulation 108, 929–932 (2003).
van Gelder, B. M., Bracke, F. A., Meijer, A., Lakerveld, L. J. & Pijls, N. H. Effect of optimizing the VV interval on left ventricular contractility in cardiac resynchronization therapy. Am. J. Cardiol. 93, 1500–1503 (2004).
Verbeek, X. et al. Quantification of interventricular asynchrony during LBBB and ventricular pacing. Am. J. Physiol. 283, H1370–H1378 (2002).
Verbeek, X. et al. Intra-ventricular resynchronization for optimal left ventricular function during pacing in experimental left bundle branch block. J. Am. Coll. Cardiol. 42, 558–567 (2003).
Van Geldorp, I. E. et al. Comparison of a non-invasive arterial pulse contour technique and echo Doppler aorta velocity-time-integral on stroke volume changes in optimization of CRT. Europace 13, 87–95 (2011).
Dekker, A. L. et al. Epicardial left ventricular lead placement for cardiac resynchronization therapy: optimal pace site selection with pressure-volume loops. J. Thorac. Cardiovasc. Surg. 127, 1641–1647 (2004).
Duckett, S. G. et al. Invasive acute hemodynamic response to guide left ventricular lead implantation predicts chronic remodeling in patients undergoing cardiac resynchronization therapy. J. Am. Coll. Cardiol. 58, 1128–1136 (2011).
De Boeck, B. W. et al. Septal rebound stretch reflects the functional substrate to cardiac resynchronization therapy and predicts volumetric and neurohormonal response. Eur. J. Heart Fail. 11, 863–871 (2009).
Vernooy, K. et al. Cardiac resynchronization therapy cures dyssynchronopathy in canine left bundle-branch block hearts. Eur. Heart J. 28, 2148–2155 (2007).
Yu, C. M. et al. Tissue Doppler echocardiographic evidence of reverse remodeling and improved synchronicity by simultaneously delaying regional contraction after biventricular pacing therapy in heart failure. Circulation 105, 438–445 (2002).
Chakir, K. et al. Mechanisms of enhanced beta-adrenergic reserve from cardiac resynchronization therapy. Circulation 119, 1231–1240 (2009).
Delnoy, P. P. et al. Sustained benefit of cardiac resynchronization therapy. J. Cardiovasc. Electrophysiol. 18, 298–302 (2007).
Linde, C. et al. Long-term impact of cardiac resynchronization therapy in mild heart failure: 5-year results from the REsynchronization reVErses Remodeling in Systolic left vEntricular dysfunction (REVERSE) study. Eur. Heart J. 34, 2592–2599 (2013).
Stellbrink, C. et al. Impact of cardiac resynchronization therapy using hemodynamically optimized pacing on left ventricular remodeling in patients with congestive heart failure and ventricular conduction disturbances. J. Am. Coll. Cardiol. 38, 1957–1965 (2001).
Bogaard, M. D. et al. Baseline left ventricular dP/dtmax rather than the acute improvement in dP/dtmax predicts clinical outcome in patients with cardiac resynchronization therapy. Eur. J. Heart Fail. 13, 1126–1132 (2011).
Auricchio, A. & Prinzen, F. W. Non-responders to cardiac resynchronization therapy: the magnitude of the problem and the issues. Circ. J. 75, 521–527 (2011).
Ruschitzka, M. et al. Cardiac-resynchronization therapy in heart failure with a narrow QRS complex. N. Engl. J. Med. 369, 1395–1405 (2013).
Hsu, J. C. et al. Predictors of super-response to cardiac resynchronization therapy and associated improvement in clinical outcome: the MADIT-CRT (multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy) study. J. Am. Coll. Cardiol. 59, 2366–2373 (2012).
Brignole, M. et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 15, 1070–1118 (2013).
Zareba, W. et al. Effectiveness of cardiac resynchronization therapy by QRS morphology in the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT). Circulation 123, 1061–1072 (2011).
Hara, H. et al. The relationship of QRS morphology and mechanical dyssynchrony to long-term outcome following cardiac resynchronization therapy. Eur. Heart J. 33, 2680–2691 (2012).
Kandala, J. et al. QRS morphology, left ventricular lead location, and clinical outcome in patients receiving cardiac resynchronization therapy. Eur. Heart J. 34, 2252–2262 (2013).
