Abstract
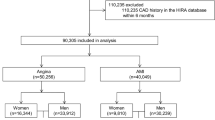
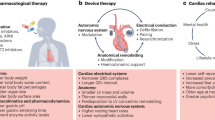
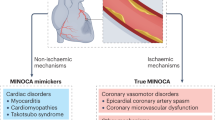
Scientific interest in ischaemic heart disease (IHD) in women has grown considerably over the past 2 decades. A substantial amount of the literature on this subject is centred on sex differences in clinical aspects of IHD. Many reports have documented sex-related differences in presentation, risk profiles, and outcomes among patients with IHD, particularly acute myocardial infarction. Such differences have often been attributed to inequalities between men and women in the referral and treatment of IHD, but data are insufficient to support this assessment. The determinants of sex differences in presentation are unclear, and few clues are available as to why young, premenopausal women paradoxically have a greater incidence of adverse outcomes after acute myocardial infarction than men, despite having less-severe coronary artery disease. Although differential treatment on the basis of patient sex continues to be described, the extent to which such inequalities persist and whether they reflect true disparity is unclear. Additionally, much uncertainty surrounds possible sex-related differences in response to cardiovascular therapies, partly because of a persistent lack of female-specific data from cardiovascular clinical trials. In this Review, we assess the evidence for sex-related differences in the clinical presentation, treatment, and outcome of IHD, and identify gaps in the literature that need to be addressed in future research efforts.
Key Points
-
Important differences exist between women and men in clinical presentation, recognition of symptoms by patients and physicians, outcome, and response to treatment for ischaemic heart disease (IHD)
-
Among patients with IHD, environmental or behavioural causes of sex-related differences in outcomes might be more important than biological factors
-
Onset of IHD in women, manifesting as an acute myocardial infarction before the age of 65 years, is associated with adverse outcomes compared with men of a similar age
-
A traditional diagnostic strategy, focusing on detection of severe coronary stenoses, is likely to be inadequate in women
-
Additional invasive testing aimed at determining endothelial coronary dysfunction might be useful to risk-stratify women with chest pain and minimal or no obstructive coronary artery disease
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Go, A. S. et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127, e6–e245 (2013).
Poon, S. et al. Bridging the gender gap: insights from a contemporary analysis of sex-related differences in the treatment and outcomes of patients with acute coronary syndromes. Am. Heart J. 163, 66–73 (2012).
Rajadurai, J. et al. Women's cardiovascular health: perspectives from South-East Asia. Nat. Rev. Cardiol. 9, 464–477 (2012).
Vaccarino, V. Ischemic heart disease in women: many questions, few facts. Circ. Cardiovasc. Qual. Outcomes 3, 111–115 (2010).
Murabito, J. M., Evans, J. C., Larson, M. G. & Levy, D. Prognosis after the onset of coronary heart disease. An investigation of differences in outcome between the sexes according to initial coronary disease presentation. Circulation 88, 2548–2555 (1993).
Lerner, D. J. & Kannel, W. B. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am. Heart J. 111, 383–390 (1986).
Hemingway, H. et al. Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation 117, 1526–1536 (2008).
Hochman, J. S. et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N. Engl. J. Med. 341, 226–232 (1999).
Berger, J. S. et al. Sex differences in mortality following acute coronary syndromes. JAMA 302, 874–882 (2009).
Genders, T. S. et al. A clinical prediction rule for the diagnosis of coronary artery disease: validation, updating, and extension. Eur. Heart J. 32, 1316–1330 (2011).
Milner, K. A., Funk, M., Arnold, A. & Vaccarino, V. Typical symptoms are predictive of acute coronary syndromes in women. Am. Heart J. 143, 283–288 (2002).
Canto, J. G. et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 307, 813–822 (2012).
Milner, K. A. et al. Gender differences in symptom presentation associated with coronary heart disease. Am. J. Cardiol. 84, 396–399 (1999).
