Abstract
Neuropsychiatric illnesses are associated with dysfunction in distributed prefrontal neural systems that underlie perception, cognition, social interactions, emotion regulation, and motivation. The high degree of learning-dependent plasticity in these networks—combined with the availability of advanced computerized technology—suggests that we should be able to engineer very specific training programs that drive meaningful and enduring improvements in impaired neural systems relevant to neuropsychiatric illness. However, cognitive training approaches for mental and addictive disorders must take into account possible inherent limitations in the underlying brain ‘learning machinery’ due to pathophysiology, must grapple with the presence of complex overlearned maladaptive patterns of neural functioning, and must find a way to ally with developmental and psychosocial factors that influence response to illness and to treatment. In this review, we briefly examine the current state of knowledge from studies of cognitive remediation in psychiatry and we highlight open questions. We then present a systems neuroscience rationale for successful cognitive training for neuropsychiatric illnesses, one that emphasizes the distributed nature of neural assemblies that support cognitive and affective processing, as well as their plasticity. It is based on the notion that, during successful learning, the brain represents the relevant perceptual and cognitive/affective inputs and action outputs with disproportionately larger and more coordinated populations of neurons that are distributed (and that are interacting) across multiple levels of processing and throughout multiple brain regions. This approach allows us to address limitations found in earlier research and to introduce important principles for the design and evaluation of the next generation of cognitive training for impaired neural systems. We summarize work to date using such neuroscience-informed methods and indicate some of the exciting future directions of this field.
Similar content being viewed by others
INTRODUCTION
It is now axiomatic that neuropsychiatric illnesses—the mental and addictive disorders—are associated with dysfunction in distributed prefrontal, fronto-limbic, and fronto-striatal neural systems that underlie perception, cognition, social interactions, emotion regulation, and motivation (For definition of key terms used in this review, please see Appendix) (Bush, 2010; Eisenberg and Berman, 2010; Hartley and Phelps, 2010; Koob and Volkow, 2010; Price and Drevets, 2010). The prefrontal cortical association areas are uncommitted at birth, programmed to be shaped over the lifetime by the individual's unique perceptual, cognitive, and affective experiences. This high degree of learning-dependent brain plasticity—combined with the availability of advanced computerized technology that allows us to deliver well-defined and constrained learning events to the brain—suggests that we should be able to engineer very specific training programs that drive meaningful and enduring improvements in impaired neural systems relevant to behavioral disorders.
If successful, this form of computerized cognitive neurotherapeutics should result in healthier, more adaptive real-world behaviors—and indeed, a whole field of research in this area has opened up over the past few years. (We will use the term ‘cognitive training’ and ‘cognitive neurotherapeutics’ interchangeably, with the understanding that the focus of treatment may be on perceptual, cognitive, or socio-affective functions. ‘Training’ is likely the better term, since the treatment method involves harnessing and promoting intact physiological mechanisms of neuroplasticity that support adaptive behaviors.) For example, Klingberg et al (2005) investigated intensive computerized working memory training in children with attention deficit disorder (ADD), and found improvements in response inhibition and reasoning as well as a decrease in parent-rated symptoms. In healthy subjects, training was associated with activation changes in frontal and parietal cortex, consistent with plasticity in a working memory network (Klingberg, 2010). Vinogradov's group examined intensive computerized auditory training in adults with persistent schizophrenia and showed that participants significantly improved their verbal memory performance as well as early magnetoencephalographic (MEG) responses in auditory and prefrontal cortex; cognitive gains were positively associated with quality of life 6 months later (Adcock et al, 2009; Fisher et al, 2009, 2010; Dale et al, 2010). In a large-scale trial of older adults, subjects who received computerized training in perceptual speed of processing showed significantly improved cognition, lower rates of depression, and lower medical expenditures at 1 year, plus greater self-rated health outcomes at 5 years, compared with those who received therapist coaching in reasoning and memory (Wolinsky et al, 2009a, 2009b, 2010); electroencephalography (EEG) revealed training-induced modifications in early visual processing that were associated with improvement in working memory (Berry et al, 2010). This ensemble of findings from across the lifespan indicates that individuals with impaired cognition from a number of etiologies can respond to targeted computerized neurocognitive training; that training can change functional activation patterns in the brain; that it can generalize to meaningful improvement in real-world behaviors; and that improvements can endure.
This notion of harnessing brain plasticity mechanisms for therapeutic interventions is not a new one (for a comprehensive recent review, see Cramer et al, 2011); it has been investigated in stroke and in traumatic brain injury (TBI) for some years and at an implicit level has served as the underpinning of neurorehabilitation approaches for the past century. Yet, neuropsychiatric illnesses have features that set them apart from other neurological disorders (Table 1):
-
First, neuropsychiatric illnesses are associated with multiple genes of small effect and have a strong neurodevelopmental component; some (or perhaps many) of the contributing genes affect plasticity-related mechanisms in the brain (Grande et al, 2010; Balu and Coyle, 2011). This suggests that the neuropsychiatrically impaired brain may—in some instances—be programmed at the outset to be an ‘impaired learner.’