Prinzen, F. W., Vernooy, K. & Auricchio, A. Cardiac resynchronization therapy: state-of-the-art of current applications, guidelines, ongoing trials and areas of controversy. Circulation 128, 2407–2418 (2013).
Surawicz, B. et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 119, e235–e240 (2009).
Luna, A. B. in The ESC Textbook of Cardiovascular Medicine 1st edn (ed. Camm, A. J.) 1–35 (Blackwell Publishing, 2006).
Strauss, D. G., Selvester, R. H. & Wagner, G. S. Defining left bundle branch block in the era of cardiac resynchronization therapy. Am. J. Cardiol. 107, 927–934 (2011).
Risum, N. et al. Left bundle-branch block: the relationship between electrocardiogram electrical activation and echocardiography mechanical contraction. Am. Heart J. 166, 340–348 (2013).
Galeotti, L., van Dam, P. M., Loring, Z., Chan, D. & Strauss, D. G. Evaluating strict and conventional left bundle branch block criteria using electrocardiographic simulations. Europace 15, 1816–1821 (2013).
Tian, Y. et al. True complete left bundle branch block morphology strongly predicts good response to cardiac resynchronization therapy. Europace 15, 1499–1506 (2013).
Mascioli, G. et al. Electrocardiographic criteria of true left bundle branch block: a simple sign to predict a better clinical and instrumental response to CRT. Pacing Clin. Electrophysiol. 35, 927–934 (2012).
Gorcsan, J. et al. Echocardiography for cardiac resynchronization therapy: recommendations for performance and reporting—a report from the American Society of Echocardiography Dyssynchrony Writing Group endorsed by the Heart Rhythm Society. J. Am. Soc. Echocardiogr. 21, 191–213 (2008).
Chung, E. S. et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 117, 2608–2616 (2008).
Seo, Y. et al. The role of echocardiography in predicting responders to cardiac resynchronization therapy: results from the Japan Cardiac Resynchronization therapy registry Trial (J-CRT). Circ. J. 75, 1156–1163 (2011).
Marwick, T. H. Hype and hope in the use of echocardiography for selection for cardiac resynchronization therapy: the Tower of Babel revisited. Circulation 117, 2573–2576 (2008).
Miyazaki, C. et al. Strain dyssynchrony index correlates with improvement in left ventricular volume after cardiac resynchronization therapy better than tissue velocity dyssynchrony indexes. Circ. Cardiovasc. Imaging 1, 14–22 (2008).
De Boeck, B. W. L. et al. Practical and conceptual limitations of tissue Doppler imaging to predict reverse remodelling in cardiac resynchronisation therapy. Eur. J. Heart Fail. 10, 281–290 (2008).
Miyazaki, C. et al. Comparison of echocardiographic dyssynchrony assessment by tissue velocity and strain imaging in subjects with or without systolic dysfunction and with or without left bundle-branch block. Circulation 117, 2617–2625 (2008).
Zhang, Q. et al. Impact of a dedicated training program on the reproducibility of systolic dyssynchrony measures using tissue Doppler imaging. J. Am. Soc. Echocardiogr. 25, 210–217 (2012).
Gorcsan, J. et al. Relationship of echocardiographic dyssynchrony to long-term survival after cardiac resynchronization therapy. Circulation 122, 1910–1918 (2010).
Beshai, J. F., Grimm, R. A., Nagueh, S. F. et al., Cardiac-resynchronization therapy in heart failure with narrow QRS complexes. N. Engl. J. Med. 357, 2461–2471 (2007).
Lumens, J. et al. Mechanistic evaluation of echocardiographic dyssynchrony indices: patient data combined with multiscale computer simulations. Circ. Cardiovasc. Imaging 5, 491–499 (2012).
Bilchick, K. C. et al. Cardiac magnetic resonance assessment of dyssynchrony and myocardial scar predicts function class improvement following cardiac resynchronization therapy. JACC Cardiovasc. Imaging 1, 561–568 (2008).
Kirn, B. et al. Mechanical discoordination rather than dyssynchrony predicts reverse remodeling upon cardiac resynchronization. Am. J. Physiol. 295, H640–H646. (2008).