Bugiardini, R. Women, 'nonspecific' chest pain, and normal or near-normal coronary angiograms are not synonymous with favourable outcome. Eur. Heart J. 27, 1387–1389 (2006).
Kreatsoulas, C., Shannon, H. S., Giacomini, M., Velianou, J. L. & Anand, S. S. Reconstructing angina: cardiac symptoms are the same in women and men. JAMA Intern. Med. 173, 829–833 (2013).
Mackay, M. H., Ratner, P. A., Johnson, J. L., Humphries, K. H. & Buller, C. E. Gender differences in symptoms of myocardial ischaemia. Eur. Heart J. 32, 3107–3114 (2011).
Bugiardini, R. & Bairey Merz, C. N. Angina with “normal” coronary arteries: a changing philosophy. JAMA 293, 477–484 (2005).
Bugiardini, R. et al. Angina, “normal” coronary angiography, and vascular dysfunction: risk assessment strategies. PLoS Med. 4, e12 (2007).
Shaw, L. J., Bugiardini, R. & Merz, C. N. Women and ischemic heart disease: evolving knowledge. J. Am. Coll. Cardiol. 54, 1561–1575 (2009).
Mosca, L., Mochari-Greenberger, H., Dolor, R. J., Newby, L. K. & Robb, K. J. Twelve-year follow-up of American women's awareness of cardiovascular disease risk and barriers to heart health. Circ. Cardiovasc. Qual. Outcomes 3, 120–127 (2010).
Mosca, L. et al. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation 127, 1254–1263 (2013).
Fukuoka, Y. et al. Is severity of chest pain a cue for women and men to recognize acute myocardial infarction symptoms as cardiac in origin? Prog. Cardiovasc. Nurs. 22, 132–137 (2007).
Rosengren, A. et al. Sex, age, and clinical presentation of acute coronary syndromes. Eur. Heart J. 25, 663–670 (2004).
Mulvagh, S. L. et al. Contrast echocardiography: current and future applications. J. Am. Soc. Echocardiogr. 13, 331–342 (2000).
Nandalur, K. R., Dwamena, B. A., Choudhri, A. F., Nandalur, M. R. & Carlos, R. C. Diagnostic performance of stress cardiac magnetic resonance imaging in the detection of coronary artery disease: a meta-analysis. J. Am. Coll. Cardiol. 50, 1343–1353 (2007).
Centers for Disease Control and Prevention (CDC). Prevalence of heart disease—United States, 2006–2010. MMWR Morb. Mortal. Wkly Rep. 60, 1377–1381 (2011).
Gibbons, R. J. et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). Circulation 106, 1883–1892 (2002).
Shaw, L. J. et al. The value of estimated functional capacity in estimating outcome: results from the NHBLI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Study. J. Am. Coll. Cardiol. 47, S36–S43 (2006).
Mieres, J. H. et al. Role of noninvasive testing in the clinical evaluation of women with suspected coronary artery disease: consensus statement from the Cardiac Imaging Committee, Council on Clinical Cardiology, and the Cardiovascular Imaging and Intervention Committee, Council on Cardiovascular Radiology and Intervention, American Heart Association. Circulation 111, 682–696 (2005).
Grzybowski, A. et al. How to improve noninvasive coronary artery disease diagnostics in premenopausal women? The influence of menstrual cycle on ST depression, left ventricle contractility, and chest pain observed during exercise echocardiography in women with angina and normal coronary angiogram. Am. Heart J. 156, 964.e1–964.e5 (2008).
Shaw, L. J. et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) study: part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. J. Am. Coll. Cardiol. 47 (Suppl.), S4–S20 (2006).
Lanza, G. A. & Crea, F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121, 2317–2325 (2010).
Maseri, A., Crea, F., Kaski, J. C. & Crake, T. Mechanisms of angina pectoris in syndrome X. J. Am. Coll. Cardiol. 17, 499–506 (1991).