-
Second, given their neurodevelopmental component, mental and addictive disorders generally have a gradual onset and often show high rates of comorbidity. In addition, illness course tends to be chronic or relapsing, with slow recovery and with each episode of illness increasing the likelihood of future episodes, through what has been termed a process of sensitization (Patten, 2008; Robinson and Berridge, 2008). This pattern suggests that the physiological experience of illness expression drives key neural systems in the direction of ever-more dysfunctional configurations. In other words, the neuropsychiatrically impaired brain is also an ‘overlearner’ of maladaptive associations, having spent many years practicing dysfunctional perceptions, cognitions, emotions, and actions. Reverberations throughout interacting systems—for example, between prefrontal and limbic networks—further amplifies such dysfunction over time and perpetuates illness-related behaviors, given the role that prefrontal cortex plays in social cognition, self-referential processing, cognitive appraisal, emotion regulation, motivated behavior, and impulse control.
-
Third, unlike neurologic disorders, neuropsychiatric illnesses have clinical trajectories that are heavily influenced by the social environment. Social/emotional learning and attachments, interpersonal experiences, psychological trauma, internal representations of self and others, and socio-cultural influences all influence the expression and course of illness (Grossman et al, 2003; Leonardo and Hen, 2008). This indicates that the neuropsychiatrically impaired brain—like all human brains—is a ‘networked learner’ and that cognitive interventions must capitalize on the various ways that social–emotional contexts can influence motivation, treatment adherence, and treatment response over the course of development (Meltzoff et al, 2009).
Taken together, these features indicate that cognitive training for mental and addictive disorders has several unique challenges: it must take into account possible inherent limitations in the underlying brain ‘learning machinery’ due to pathophysiology; it must grapple with the presence of complex overlearned maladaptive patterns of neural functioning; and it must find a way to ally with psychosocial and developmental factors that influence response to illness and to treatment (Table 1). The kinds of behavioral interventions that can work well for a healthy brain may not yield the desired outcomes when applied to a developmentally- and plasticity-impaired brain.
In this review, we will take a systems neuroscience-informed approach to these challenges. We will argue that cognitive training for neuropsychiatric disorders must be explicitly designed to induce specific and substantial distributed changes in cortical and subcortical representations and processing efficiency, and we will present suggestions on how to accomplish this goal. At the same time, we will keep in mind that any useful treatment tool built on these principles must also be delivered in a developmentally appropriate and scalable context that is engaging, rewarding, and motivating for the learner.
We will:
-
briefly review the current state of knowledge on cognitive remediation in neuropsychiatric illness, including methodological issues and other emerging questions in the field;
-
use findings from systems neuroscience both to answer some of the emerging questions and to think about how principles of learning-induced neuroplasticity can inform the design of cognitive neurotherapeutics;
-
present suggestions on how to translate these principles into successful computerized training methods for the impaired brain;
-
provide our thoughts about emerging research and future directions for this exciting new field.
CURRENT STATE OF KNOWLEDGE
Cognitive remediation as a specific form of intervention first emerged in the late 1960s, when Wagner performed a remarkably sophisticated experiment with schizophrenia inpatients—using a slide projector, levers, bells, and buzzers—to compare the effects of four 1/2-h contingent-reinforcement training sessions in attention and abstraction (Wagner, 1968). He observed that basic cognitive capacities were present but reduced in patients, and that patients definitely responded to training; he also noted that the experimenter was a positive social reinforcer who clearly ‘enhanced the motivational condition of the subjects.’ By the mid-1980s, Spaulding et al (1986) were suggesting that ‘persons with schizophrenia show deficits in … attention, perception, and cognition’ and that ‘remediation of these deficits by direct training may facilitate the effectiveness of … therapy’.
Since that time, essentially all of the research on cognitive remediation in neuropsychiatric illness has taken place in schizophrenia and has examined a wide variety of rehabilitation approaches, from computer-based drill-and-practice training in attention to the use of educational software to therapist-guided strategy coaching in pencil and paper problem-solving tasks. A large majority of the studies have been based on a neuropsychological model of brain function, which tends to emphasize: (1) The notion of ‘separable domains’—the idea that cognitive functions are ‘separate’ and can be assessed and trained independently of one another—for example, that attention, memory, and executive control are discrete functions; and (2) The concept of ‘rehabilitation’ or ‘remediation’—the idea that brains with cognitive impairments need to develop work-around approaches to compensate for functions that are unalterably damaged. McGurk et al (2007) performed a meta-analysis of 26 studies of cognitive remediation in schizophrenia and found a mean effect size of 0.41 for cognitive improvement and 0.36 for functional outcome. There was no significant heterogeneity in effect sizes across various cognitive domains based on either the type of method or hours of training, with the exception of verbal learning and memory. In this one domain, a larger effect size was associated with more hours of remediation (0.57) compared with fewer hours (0.29) and with computerized drill-and-practice (0.48) compared with drill-and-practice plus strategy coaching (0.23) (we will return to this finding later). Wykes et al (2011) recently performed a meta-analysis of 40 studies undertaken from 1973 to June 2009, rating the trial methodology of each study using the Clinical Trials Assessment Measure (assessing sample characteristics, allocation to treatment, comparison treatments, etc.) (Table 2). As in the study by McGurk et al (2007), many different forms of remediation were represented, had been studied in various combinations with other therapies or psychosocial rehabilitation, and were compared with a large assortment of ‘control conditions’. A mean global cognition effect size of 0.45 was found, with heterogeneity of effect sizes in global cognition, speed of processing, and reasoning and problem solving; however, the meta-analysis did not find that type of remediation, participant characteristics, or trial quality could account for this heterogeneity in cognitive outcomes (Table 2). In an exploratory analysis, functional outcomes were significantly better in the four studies where cognitive remediation was combined with some other form of rehabilitation and when it included strategy coaching (Table 3).