Bilchick, K. C. et al. Impact of mechanical activation, scar, and electrical timing on cardiac resynchronization therapy response and clinical outcomes. J. Am. Coll. Cardiol. 63, 1657–1666 (2014).
St John Sutton, M. G. et al. Effect of cardiac resynchronization therapy on left ventricular size and function in chronic heart failure. Circulation 107, 1985–1990 (2003).
Adelstein, E. C. & Saba, S. Scar burden by myocardial perfusion imaging predicts echocardiographic response to cardiac resynchronization therapy in ischemic cardiomyopathy. Am. Heart J. 153, 105–112 (2007).
Ypenburg, C. et al. Effect of total scar burden on contrast-enhanced magnetic resonance imaging on response to cardiac resynchronization therapy. Am. J. Cardiol. 99, 657–660 (2007).
Chalil, S. et al. Late gadolinium enhancement-cardiovascular magnetic resonance as a predictor of response to cardiac resynchronization therapy in patients with ischaemic cardiomyopathy. Europace 9, 1031–1037 (2007).
Rademakers, L. et al. Myocardial infarction does not preclude electrical and hemodynamic benefits of CRT in dyssynchronous canine hearts. Circ. Arrhythm. Electrophysiol. 3, 361–368 (2010).
Knappe, D. et al. Dyssynchrony, contractile function, and response to cardiac resynchronization therapy. Circ. Heart Fail. 4, 433–440 (2011).
Aggarwal, N. R., Martinez, M. W., Gersh, B. J. & Chareonthaitawee, P. Role of cardiac MRI and nuclear imaging in cardiac resynchronization therapy. Nat. Rev. Cardiol. 6, 759–770 (2009).
Ypenburg, C. et al. Impact of viability and scar tissue on response to cardiac resynchronization therapy in ischaemic heart failure patients. Eur. Heart J. 28, 33–41 (2007).
Bleeker, G. B. et al. Effect of posterolateral scar tissue on clinical and echocardiographic improvement after cardiac resynchronization therapy. Circulation 113, 969–976 (2006).
Chalil, S. et al. Effect of posterolateral left ventricular scar on mortality and morbidity following cardiac resynchronization therapy. Pacing Clin. Electrophysiol. 30, 1201–1209 (2007).
Khan, F. Z. et al. Targeted left ventricular lead placement to guide cardiac resynchronization therapy: the TARGET study: a randomized, controlled trial. J. Am. Coll. Cardiol. 59, 1509–1518 (2012).
Leyva, F. et al. Cardiac resynchronization therapy guided by late gadolinium-enhancement cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 13, 29 (2011).
Singh, J. P. et al. Left ventricular lead position and clinical outcome in the multicenter automatic defibrillator implantation trial-cardiac resynchronization therapy (MADIT-CRT) trial. Circulation 123, 1159–1166 (2011).
Gold, M. R. et al. Comparison of stimulation sites within left ventricular veins on the acute hemodynamic effects of cardiac resynchronization therapy. Heart Rhythm 2, 376–381 (2005).
Foley, P. W. et al. Fluoroscopic left ventricular lead position and the long-term clinical outcome of cardiac resynchronization therapy. Pacing Clin. Electrophysiol. 34, 785–797 (2011).
Saxon, L. A. et al. Influence of left ventricular lead location on outcomes in the COMPANION study. J. Cardiovasc. Electrophysiol. 20, 764–768 (2009).
Butter, C. et al. Effect of resynchronization therapy stimulation site on the systolic function of heart failure patients. Circulation 104, 3026–3029 (2001).
Ansalone, G. et al. Doppler myocardial imaging to evaluate the effectiveness of pacing sites in patients receiving biventricular pacing. J. Am. Coll. Cardiol. 39, 489–499 (2002).
Ypenburg, C. et al. Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J. Am. Coll. Cardiol. 52, 1402–1409 (2008).
Derval, N. et al. Optimizing hemodynamics in heart failure patients by systematic screening of left ventricular pacing sites: the lateral left ventricular wall and the coronary sinus are rarely the best sites. J. Am. Coll. Cardiol. 55, 566–575 (2010).
Helm, R. H. et al. Three-dimensional mapping of optimal left ventricular pacing site for cardiac resynchronization. Circulation 115, 953–961 (2007).
Fung, J. W. et al. Variable left ventricular activation pattern in patients with heart failure and left bundle branch block. Heart 90, 17–19 (2004).