Bugiardini, R., Pozzati, A., Ottani, F., Morgagni, G. L. & Puddu, P. Vasotonic angina: a spectrum of ischemic syndromes involving functional abnormalities of the epicardial and microvascular coronary circulation. J. Am. Coll. Cardiol. 22, 417–425 (1993).
Gan, S. C. et al. Treatment of acute myocardial infarction and 30-day mortality among women and men. N. Engl. J. Med. 343, 8–15 (2000).
Bugiardini, R., Manfrini, O. & De Ferrari, G. M. Unanswered questions for management of acute coronary syndrome: risk stratification of patients with minimal disease or normal findings on coronary angiography. Arch. Intern. Med. 166, 1391–1395 (2006).
Scanlon, P. J. et al. ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation 99, 2345–2357 (1999).
Ong, P. et al. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J. Am. Coll. Cardiol. 59, 655–662 (2012).
Budoff, M. J. et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicentre ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J. Am. Coll. Cardiol. 52, 1724–1732 (2008).
Beigel, R. et al. Prognostic implications of nonobstructive coronary artery disease in patients undergoing coronary computed tomographic angiography for acute chest pain. Am. J. Cardiol. 111, 941–945 (2013).
Lin, F. Y. et al. Mortality risk in symptomatic patients with nonobstructive coronary artery disease: a prospective 2-centre study of 2,583 patients undergoing 64-detector row coronary computed tomographic angiography. J. Am. Coll. Cardiol. 58, 510–519 (2011).
Min, J. K. et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicentre CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicentre Registry) of 23,854 patients without known coronary artery disease. J. Am. Coll. Cardiol. 58, 849–860 (2011).
Martinez, M. W. et al. Myocardial infarction with normal coronary arteries: a role for MRI? Clin. Chem. 53, 995–996 (2007).
Steg, P. G. et al. Impact of collateral flow to the occluded infarct-related artery on clinical outcomes in patients with recent myocardial infarction: a report from the randomized occluded artery trial. Circulation 121, 2724–2730 (2010).
Wolff, S. D. et al. Myocardial first-pass perfusion magnetic resonance imaging: a multicentre dose-ranging study. Circulation 110, 732–737 (2004).
Schwitter, J. et al. MR-IMPACT: comparison of perfusion-cardiac magnetic resonance with single-photon emission computed tomography for the detection of coronary artery disease in a multicentre, multivendor, randomized trial. Eur. Heart J. 29, 480–489 (2008).
Panting, J. R. et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N. Engl. J. Med. 346, 1948–1953 (2002).
Schwitter, J. Extending the frontiers of cardiac magnetic resonance. Circulation 118, 109–112 (2008).
Reynolds, H. R. et al. Mechanisms of myocardial infarction in women without angiographically obstructive coronary artery disease. Circulation 124, 1414–1425 (2011).
Mieres, J. H. et al. American Society of Nuclear Cardiology consensus statement: Task Force on Women and Coronary Artery Disease—the role of myocardial perfusion imaging in the clinical evaluation of coronary artery disease in women [correction]. J. Nucl. Cardiol. 10, 95–101 (2003).
Klocke, F. J. et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to revise the 1995 guidelines for the clinical use of cardiac radionuclide imaging). Circulation 108, 1404–1418 (2003).
Matsunari, I. et al. Attenuation-corrected rest thallium-201/stress technetium 99m sestamibi myocardial SPECT in normals. J. Nucl. Cardiol. 5, 48–55 (1998).
Hemingway, H. et al. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 295, 1404–1411 (2006).
Daly, C. et al. Gender differences in the management and clinical outcome of stable angina. Circulation 113, 490–498 (2006).
Fox, K. et al. Guidelines on the management of stable angina pectoris: executive summary: the Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. Eur. Heart J. 27, 1341–1381 (2006).
Crilly, M., Bundred, P., Hu, X., Leckey, L. & Johnstone, F. Gender differences in the clinical management of patients with angina pectoris: a cross-sectional survey in primary care. BMC Health Serv. Res. 7, 142 (2007).