As one carefully examines the studies performed thus far in schizophrenia, perplexing questions emerge (we note that similar questions have emerged in the field of TBI and cognitive remediation (Rohling et al, 2009). Why—across a wide range of approaches—do average effect sizes for the most part remain stuck against a glass ceiling in the low-to-medium range? Why do identical approaches used in different studies (Penades et al, 2006; Wykes et al, 2007) yield such different outcomes? Why do more hours of remediation result in stronger effects for verbal learning and memory in the McGurk meta-analysis (McGurk et al, 2007)? What unexamined variables account for the heterogeneity of effects in the Wykes meta-analysis (eg, treatment ‘dose,’ treatment intensity) (Wykes et al, 2011)? Why—in the absence of adjunctive psychosocial interventions—do patients show little significant change in real-world functioning (Table 3)? Why do benefits show a tendency to fade over time once the patient is no longer actively engaged in treatment? Recalling Wagner's observations, what are the possible confounding effects when the intervention is delivered with positive social reinforcers that greatly enhance motivation, such as the enriched psychosocial context of a rehabilitation environment and meaningful social interactions with a therapist?
The short answer to these questions is that it is difficult to draw any definitive conclusions from the prior literature since a large and extremely disparate range of (combinations of) interventions delivered across a wide range of treatment durations and intensities using a multitude of study designs and analytic approaches applied to small samples of patients all appear to induce modest positive effects that do not generalize widely or robustly outside of the trained task in the absence of additional psychosocial therapy. Moreover, a number of the interventions have included therapist contact or other positive social reinforcement not provided in the control condition. Wykes et al (2011) infer that the various forms of cognitive remediation have ‘few salient differences’ and instead ‘lie along a dimension of learning support’; they suggest that the critical elements that result in the best outcomes are the explicit teaching of strategies and the use of ‘transfer techniques’—though their exploratory analysis indicates that this is true only when cognitive remediation occurs concomitantly with a rehabilitation environment, which was the case in only four studies, which for the most part were unblinded and/or did not control for confounds in terms of the amount of psychosocial incentives between treatment and control conditions. Thus, there is only one definite conclusion we can draw at the present time from the meta-analytic work in schizophrenia: that non-specific cognitive stimulation based on any number of approaches is moderately beneficial, and patients who receive such stimulation while getting one-to-one involvement/coaching from a therapist in a rehabilitation environment show better functional outcomes. This unsurprising conclusion—combined with a widely held view that serious mental illness is characterized by immutable neurodevelopmentally based impairments—is perhaps the source of what has been a fair amount of skepticism in the field about the ultimate usefulness of cognitive remediation as a targeted therapeutic treatment for neuropsychiatric illnesses.
We argue here that, moving forward, if a cognitive intervention is to be successful, it must have a well-articulated theoretical rationale and clearly understood, specific mechanisms of action that are grounded in the neuroscience of learning and cognition; it must induce a specific, robust, and enduring change in a well-defined set of cognitive/socio-affective functions and neurological outcome measures when studied under rigorously controlled conditions; and it must generalize beyond the trained task and result in meaningful behavioral improvements that affect real-world functioning. We also propose that the neuropsychological model of remediation requires updating and that a number of innovative and perhaps counterintuitive training approaches are necessary for achieving robust and widespread gains in cognition in the impaired brain. Advances in systems neuroscience provide a useful theoretical framework for addressing these issues, and point the way for the development of the next generation of cognitive training techniques.
KEY PROCESSES MUST BE ADDRESSED AS THE FIELD MOVES FORWARD
The past 15 years of experimental neuroscience have unequivocally demonstrated two fundamental principles regarding brain function. The first principle is that the brain performs its computational work via distributed neural systems that are continuously making predictions about incoming data and that are interacting in a probabilistic manner through variations in their oscillatory patterns (Buzsaki, 2006). The second principle is that inputs from the senses, the environment, and other brains calibrate and modify neural connections; that is, the brain changes with the introduction of new experiences and with the training of new perceptual, cognitive, socio-emotive, or motor skills (Figure 1, adapted from Buzsaki, 2006). Put another way, during successful learning, the brain selectively promotes neural activity patterns—cortical representations—that represent meaningful stimuli and behaviors at both lower and higher levels of processing, particularly those associated with reward (Figure 2, adapted from Jenkins et al, 1990; see Cruikshank and Weinberger, 1996 and Buonomano and Merzenich, 1998 for reviews). In addition, the past 10 years of clinical neuroscience have unequivocally demonstrated that major mental illnesses are characterized by a range of impairments in neural system functioning, including perceptual and pre-attentive processing; higher-order cognitive operations such as attention, working memory, and inhibitory control; and the processing of socio-affective stimuli (see Table 4; although most of this work has been done in schizophrenia, there has been a recent surge of findings in other disorders as well). We propose that any meaningful treatment approach to the complex problems of neuropsychiatric illness must be grounded in these three fundamental principles.