Lambiase, P. D. et al. Non-contact left ventricular endocardial mapping in cardiac resynchronisation therapy. Heart 90, 44–51 (2004).
Rodriguez, L. M., Timmermans, C., Nabar, A., Beatty, G. & Wellens, H. J. Variable patterns of septal activation in patients with left bundle branch block and heart failure. J. Cardiovasc. Electrophysiol. 14, 135–141 (2003).
Ploux, S. et al. Acute electrical and hemodynamic effects of multi-left ventricular pacing for cardiac resynchronization therapy in the dyssynchronous canine heart. Heart Rhythm 11, 119–125 (2014).
Lumens, J. et al. Comparative electromechanical and hemodynamic effects of left ventricular and biventricular pacing in dyssynchronous heart failure: electrical resynchronization versus left-right ventricular interaction. J. Am. Coll. Cardiol. 62, 2395–2403 (2013).
Becker, M. et al. Impact of left ventricular lead position in cardiac resynchronization therapy on left ventricular remodelling. A circumferential strain analysis based on 2D echocardiography. Eur. Heart J. 28, 1211–1220 (2007).
Becker, M. et al. Analysis of LV lead position in cardiac resynchronization therapy using different imaging modalities. JACC Cardiovasc. Imaging 3, 472–481 (2010).
Saba, S. et al. Echocardiography-guided left ventricular lead placement for cardiac resynchronization therapy: results of the Speckle Tracking Assisted Resynchronization Therapy for Electrode Region trial. Circ. Heart Fail. 6, 427–434 (2013).
Marek, J. J. et al. Usefulness of echocardiographically guided left ventricular lead placement for cardiac resynchronization therapy in patients with intermediate QRS width and non-left bundle branch block morphology. Am. J. Cardiol. 113, 107–116 (2014).
Gold, M. R. et al. The relationship between ventricular electrical delay and left ventricular remodelling with cardiac resynchronization therapy. Eur. Heart J. 32, 2516–2524 (2011).
Singh, J. P. et al. Left ventricular lead electrical delay predicts response to cardiac resynchronization therapy. Heart Rhythm 3, 1385–1392 (2006).
Ellenbogen, K. A. et al. Primary results from the SmartDelay determined AV optimization: a comparison to other AV delay methods used in cardiac resynchronization therapy (SMART-AV) trial: a randomized trial comparing empirical, echocardiography-guided, and algorithmic atrioventricular delay programming in cardiac resynchronization therapy. Circulation 122, 2660–2668 (2010).
Bongiorni, M. G. et al. Preferred tools and techniques for implantation of cardiac electronic devices in Europe: results of the European Heart Rhythm Association survey. Europace 15, 1664–1668 (2013).
Ghani, A. et al. Assessment of left ventricular dyssynchrony in pacing-induced left bundle branch block compared with intrinsic left bundle branch block. Europace 13, 1504–1507 (2011).
Varma, N. J. Left ventricular conduction delays induced by right ventricular apical pacing: effect of left ventricular dysfunction and bundle branch block. Cardiovasc. Electrophysiol. 19, 114–122 (2008).
Friehling, M. et al. Deterioration of left ventricular ejection fraction and contraction synchrony during right ventricular pacing in patients with left bundle branch block. J. Nucl. Cardiol. 20, 830–834 (2013).
van Gelder, B. M., Meijer, A. & Bracke, F. A. Timing of the left ventricular electrogram and acute hemodynamic changes during implant of cardiac resynchronization therapy devices. Pacing Clin. Electrophysiol. 32 (Suppl. 1), S94–S97 (2009).
Bordachar, P. et al. Biventricular pacing and left ventricular pacing in heart failure: similar hemodynamic improvement despite marked electromechanical differences. J. Cardiovasc. Electrophysiol. 15, 1342–1347 (2004).
Blanc, J. J., Bertault-Valls, V., Fatemi, M., Gilard, M., Pennec, P. Y. & Etienne, Y. Midterm benefits of left univentricular pacing in patients with congestive heart failure. Circulation 109, 1741–1744 (2003).
Thibault, B. et al. Left ventricular versus simultaneous biventricular pacing in patients with heart failure and a QRS complex ≥120 milliseconds. Circulation 124, 2874–2881 (2011).