Johnston, N., Schenck-Gustafsson, K. & Lagerqvist, B. Are we using cardiovascular medications and coronary angiography appropriately in men and women with chest pain? Eur. Heart J. 32, 1331–1336 (2011).
Vaccarino, V., Krumholz, H. M., Berkman, L. F. & Horwitz, R. I. Sex differences in mortality after myocardial infarction. Is there evidence for an increased risk for women? Circulation 91, 1861–1871 (1995).
Wenger, N. K., Shaw, L. J. & Vaccarino, V. Coronary heart disease in women: update 2008. Clin. Pharmacol. Ther. 83, 37–51 (2008).
Champney, K. P. et al. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction. Heart 95, 895–899 (2009).
Jneid, H. et al. Sex differences in medical care and early death after acute myocardial infarction. Circulation 118, 2803–2810 (2008).
Capewell, S. et al. Short-term and long-term outcomes in 133,429 emergency patients admitted with angina or myocardial infarction in Scotland, 1990–2000: population-based cohort study. Heart 92, 1563–1570 (2006).
Fuster, V. Elucidation of the role of plaque instability and rupture in acute coronary events. Am. J. Cardiol. 76, 24C–33C (1995).
Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1,000 patients. Lancet 343, 311–322 (1994).
Tamis-Holland, J. E. et al. Benefits of direct angioplasty for women and men with acute myocardial infarction: results of the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes Angioplasty (GUSTO II-B) angioplasty substudy. Am. Heart J. 147, 133–139 (2004).
Kim, E. S. & Menon, V. Status of women in cardiovascular clinical trials. Arterioscler. Thromb. Vac. Biol. 29, 279–283 (2009).
Bavry, A. A. et al. Invasive therapy along with glycoprotein IIb/IIIa inhibitors and intracoronary stents improves survival in non-ST-segment elevation acute coronary syndromes: a meta-analysis and review of the literature. Am. J. Cardiol. 93, 830–835 (2004).
Glaser, R. et al. Benefit of an early invasive management strategy in women with acute coronary syndromes. JAMA 288, 3124–3129 (2002).
Lansky, A. J. et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation 111, 940–953 (2005).
Cho, L. et al. Clinical benefit of glycoprotein IIb/IIIa blockade with abciximab is independent of gender: pooled analysis from EPIC, EPILOG and EPISTENT trials. Evaluation of 7E3 for the prevention of ischemic complications. Evaluation in percutaneous transluminal coronary angioplasty to improve long-term outcome with abciximab GP IIb/IIIa blockade. Evaluation of platelet IIb/IIIa inhibitor for stent. J. Am. Coll. Cardiol. 36, 381–386 (2000).
Boersma, E. et al. Platelet glycoprotein IIb/IIIa inhibitors in acute coronary syndromes: a meta-analysis of all major randomised clinical trials. Lancet 359, 189–198 (2002).
Healy, B. The Yentl syndrome. N. Engl. J. Med. 325, 274–276 (1991).
Bugiardini, R., Oestrada, J. L., Nikus, K., Hall, A. S. & Manfrini, O. Gender bias in acute coronary syndromes. Curr. Vasc. Pharmacol. 8, 276–284 (2010).
Blomkalns, A. L. et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) national quality improvement initiative. J. Am. Coll. Cardiol. 45, 832–837 (2005).
Anand, S. S. et al. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J. Am. Coll. Cardiol. 46, 1845–1851 (2005).
Dey, S. et al. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: the Global Registry of Acute Coronary Events. Heart 95, 20–26 (2009).
Vaccarino, V. et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N. Engl. J. Med. 353, 671–682 (2005).
Karp, I., Chen, S. F. & Pilote, L. Sex differences in the effectiveness of statins after myocardial infarction. CMAJ 176, 333–338 (2007).
Walsh, J. M. & Pignone, M. Drug treatment of hyperlipidemia in women. JAMA 291, 2243–2252 (2004).
Shekelle, P. G. et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status: a meta-analysis of major clinical trials. J. Am. Coll. Cardiol. 41, 1529–1538 (2003).