The brain is organized in a hierarchy of neural assemblies that consist of multiple parallel loops. Intermediate- and long-range connections link the various loops in the cerebral cortex, and link cortical assemblies to subcortical structures. Sensory information passes through the thalamus to sensory cortex, and is in turn modulated by prefrontal influences. Modification of connections is determined by input from the senses, the environment, and interactions with other brains. Adapted from Buzsaki (2006).
During successful learning, the brain enhances the neural representations of behaviorally relevant stimuli and actions. Monkeys trained to apply the tips of their second and third fingers to a rotating disc show substantially enlarged cortical representations of those digits' tips after training (Jenkins et al, 1990).
In contrast to earlier neuropsychological models of cognition, this is a systems neuroscience conceptualization, one that emphasizes the distributed nature of neural systems or neural assemblies that support cognitive and affective processing, as well as their plasticity. It is based on the notion that the brain can adapt throughout the lifespan to salient experiences by representing the relevant sensory and cognitive/affective inputs and action outputs with disproportionately larger and more coordinated populations of neurons that are distributed (and that are interacting) throughout multiple brain regions. It also implies that the impaired brain is capable of adaptive plastic change despite its underlying neuropathology, but that the magnitude of global improvement driven by any remediation method will be limited by the weakest link in the interacting neural systems. This neuroplasticity-based systems model allows us to address some of the limitations found in earlier remediation research and to propose three important considerations for the design of successful cognitive training for impaired neural systems.
Cognitive Training must Address Limitations in Perceptual/Pre-Attentive Processing
The first consideration is that neuropsychiatrically impaired brains often have limitations or alterations in their sensory and pre-attentive perceptual processing capacities. Though these have been particularly well studied in schizophrenia (Butler et al, 2007; Javitt, 2009; Dias et al, 2011), they are also present in bipolar disorder, in depression, in PTSD, in alcoholism, in cocaine addiction, in ADD, in autism, and in the aging brain (Table 4). In order for prefrontal ‘higher-level’ cortical operations to engage in efficient decision-making and adaptive learning, the brain must be able to continuously make accurate predictions about the near future (Liang et al, 2002; Mukai et al, 2007; Cao et al, 2008; Miller et al, 2008; Friedman-Hill et al, 2010; Nahum et al, 2010; Roelfsema et al, 2010; Rutman et al, 2010; Zanto et al, 2011). These predictions rely on rapidly and correctly comparing high-fidelity ‘lower-level’ perceptions of our current internal and external environments with past experiences (Figures 3 and 4). Thus, any process that leads to significant distortions in sensory and early perceptual representations in the brain can affect its ability to make accurate and relevant predictions and comparisons, to assign appropriate salience to incoming data, and to respond in an adaptive manner to environmental demands. For example, deficits in automatic auditory information processing in otherwise healthy individuals are associated with poor working memory and delayed verbal memory performance (Light et al, 2007); impaired sensory prediction is related to measures of delusional ideation in a psychiatrically normal sample (Teufel et al, 2010); and hearing loss in mid-adulthood significantly increases the risk of later developing dementia (Lin et al, 2011). The idea here is that throughout our lives, the establishment and maintenance of new skills are highly dependent on the quality of perceptual processing, for our senses are our sole source of information about the external world (Merzenich and DeCharms, 1996). When the quality of perceptual representations is degraded or abnormally biased, cognitive and socio-affective consequences appear (Figure 4). Perceptual representations may be affected by ‘primary’ deficits in the earliest phases of sensory inputs (peripheral sense organs, thalamus, sensory cortex), or they may be altered ‘secondary’ to deficits in prefrontal modulation of attentional resources that affect the appropriate processing of incoming information.
Prefrontal cortical areas interact bidirectionally with lower levels of sensory and perceptual operations, with multiple feed-back and feed-forward effects. A schematic representation is presented for the visual system. Adapted and modified from Ahissar et al (2009).
In order for prefrontal cortical operations to engage in efficient decision-making and adaptive behavior, the brain must be able to continuously make accurate predictions about the near future. These predictions rely on rapidly and accurately comparing high-fidelity perceptions of our current internal and external environments with past experiences.