Pappone, C. et al. Cardiac pacing in heart failure patients with left bundle branch block: impact of pacing site for optimizing left ventricular resynchronization. Ital. Heart J. 1, 464–469 (2000).
Leclercq, C. et al. A randomized comparison of triple-site versus dual-site ventricular stimulation in patients with congestive heart failure. J. Am. Coll. Cardiol. 51, 1455–1462 (2008).
Thibault, B. et al. Acute haemodynamic comparison of multisite and biventricular pacing with a quadripolar left ventricular lead. Europace 15, 984–991 (2013).
Shetty, A. K. et al. The acute hemodynamic response to LV pacing within individual branches of the coronary sinus using a quadripolar lead. Pacing Clin. Electrophysiol. 35, 196–203 (2012).
Bordachar, P. et al. Left ventricular endocardial or triventricular pacing to optimize cardiac resynchronization therapy in a chronic canine model of ischemic heart failure. Am. J. Physiol. Heart Circ. Physiol. 303, H207–H215 (2012).
Strik, M. et al. Endocardial left ventricular pacing improves cardiac resynchronization therapy in chronic asynchronous infarction and heart failure models. Circ. Arrhythm. Electrophysiol. 5, 191–200 (2012).
Spragg, D. D. et al. Optimal left ventricular endocardial pacing sites for cardiac resynchronization therapy in patients with ischemic cardiomyopathy. J. Am. Coll. Cardiol. 56, 774–781 (2010).
Ginks, M. R. et al. Benefits of endocardial and multi-site pacing are dependent on the type of lv electrical activation pattern and presence of ischemic heart disease: insights from electro-anatomical mapping. Circ. Arrhythm. Electrophysiol. 5, 889–897 (2012).
Garrigue, S. et al. Comparison of chronic biventricular pacing between epicardial and endocardial left ventricular stimulation using Doppler tissue imaging in patients with heart failure. Am. J. Cardiol. 88, 858–862 (2001).
van Gelder, B. M., Houthuizen, P. & Bracke, F. A. Transseptal left ventricular endocardial pacing: preliminary experience from a femoral approach with subclavian pull-through. Europace 13, 1454–1458 (2011).
Jais, P. et al. Mid-term follow-up of endocardial biventricular pacing. Pacing Clin. Electrophysiol. 23, 1744–1747 (2000).
Elencwajg, B. et al. The Jurdham procedure: endocardial left ventricular lead insertion via a femoral transseptal sheath for cardiac resynchronization therapy pectoral device implantation. Heart Rhythm 9, 1798–1804 (2012).
Rademakers, L. M., van Gelder, B. M., Scheffer, M. G. & Bracke, F. A. Mid-term follow up of thromboembolic complications in left ventricular endocardial cardiac resynchronization therapy. Heart Rhythm 11, 609–613 (2014).
Kassai, I., Mihalcz, A., Foldesi, C., Kardos, A. & Szili-Torok, T. A novel approach for endocardial resynchronization therapy: initial experience with transapical implantation of the left ventricular lead. Heart Surg. Forum. 12, E137–E140 (2009).
Echt, D. S., Cowan, M. W., Riley, R. E. & Brisken, A. F. Feasibility and safety of a novel technology for pacing without leads. Heart Rhythm 3, 1202–1206 (2006).
Durrer, D. et al. Total excitation of the isolated human heart. Circulation 41, 899–912 (1970).
Narula, O. S. Longitudinal dissociation in the His bundle: bundle branch block due to asynchronous conduction within the His bundle in man. Circulation 56, 996–1006 (1977).
Dabrowski, P., Kleinrok, A., Kozluk, E. & Opolski, G. Physiologic resynchronization therapy: a case of his bundle pacing reversing physiologic conduction in a patient with CHF and LBBB during 2 years of observation. J. Cardiovasc. Electrophysiol. 22, 813–817 (2011).
Barba-Pichardo, R. et al. Ventricular resynchronization therapy by direct His-bundle pacing using an internal cardioverter defibrillator. Europace 15, 83–88 (2013).
Gasparini, M. et al. Long-term survival in patients undergoing cardiac resynchronization therapy: the importance of performing atrio-ventricular junction ablation in patients with permanent atrial fibrillation. Eur. Heart. J. 29, 1644–1652 (2008).