First International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous atenolol among 16,027 cases of suspected acute myocardial infarction: ISIS-1. Lancet 2, 57–66 (1986).
Institute of Medicine (eds Wizemann, T. & Pardue, M.) Exploring the Biological Contributions to Human Health: Does Sex Matter? (The National Academy Press, 2001).
Aldea, G. S. et al. Effect of gender on postoperative outcomes and hospital stays after coronary artery bypass grafting. Ann. Thorac. Surg. 67, 1097–1103 (1999).
Stern, S. & Bayes de Luna, A. Coronary artery spasm: a 2009 update. Circulation 119, 2531–2534 (2009).
Selzer, A., Langston, M., Ruggeroli, C. & Cohn, K. Clinical syndrome of variant angina with normal coronary arteriogram. N. Engl. J. Med. 295, 1343–1347 (1976).
Seung-Woon, R. et al. The impact of gender difference on angiographic characteristics during intracoronary acetylcholine provocation test in Korean patients [abstract TCT-437]. J. Am. Coll. Cardiol. 60 (Suppl. B), B124 (2012).
Bory, M. et al. Coronary artery spasm in patients with normal or near normal coronary arteries. Long-term follow-up of 277 patients. Eur. Heart J. 17, 1015–1021 (1996).
Pozzati, A., Pancaldi, L. G., Di Pasquale, G., Pinelli, G. & Bugiardini, R. Transient sympathovagal imbalance triggers “ischemic” sudden death in patients undergoing electrocardiographic Holter monitoring. J. Am. Coll. Cardiol. 27, 847–852 (1996).
Yoo, S. Y. & Kim, J. Y. Recent insights into the mechanisms of vasospastic angina. Korean Circ. J. 39, 505–511 (2009).
Egashira, K. et al. Basal release of endothelium-derived nitric oxide at site of spasm in patients with variant angina. J. Am. Coll. Cardiol. 27, 1444–1449 (1996).
Walling, A. et al. Long-term prognosis of patients with variant angina. Circulation 76, 990–997 (1987).
Mishra, P. K. Variations in presentation and various options in management of variant angina. Eur. J. Cardiothorac. Surg. 29, 748–759 (2006).
Waters, D. D. et al. Factors influencing the long-term prognosis of treated patients with variant angina. Circulation 68, 258–265 (1983).
Ong, P., Athanasiadis, A., Borgulya, G., Voehringer, M. & Sechtem, U. 3-year follow-up of patients with coronary artery spasm as cause of acute coronary syndrome: the CASPAR (coronary artery spasm in patients with acute coronary syndrome) study follow-up. J. Am. Coll. Cardiol. 57, 147–152 (2011).
Asbury, E. A., Creed, F. & Collins, P. Distinct psychosocial differences between women with coronary heart disease and cardiac syndrome X. Eur. Heart J. 25, 1695–1701 (2004).
Camici, P. G. & Crea, F. Coronary microvascular dysfunction. N. Engl. J. Med. 356, 830–840 (2007).
Khuddus, M. A. et al. An intravascular ultrasound analysis in women experiencing chest pain in the absence of obstructive coronary artery disease: a substudy from the National Heart, Lung and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE). J. Interv. Cardiol. 23, 511–519 (2010).
Wenger, N. K. Women and coronary heart disease: a century after Herrick: understudied, underdiagnosed, and undertreated. Circulation 126, 604–611 (2012).
Bairey Merz, C. N. et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation (WISE) study: part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J. Am. Coll. Cardiol. 47 (3 Suppl.), S21–S29 (2006).
Jespersen, L. et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur. Heart J. 33, 734–744 (2012).
Kaski, J. C. et al. Cardiac syndrome X: clinical characteristics and left ventricular function. Long-term follow-up study. J. Am. Coll. Cardiol. 25, 807–814 (1995).
Gulati, M. et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch. Intern. Med. 169, 843–850 (2009).