How might this consideration be translated into a cognitive training technique? As a simple example, people with major depression show a decreased latency in their P1 response to negative vs positive target stimuli (Yang et al, 2011), indicating a very early pre-attentive negativity bias in emotion perception. Such a bias toward the processing of negative emotional stimuli will then feed forward and induce prefrontal association areas to preferentially attend to and assign salience to negative stimuli, as well as generate abnormal/maladaptive responses in amygdala and associated limbic system regions (Victor et al, 2010). This in turn perpetuates a brain that is biased toward selective enhancement of very early perceptual processing of all potentially negative emotional information encountered in its environment, a brain that is responding to a world continuously perceived and experienced as distressing (Kilgard, 2002). Successful treatment can certainly occur when the individual learns to challenge the conscious cognitions and biased interpretations related to these perceptions, as happens during cognitive behavioral therapy—though even remitted symptom-free patients still show abnormal pre-attentive ERP responses to emotional stimuli, perhaps indicating risk of relapse (Shestyuk and Deldin, 2010). An alternative (or complementary) approach might be to train the brain to pay less selective attention to negatively biased perceptual information, for example, through the kind of computerized tonic and phasic alertness training that has been successfully used to address abnormal attention bias in hemi-neglect patients (Degutis and Van Vleet, 2010). Indeed, such an approach has been successfully piloted in highly anxious children who show abnormal attention bias toward threatening stimuli (Bar-Haim et al, 2011) and is under study in major depression (Thomas Van Vleet, personal communication).
We emphasize that the interaction between higher and lower levels of processing is complex and bidirectional, for prefrontal cortical areas continuously and strongly influence multiple aspects of sensory and perceptual operations, with powerful feed-back and feed-forward effects (Figure 3; see also Liang et al, 2002; Mukai et al, 2007; Cao et al, 2008; Miller et al, 2008; Friedman-Hill et al, 2010; Nahum et al, 2010; Roelfsema et al, 2010; Rutman et al, 2010; Zanto et al, 2011). Gazzaley (2010), for instance, has shown that prefrontal modulation of early perceptual processing (100–200 ms after stimulus onset) impacts subsequent working memory performance—but that task practice, perceptual training, and aging effects in the brain, can all affect this relationship. Regardless of etiology or of the original location or directionality of the primary ‘lesion,’ the evidence indicates that degraded or biased processing of lower-level perceptual information will reverberate throughout distributed neural systems, and will affect higher-level prefrontal efficiency and function, including working memory and long-term memory encoding, as well as limbic and subcortical activation patterns. We postulate that attempts to remediate or improve higher-level functions in neuropsychiatric illnesses may hit a bottleneck if underlying perceptual processing limitations are not addressed. For instance, in order to perform a basic social cognition task successfully, such as identifying the emotion on a face, the brain must rapidly and accurately perform a visual scan of informative facial features (eyes, mouth, midfacial region), and then process that visual data in an efficient and accurate manner, creating stable and detailed cortical representations of the relevant sensory inputs. If these basic processes are degraded or ‘noisy’ in their earliest representations, as is the case in schizophrenia and autism (Wong et al, 2008; Butler et al, 2009; Hileman et al, 2011), the brain will have difficulty performing appropriate and adaptive complex multimodal operations, predictions, comparisons, or decisions on the visual data (Figure 5). This can lead not only to failures in encoding relevant signals from the environment, but also to high errors or ‘false alarms’ about irrelevant signals (see pre-clinical data on the higher-level effects of degraded auditory processing from the aged rat brain in de Villers-Sidani et al (2010). High ‘false alarms’—or the processing of task-irrelevant stimuli—in turn leads to overload on working memory systems (Zanto and Gazzaley, 2009).
If lower-level perceptual and/or attentional processes are degraded or abnormally biased, the brain will have difficulty adaptively performing other more complex multimodal operations, predictions, or decisions on the data.
High rates of task-irrelevant interference occurring at the pre-attentive level not only affect working memory, they also disrupt the brain's ability to assign appropriate salience to incoming information, and lead to abnormalities in neuromodulation (for discussion of prediction errors, learning, and neuromodulatory functions in the healthy brain, see Schultz and Dickinson, 2000; Nomoto et al, 2010; see also Axmacher et al, 2010; for discussion in the context of schizophrenia see Keefe et al, 2011). Relevant or novel stimuli are ‘missed’ and fail to generate the appropriate input/output mismatch that leads to attentional salience and representations in working memory. Irrelevant stimuli capture attentional resources, are incorrectly coded as salient or novel, enter into working memory, and increase activity in subcortical noradrenergic and dopaminergic systems. This creates an unstable state in the brain, leading to further inappropriate learning (see Mercado et al, 2001; Kilgard, 2002). As an example, the abnormal early processing of visual data from faces found in autism and schizophrenia appears to be a strong contributor to the poor social cognitive abilities in these disorders; poor social cognitive abilities combined with affective arousal and inappropriate attribution of salience found in schizophrenia in turn increases the risk for paranoia, further perpetuating a state of maladaptive memory formation (Dalton et al, 2005; Akiyama et al, 2008; Heinz and Schlagenhauf, 2010; Kirchner et al, 2011).