Wilton, S. B., Leung, A. A., Ghali, W. A., Faris, P. & Exner, D. V. Outcomes of cardiac resynchronization therapy in patients with versus those without atrial fibrillation: a systematic review and meta-analysis. Heart Rhythm 8, 1088–1094 (2011).
Koplan, B. A. et al. Heart failure decompensation and all-cause mortality in relation to percent biventricular pacing in patients with heart failure: is a goal of 100% biventricular pacing necessary? J. Am. Coll. Cardiol. 53, 355–360 (2009).
Hayes, D. L. et al. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm 8, 1469–1475 (2011).
Sawhney, N. S. et al. Randomized prospective trial of atrioventricular delay programming for cardiac resynchronization therapy. Heart Rhythm 1, 562–567 (2004).
Whinnett, Z. I. et al. Haemodynamic effects of changes in atrioventricular and interventricular delay in cardiac resynchronisation therapy show a consistent pattern: analysis of shape, magnitude and relative importance of atrioventricular and interventricular delay. Heart 92, 1628–1634 (2006).
Morales, M. A., Startari, U., Panchetti, L., Rossi, A. & Piacenti, M. Atrioventricular delay optimization by Doppler-derived left ventricular dP/dt improves 6-month outcome of resynchronized patients. Pacing Clin. Electrophysiol. 29, 564–568 (2006).
Mullens, W. et al. Insights from a cardiac resynchronization optimization clinic as part of a heart failure disease management program. J. Am. Coll. Cardiol. 53, 765–773 (2009).
Sohaib, S. M. et al. Cardiac resynchronisation therapy optimisation strategies: systematic classification, detailed analysis, minimum standards and a roadmap for development and testing. Int. J. Cardiol. 170, 118–131 (2013).
Kedia, N. et al. Usefulness of atrioventricular delay optimization using Doppler assessment of mitral inflow in patients undergoing cardiac resynchronization therapy. Am. J. Cardiol. 98, 780–785 (2006).
Porciani, C. M. et al. Echo/Doppler-derived time intervals are able to predict left ventricular reverse remodeling after cardiac resynchronization therapy. J. Cardiovasc. Med. (Hagerstown) 11, 157–163 (2010).
Whinnett, Z. I. et al. Determination of optimal atrioventricular delay for cardiac resynchronization therapy using acute non-invasive blood pressure. Europace 8, 358–366 (2006).
Butter, C. et al. Cardiac resynchronization therapy optimization by finger plethysmography. Heart Rhythm 1, 568–575 (2004).
Jansen, A. H. et al. Correlation of echo-Doppler optimization of atrioventricular delay in cardiac resynchronization therapy with invasive hemodynamics in patients with heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am. J. Cardiol. 97, 552–557 (2006).
de Roest, G. J. et al. Prediction of long-term outcome of cardiac resynchronization therapy by acute pressure-volume loop measurements. Eur. J. Heart Fail. 15, 299–307 (2013).
Kyriacou, A. et al. Fully automatable, reproducible, noninvasive simple plethysmographic optimization: proof of concept and potential for implantability. Pacing Clin. Electrophysiol. 35, 948–960 (2012).
Pabari, P. A. et al. When is an optimization not an optimization? Evaluation of clinical implications of information content (signal-to-noise ratio) in optimization of cardiac resynchronization therapy, and how to measure and maximize it. Heart Fail. Rev. 16, 277–290 (2011).
Francis, D. P. Precision of a parabolic optimum calculated from noisy biological data, and implications for quantitative optimization of biventricular pacemakers (cardiac resynchronization therapy). Appl. Math. 2, 1497–1506 (2011).
Francis, D. P. How to reliably deliver narrow individual-patient error bars for optimization of pacemaker AV or VV delay using a “pick-the-highest” strategy with haemodynamic measurements. Int. J. Cardiol. 163, 221–225 (2013).
Martin, D. O. et al. Investigation of a novel algorithm for synchronized left-ventricular pacing and ambulatory optimization of cardiac resynchronization therapy: results of the adaptive CRT trial. Heart Rhythm 9, 1807–1814 (2012).
Boriani, G. et al. A prospective randomized evaluation of VV delay optimization in CRT-D recipients: echocardiographic observations from the RHYTHM II ICD study. Pacing Clin. Electrophysiol. 32 (Suppl. 1), S120–S125 (2009).