Johnson, B. D. et al. Prognosis in women with myocardial ischemia in the absence of obstructive coronary disease: results from the National Institutes of Health-National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 109, 2993–2999 (2004).
Oerlemans, J. G., Lagro-Janssen, A. L. & Bakx, C. Angina pectoris and normal coronary arteries: prevalence and prognosis in men and women [Dutch]. Ned. Tijdschr. Geneeskd. 144, 522–527 (2000).
von Mering, G. O. et al. Abnormal coronary vasomotion as a prognostic indicator of cardiovascular events in women: results from the National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). Circulation 109, 722–725 (2004).
Bugiardini, R., Manfrini, O., Pizzi, C., Fontana, F. & Morgagni, G. Endothelial function predicts future development of coronary artery disease: a study of women with chest pain and normal coronary angiograms. Circulation 109, 2518–2523 (2004).
Pepine, C. J. et al. Coronary microvascular reactivity to adenosine predicts adverse outcome in women evaluated for suspected ischemia: results from the National Heart, Lung and Blood Institute WISE (Women's Ischemia Syndrome Evaluation) Study. J. Am. Coll. Cardiol. 55, 2825–2832 (2010).
Britten, M. B., Zeiher, A. M. & Schächinger, V. Microvascular dysfunction in angiographically normal or mildly diseased coronary arteries predicts adverse cardiovascular long-term outcome. Coron. Artery Dis. 15, 259–264 (2004).
Fragasso, G. et al. Coronary slow-flow causing transient myocardial hypoperfusion in patients with cardiac syndrome X: long-term clinical and functional prognosis. Int. J. Cardiol. 137, 137–144 (2009).
Bugiardini, R., Borghi, A., Biagetti, L. & Puddu, P. Comparison of verapamil versus propranolol therapy in syndrome X. Am. J. Cardiol. 63, 286–290 (1989).
Xhyheri, B. & Bugiardini, R. Diagnosis and treatment of heart disease: are women different from men? Prog. Cardiovasc. Dis. 53, 227–236 (2010).
Kaski, J. C., Rosano, G., Gavrielides, S. & Chen, L. Effects of angiotensin-converting enzyme inhibition on exercise-induced angina and ST segment depression in patients with microvascular angina. J. Am. Coll. Cardiol. 23, 652–657 (1994).
Nalbantgil, I. et al. Therapeutic benefits of cilazapril in patients with syndrome X. Cardiology 89, 130–133 (1998).
Pauly, D. F. et al. In women with symptoms of cardiac ischemia, nonobstructive coronary arteries, and microvascular dysfunction, angiotensin-converting enzyme inhibition is associated with improved microvascular function: A double-blind randomized study from the National Heart, Lung and Blood Institute Women's Ischemia Syndrome Evaluation (WISE). Am. Heart J. 162, 678–684 (2011).
Akashi, Y. J., Nef, H. M., Mollmann, H. & Ueyama, T. Stress cardiomyopathy. Annu. Rev. Med. 61, 271–286 (2010).
Yoshioka, T. et al. Clinical implications of midventricular obstruction and intravenous propranolol use in transient left ventricular apical ballooning (Tako-tsubo cardiomyopathy). Am. Heart J. 155, 526.e1–526.e7 (2008).
Wittstein, I. S. et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N. Engl. J. Med. 352, 539–548 (2005).
Bielecka-Dabrowa, A. et al. Takotsubo cardiomyopathy—the current state of knowledge. Int. J. Cardiol. 142, 120–125 (2010).
Akashi, Y. J., Goldstein, D. S., Barbaro, G. & Ueyama, T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation 118, 2754–2762 (2008).
Edwards, F. H., Carey, J. S., Grover, F. L., Bero, J. W. & Hartz, R. S. Impact of gender on coronary bypass operative mortality. Ann. Thorac. Surg. 66, 125–131 (1998).
Weintraub, W. S., Wenger, N. K., Jones, E. L., Craver, J. M. & Guyton, R. A. Changing clinical characteristics of coronary surgery patients. Differences between men and women. Circulation 88, II79–II86 (1993).