The point we are making here is that any remediation approach that does not address impairments or biases in early perceptual processing can lead to modest improvements in behavior, especially if the remediation is provided in an enriched therapeutic environment (as has been shown in the meta-analytic studies of schizophrenia), but it is unlikely that these gains will be robust, will generalize to broad new learning patterns, or will be associated with widespread and enduring improvements in the efficiency of distributed neural systems. For instance, we would predict that any attempt to train a person with schizophrenia or with autism to have better social skills—through group therapy, therapist coaching, or a virtual reality platform—will hit a plateau if the lower-level face-processing deficits are not addressed. Training that also improves the perception of and appropriate salience of facial features—along with their representation and manipulation in working memory—will, we propose, greatly enhance the success of social skills interventions in these disorders. Indeed, this has been recently shown to be the case both in schizophrenia (Roberts and Penn, 2009) and in autism (Hopkins et al, 2011). We note that this approach is ‘restorative’ in nature—the idea is not to develop compensatory or work-around strategies for impaired perceptual processes (be they basic and ‘primary’ in nature, or secondary to attentional biases), but rather to drive the impaired neural systems in the direction of more normal functioning through carefully engineered training strategies.
Constrained and Intensive Training Is Necessary to Induce Robust Plastic Changes in Cortex
The second consideration we propose is that, in order for a brain to undergo significant plastic changes, it must practice a well-defined skill at a sufficient level of difficulty for a sufficient amount of time; this may be especially true for an impaired brain. Skill learning is characterized by two general phases. The first phase involves rapid improvements in performance that are observed within a single training session and/or after initial training (Figure 6a). The second slower phase involves moderate gains in performance that progress across multiple training sessions (Kleim et al, 1996, 1998; Nudo et al, 1996; Karni et al, 1998). Each phase is supported by unique neural responses. For example, in motor skill learning, the initial fast phase is associated with activation of cerebellum and then fronto-striatal regions, whereas the later phase engages motor cortex (Ungerleider et al, 2002). Kleim et al (2004) have shown in rats that synaptogenesis and reorganization of motor maps within the cortex only occurs during the second, slower phase (see also Maviel et al, 2004 for similar findings concerning spatial memory in mice). Large-scale learning-dependent neural plasticity is temporally dissociated from learning-induced improvements in behavior; major plastic changes in neural representations occur only after sufficiently intense training of a specific skill.
(a) The first phase of skill learning involves rapid improvements in performance. (b) The second phase of learning is characterized by massive reorganization of task-specific representations in the brain.
Prior cognitive remediation methods—and indeed many behavioral interventions in neuropsychiatric illness—have tended to focus mainly on the first phase of learning, and often ask patients to train simultaneously across a diffuse set of skills. This phase can be thought of as a non-specific task-induced increase in performance efficiency, where rapid behavioral gains occur, probably due to the creation of a general task schema relying heavily on prefrontal processes (see Ahissar and Hochstein, 2004). This phase engages an early set of less-persistent plasticity mechanisms that involve changes in the efficacy of existing synapses (Rioult-Pedotti et al, 1998), increases in neuronal excitability (Aou et al, 1992), changes in neural activity that reflect the encoding of novel task-relevant patterns (Rioult-Pedotti et al, 1998; Laubach et al, 2000), or transient changes in task-specific cortical representations that occur, but do not persist, outside of the training session (eg, changes in movement representations after a single training session can last for several minutes before reverting to the pre-training state (Classen et al, 1998). This might explain the gains seen in any number of previous forms of cognitive remediation in schizophrenia: improvement in task performance occurs due to the activation of early plasticity mechanisms and/or from non-specific frontally mediated processes related to the creation of a more efficient task schema. This also likely explains the non-specific general effects seen when comparing multiple different cognitive remediation approaches in schizophrenia (McGurk et al, 2007; Wykes et al, 2011).
These processes are quite distinct from those in the second phase of learning. During this phase, behavioral gains are more modest and are approaching an asymptote, and yet experimental data indicate that the cortex is showing first, significant synaptogenesis, and next, massive reorganization of task-specific representations (Figure 6b). For example, Kleim et al (2004) have shown that during training in rats on a skilled reaching task, significant increases in synapse number within the motor cortex are not detectable until well after significant skill acquisition has occurred. Although trained animals exhibit a significant increase in reaching accuracy after only 3 days of training, the number of synapses per neuron within motor cortex does not significantly differ from untrained animals until after 7 days of training, while the distal forelimb representations in motor cortex are not significantly larger until after 10 days of training. In a human study, Karni et al (1995) used fMRI to show the reorganization of motor cortex in healthy adults while they performed motor tasks requiring rapid sequences of finger movements. Behavioral performance, indicated by the speed at which the trained sequence could be performed, reached an asymptote after 3 weeks of training. It was only at week 4 of training that the motor cortex, activated by the practiced sequence, became significantly enlarged compared with the unpracticed sequence. Additionally, this reorganization of motor cortex that occurred during the slow phase of learning persisted for several months, suggesting that it is related to the actual retention of the new motor skill.
In sum, the basic science indicates that, in order to (efficiently) move the learner well into the second phase of learning where significant and enduring cortical reorganization occurs, learning trials must be well defined or constrained, must be adaptive to the level of the given individual (must continuously adjust so that learning is occurring with a high level of success and at asymptote), and must be given for a sufficient number of trials. This indicates that the ability to develop many thousands of precisely defined learning events with precisely engineered timing, difficulty level, and reward schedules is an important feature of effective cognitive training methods.