Strik, M. et al. Interplay of electrical wavefronts as determinant of the response to cardiac resynchronization therapy in dyssynchronous canine hearts. Circ. Arrhythm. Electrophysiol. 6, 924–931 (2013).
Vernooy, K. et al. Calculation of effective VV-interval facilitates optimization of AV-delay and VV-interval in cardiac resynchronization therapy. Heart Rhythm 4, 75–82 (2007).
Birnie, D. et al. Clinical outcomes with synchronized left ventricular pacing: analysis of the adaptive CRT trial. Heart Rhythm 10, 1368–1374 (2013).
Van Deursen, C. J. et al. Vectorcardiography as a tool for easy optimization of cardiac resynchronization in canine LBBB hearts. Circ. Arrhythm. Electrophysiol. 5, 544–552 (2012).
Abraham, W. T. et al. Results from the FREEDOM trial—assess the safety and efficacy of frequent optimization of cardiac resynchronization therapy. Presented at the Heart Rhythm 31st Annual Scientific Sessions.
van Gelder, B. M., Meijer, A. & Bracke, F. A. The optimized V-V interval determined by interventricular conduction times versus invasive measurement by LVdP/dtmax . J. Cardiovasc. Electrophysiol. 19, 939–944 (2008).
Porciani, M. C. et al. Discordant electrical and mechanical atrial delays affect intracavitary electrogram-based cardiac resynchronization therapy optimization. Europace 14, 593–598 (2012).
Ritter, P. et al. A randomized pilot study of optimization of cardiac resynchronization therapy in sinus rhythm patients using a peak endocardial acceleration sensor vs. standard methods. Europace 14, 1324–1333 (2012).
Altman, R. K. et al. Multidisciplinary care of patients receiving cardiac resynchronization therapy is associated with improved clinical outcomes. Eur. Heart J. 33, 2181–2188 (2012).
Kutyifa, V. et al. Dyssynchrony and the risk of ventricular arrhythmias. JACC Cardiovasc. Imaging 6, 432–444 (2013).
Cowie, M. R. et al. Development and validation of an integrated diagnostic algorithm derived from parameters monitored in implantable devices for identifying patients at risk for heart failure hospitalization in an ambulatory setting. Eur. Heart J. 34, 2472–2480 (2013).
Prinzen, F. W. & Auricchio, A. The “missing” link between acute hemodynamic effect and clinical response. J. Cardiovasc. Transl. Res. 5, 188–195 (2012).
van Deursen, C. J. et al. The value of the 12-lead ECG for evaluation and optimization of cardiac resynchronization therapy in daily clinical practice. J. Electrocardiol. 47, 202–211 (2014).
Gold, M. R. et al. Effect of QRS duration and morphology on cardiac resynchronization therapy outcomes in mild heart failure: results from the Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction (REVERSE) study. Circulation 126, 822–829 (2012).
Author information
Authors and Affiliations
Contributions
K.V. and F.W.P. researched data for the article. All the authors contributed substantially to discussion of content and wrote the manuscript. K.V. and F.W.P. reviewed/edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
K.V. has received research grants from Medtronic. F.W.P. has received research grants from Biological Delivery Systems (Johnson & Johnson), EBR Systems, Medtronic, MSD, and Proteus Biomedical; and is an advisor to St. Jude Medical. The other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Vernooy, K., van Deursen, C., Strik, M. et al. Strategies to improve cardiac resynchronization therapy. Nat Rev Cardiol 11, 481–493 (2014). https://doi.org/10.1038/nrcardio.2014.67
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2014.67
This article is cited by
-
Monolithic silicon for high spatiotemporal translational photostimulation
Nature (2024)
-
Patient Selection for Biventricular Cardiac Resynchronization Therapy, His Bundle Pacing, and Left Bundle Branch Pacing
Current Cardiovascular Risk Reports (2021)
-
Physiologic heart rate dependency of the PQ interval and its sex differences
Scientific Reports (2020)
-
Patient-specific heart simulation can identify non-responders to cardiac resynchronization therapy
Heart and Vessels (2020)
-
Prevention of non-response to cardiac resynchronization therapy: points to remember
Heart Failure Reviews (2020)