Woods, S. E., Noble, G., Smith, J. M. & Hasselfeld, K. The influence of gender in patients undergoing coronary artery bypass graft surgery: an eight-year prospective hospitalized cohort study. J. Am. Coll. Surg. 196, 428–434 (2003).
Vaccarino, V., Abramson, J. L., Veledar, E. & Weintraub, W. S. Sex differences in hospital mortality after coronary artery bypass surgery: evidence for a higher mortality in younger women. Circulation 105, 1176–1181 (2002).
Kelsey, S. F. et al. Results of percutaneous transluminal coronary angioplasty in women. 1985–1986 National Heart, Lung, and Blood Institute's Coronary Angioplasty Registry. Circulation 87, 720–727 (1993).
Holubkov, R. et al. Angina 1 year after percutaneous coronary intervention: a report from the NHLBI Dynamic Registry. Am. Heart J. 144, 826–833 (2002).
Jacobs, A. K. et al. Better outcome for women compared with men undergoing coronary revascularization: a report from the Bypass Angioplasty Revascularization Investigation (BARI). Circulation 98, 1279–1285 (1998).
Thompson, C. A. et al. Gender-based differences of percutaneous coronary intervention in the drug-eluting stent era. Catheter. Cardiovasc. Interv. 67, 25–31 (2006).
Abbott, J. D. et al. Gender-based outcomes in percutaneous coronary intervention with drug-eluting stents (from the National Heart, Lung, and Blood Institute Dynamic Registry). Am. J. Cardiol. 99, 626–631 (2007).
Argulian, E. et al. Gender differences in short-term cardiovascular outcomes after percutaneous coronary interventions. Am. J. Cardiol. 98, 48–53 (2006).
Yang, F., Minutello, R. M., Bhagan, S., Sharma, A. & Wong, S. C. The impact of gender on vessel size in patients with angiographically normal coronary arteries. J. Interv. Cardiol. 19, 340–344 (2006).
Mehilli, J. et al. Gender and restenosis after coronary artery stenting. Eur. Heart J. 24, 1523–1530 (2003).
Dickerson, J. A., Nagaraja, H. N. & Raman, S. V. Gender-related differences in coronary artery dimensions: a volumetric analysis. Clin. Cardiol. 33, E44–E49 (2010).
Vaccarino, V. et al. Sex differences in mortality after acute myocardial infarction: changes from 1994 to 2006. Arch. Intern. Med. 169, 1767–1774 (2009).
Vaccarino, V., Parsons, L., Every, N. R., Barron, H. V. & Krumholz, H. M. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N. Engl. J. Med. 341, 217–225 (1999).
Andrikopoulos, G. K. et al. Younger age potentiates post myocardial infarction survival disadvantage of women. Int. J. Cardiol. 108, 320–325 (2006).
Koek, H. L. et al. Short- and long-term prognosis after acute myocardial infarction in men versus women. Am. J. Cardiol. 98, 993–999 (2006).
Radovanovic, D. et al. Gender differences in management and outcomes in patients with Acute Coronary Syndromes: results on 20,290 patients from the AMIS Plus Registry. Heart 93, 1369–1375 (2007).
Vaccarino, V. et al. Sex differences in health status after coronary artery bypass surgery. Circulation 108, 2642–2647 (2003).
Vaccarino, V. et al. Gender differences in recovery after coronary artery bypass surgery. J. Am. Coll. Cardiol. 41, 307–314 (2003).
Abramson, J. L., Veledar, E., Weintraub, W. S. & Vaccarino, V. Association between gender and in-hospital mortality after percutaneous coronary intervention according to age. Am. J. Cardiol. 91, 968–971 (2003).
Rosengren, A. et al. Sex differences in survival after myocardial infarction in Sweden; data from the Swedish National Acute Myocardial Infarction Register. Eur. Heart J. 22, 314–322 (2001).