Indeed, we would argue that cognitive training of insufficient intensity or duration—where the learner is not involved in precisely defined learning trials at threshold of performance for a sufficient number of trials—will not drive distributed enduring adaptive changes in a specific set of neural representations of interest, particularly in a neuropsychiatrically impaired brain. This may explain why many different remediation methods (usually of relatively low intensity and/or short duration and/or that train diffusely) applied in many different clinical contexts have yielded some behavioral improvement, but without convincing evidence of strong and lasting benefits. In the 26 schizophrenia studies in the McGurk et al (2007) meta-analysis, the median treatment intensity was 2 h/week and the median treatment duration was 7 weeks. The recent study by Owen et al (2010) in which roughly 30 min a week of ‘brain training exercises’ given for 6 weeks in over 10 000 individuals in Britain failed to drive significant improvement in cognition, may likely be an example of under-dosing; it is equivalent to saying that a leisurely stroll around the block twice a week for several weeks in healthy individuals fails to significantly improve aerobic capacity, proving that exercise does not improve physical fitness. The need for sufficiently intensive training of sufficiently long duration may be especially important in neuropsychiatric illness characterized by impaired neuromolecular mechanisms combined with many years of maladaptive learning events.
Cognitive Training Must Focus on Implicit Learning Mechanisms
The third consideration we propose is that the neuropsychiatrically impaired brain is often a ‘poor learner of new behaviors’ either through etiologic factors and/or the self-perpetuating nature of ever-more dysfunctional neural configurations related to disease expression. Thus, explicit instruction, insight, and strategy coaching often do not help the individual to change maladaptive patterns of behavior. The success of these kinds of approaches relies heavily on declarative/explicit learning and memory, and on intact motivation/reward systems, two domains that are demonstrably impaired in a number of neuropsychiatric illnesses (Ragland et al, 1996; Heckers et al, 1998; Kurtz et al, 2001; Arts et al, 2008; Bora et al, 2009; Hermens et al, 2010; Torralva et al, 2010). We suggest that impairments in the brain systems subserving explicit learning provide an inherent limitation to the utility of stand-alone instruction, strategy coaching, and other declarative memory-based therapeutic methods. (We will address the issue of motivation and reward at the conclusion of the review.) It is interesting to point out that, in the McGurk et al (2007) meta-analysis described earlier, a larger effect size in verbal learning/verbal memory was significantly associated with more hours of remediation vs fewer hours, and with drill-and-practice vs drill-and-practice that had been combined with strategy coaching. Two ideas emerge from this meta-analytic finding.
The first idea is that many hours of drill-and-practice can be successful in an impaired brain—suggesting that the effects of implicit learning and repetitive practice are still (relatively) intact even when explicit learning is broken. Indeed, although there are some inconsistent findings, the overall pattern is that behavioral responses to implicit learning and to repetitive practice of a well-defined task can be harnessed successfully in most major neuropsychiatric illnesses, including schizophrenia, Alzheimer's dementia, depression, and autism (Klimkowicz-Mrowiec et al, 2008; Nemeth et al, 2010). Similar to the point we made earlier about constrained and intensive training, this indicates that cognitive training should harness implicit learning mechanisms and employ repetitive, adaptive practice of critical cognitive and affective processing skills.
The second idea is that the addition of explicit instruction—the attempt to use declarative memory along with implicit learning—actually results in less behavioral improvement for the patient. This counterintuitive notion will require further investigation as the field moves forward. At present, our understanding of the detailed relationship between implicit and explicit learning mechanisms is still relatively unsophisticated, but a great deal of evidence suggests that—at least in the young, healthy brain—there is anatomic and behavioral dissociation as well as competition between these two systems (Poldrack and Packard, 2003; Voss and Gonsalves, 2010). However, the anatomic differentiation that seems so apparent in the healthy brain may not represent the picture in the impaired brain. Dennis and Cabeza (2010) recently showed that young subjects recruited the striatum for implicit learning and the medial temporal lobe for explicit learning, while—surprisingly—older adults recruited the medial temporal lobe during implicit learning. In fact, older adults showed no preferential regions of recruitment for either task, suggesting that, in the aging brain, there may be de-differentiation across memory systems. Patients with schizophrenia also show abnormal brain activation patterns during implicit learning, despite normal behavioral performance, as do patients with major depression (Zedkova et al, 2006; Naismith et al, 2010). It appears that in certain neuropsychiatric conditions, the neural instantiations of implicit and explicit learning may not show normal patterns of differentiation; the picture is of a brain that is inefficient in its various learning and memory operations. Due to these inefficiencies, training that occurs simultaneously or diffusely across perceptual or cognitive modalities may be ineffective or even counterproductive (see also Ahissar et al, 2009). Vinogradov's group have found evidence of possible competitive interference in verbal learning/memory in schizophrenia subjects assigned to a control computer games condition; these subjects showed worse performance on a list-learning task after 50 h of visually demanding computer games (Fisher et al, 2009). It appears as if intensive visual perceptual processing over a 10-week period interferes with explicit learning of verbal material in individuals who have impaired verbal memory systems. This finding, if replicated, will have important implications for the design and sequencing of training exercises for the impaired brain.