Russo, A. M. et al. Influence of gender on arrhythmia characteristics and outcome in the Multicentre UnSustained Tachycardia Trial. J. Cardiovasc. Electrophysiol. 15, 993–998 (2004).
Salomaa, V. et al. Decline in out-of-hospital coronary heart disease deaths has contributed the main part to the overall decline in coronary heart disease mortality rates among persons 35 to 64 years of age in Finland: the FINAMI study. Circulation 108, 691–696 (2003).
MacIntyre, K. et al. Gender and survival: a population-based study of 201,114 men and women following a first acute myocardial infarction. J. Am. Coll. Cardiol. 38, 729–735 (2001).
Centers for Disease Control and Prevention (CDC). State-specific mortality from sudden cardiac death—United States, 1999. MMWR Morb. Mortal. Wkly Rep. 51, 123–126 (2002).
Njølstad, I., Arnesen, E. & Lund-Larsen, P. G. Smoking, serum lipids, blood pressure, and sex differences in myocardial infarction. A 12-year follow-up of the Finnmark Study. Circulation 93, 450–456 (1996).
Kemp, H. G. Jr, Vokonas, P. S., Cohn, P. F. & Gorlin, R. The anginal syndrome associated with normal coronary arteriograms. Report of a six year experience. Am. J. Med. 54, 735–742 (1973).
Cannon, R. O. 3rd et al. Abnormal cardiac sensitivity in patients with chest pain and normal coronary arteries. J. Am. Coll. Cardiol. 16, 1359–1366 (1990).
Cannon R. O. 3rd & Epstein, S. E. “Microvascular angina” as a cause of chest pain with angiographically normal coronary arteries. Am. J. Cardiol. 61, 1338–1343 (1988).
Reis, S. E. et al. Coronary flow velocity response to adenosine characterizes coronary microvascular function in women with chest pain and no obstructive coronary disease. Results from the pilot phase of the Women's Ischemia Syndrome Evaluation (WISE) study. J. Am. Coll. Cardiol. 33, 1469–1475 (1999).
Acknowledgements
The authors of this Review are members of the European Society of Cardiology Working Group on Coronary Pathophysiology and Microcirculation, and acknowledge the European Society of Cardiology for financial support. Dr Vaccarino is supported by the National Institutes of Health, grant K24HL077506.
Author information
Authors and Affiliations
Contributions
V. Vaccarino, R. Corti, O. Manfrini, E. Cenko, and R. Bugiardini researched data for the article. V. Vaccarino, L. Badimon, M. Dorobantu, O. Manfrini, A. Pries, E. Cenko, and R. Bugiardini contributed substantially to the discussion of content. The article was written by V. Vaccarino, R. Corti, and R. Bugiardini. V. Vaccarino, L. Badimon, R. Corti, C. de Wit, M. Dorobantu, O. Manfrini, A. Koller, E. Cenko, and R. Bugiardini reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Vaccarino, V., Badimon, L., Corti, R. et al. Presentation, management, and outcomes of ischaemic heart disease in women. Nat Rev Cardiol 10, 508–518 (2013). https://doi.org/10.1038/nrcardio.2013.93
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2013.93
This article is cited by
-
Cardiac medication use in patients with suspected ischaemia without obstructive coronary arteries: sex differences and psychological distress
Netherlands Heart Journal (2021)
-
Facial Expressions of Emotions During Pharmacological and Exercise Stress Testing: the Role of Myocardial Ischemia and Cardiac Symptoms
International Journal of Behavioral Medicine (2021)
-
Sex and age differences in the association of heart rate responses to adenosine and myocardial ischemia in patients undergoing myocardial perfusion imaging
Journal of Nuclear Cardiology (2020)
-
Sex-Related Differences in Pharmacokinetics and Pharmacodynamics of Frequently Prescribed Drugs: A Review of the Literature
Advances in Therapy (2020)
-
Gender Differences in Residual Risk Factors for Major Adverse Cardiovascular Events Following ACS and How to Bridge the Gap
Current Atherosclerosis Reports (2020)