Indeed, in keeping with these data and with the basic neuroscience principles we underscored at the start of this section, recent models of human learning and memory emphasize the predictive and interactive nature of multiple memory systems (Henson and Gagnepain, 2010; Fell and Axmacher, 2011). In these models, the various memory systems differ primarily in their representational content and computational principles. For example, explicit/declarative memory binds items to their context and is available to consciousness, while implicit perceptual learning, which is not available to consciousness, enhances the representation of recurring features in the environment that define items of interest. Henson and Gagnepain (2010) propose that encoding and retrieval arise from recurrent interactions among the multiple systems: ‘lower’ representations of perceptual and semantic features feed forward to ‘higher’ representations of current items and their episodic context, while ‘higher’ representations generate predictions that are in turn fed back to lower levels (see also Takashima et al, 2006).
Put another way, interactions among the different memory systems are continuously occurring based on perceptual and semantic information that is being fed forward as well as expectancies and predictions that are being fed backwards (Figure 3)—given that the brain's machinery is continuously generating predictions about patterns in its environment and then using perceptual data for comparison and detection of either matches or mismatches (Buzsaki, 2006; Henson and Gagnepain, 2010). According to this model, training that improves the brain's ability to extract relevant perceptual and semantic data with high precision and feed it forward, and that also increases the brain's efficiency at making implicit rapid and accurate predictions/decisions about incoming data, should result in enhanced working memory and declarative memory function. Indeed, as Takashima et al (2006) concluded from an MEG study of the encoding of complex scenes, working memory processes associated with deep perceptual and semantic processing appear to act in tandem with top–down modulation of contextually constrained visual perception to promote successful declarative memory formation. This notion of continuously interacting memory systems is also consistent with the role of oscillatory phase synchronization between different brain regions in supporting interactions between working memory and long-term memory storage (Fell and Axmacher, 2011; see also Khader et al, 2010). We propose that these emerging ideas suggest that ‘tuning up’ perceptual and semantic processing and working memory capacity through implicit learning and/or repetitive practice may be the optimal approach to fixing broken explicit learning and memory systems in neuropsychiatrically impaired brains. Vinogradov et al have shown that intensive computerized auditory training in schizophrenia (implicit learning) improves performance on verbal delayed recognition tasks (explicit learning), with ‘normalization’ of brain activation patterns during a meta-cognitive verbal memory task (Subramaniam et al, in press), while Klingberg et al (2005) have shown a similar pattern of generalized behavioral and neural improvement after intensive visual working memory training in ADD.
IMPORTANT MODEL FEATURES OF LEARNING-DEPENDENT NEUROPLASTICITY
In the previous section, we selectively reviewed the emerging basic science of learning, and we argued that three somewhat counterintuitive considerations may be key to the design of cognitive neurotherapeutics for mental and addictive disorders: the need to target limitations or distortions in perceptual processing, the need to provide well defined and sufficiently intensive training at threshold, and the need to harness implicit learning mechanisms—both to improve critical cognitive/socio-affective skills, and to make the brain a more efficient ‘learner.’ Though we have elucidated each of these considerations as if they are independent from one another, they are in fact deeply interrelated, and they derive from pre-clinical findings of how neural systems change in response to experience. In this section, we briefly examine several features of learning-dependent neuroplasticity in auditory cortex as a model system for understanding critical neuroplasticity mechanisms. We then translate these features into specific principles that help to inform the design of human therapeutic tools.
Brain Plasticity Mechanisms Continuously Shape Neural Circuits and Behavior
The mechanisms that support plastic reorganization in the brain and its consequences on perception and behavior have been most extensively studied in animal models that focus on primary sensory cortical areas. We will highlight a few specific experiments from the auditory system, which is arguably one of the most studied systems with relevance to neuropsychiatric illness and has been extensively studied in humans and animal models using comparable neurophysiology techniques such as EEG (Arlinger et al, 2009; Javitt, 2009; Hitoglou et al, 2010; Witton, 2010).
Developing cortical circuits in primary auditory cortex (A1) are extremely sensitive to the presence or absence of clear sensory input patterns in the environment. Exposing infant rats to pulsed tones of a particular frequency 24 h/day during the second week of life (the sensitive period of plasticity in the rat auditory system) increases by threefold the number of A1 neurons tuned to that frequency (Zhang et al, 2001; de Villers-Sidani et al, 2007). Such distortion in A1 frequency coding persists into the adult life and profoundly shapes—or interferes with—perceptual discrimination in behavioral tasks (Han et al, 2007). Conversely, if the same animals are kept in an auditory environment devoid of sensory input patterns (because of the presence of moderate intensity auditory noise for example), functional maturation of the cortex is suspended and auditory cortical neurons, including inhibitory interneurons, remain very immature in their responses properties (Chang and Merzenich, 2003; de Villers-Sidani et al, 2008). These experiments indicate the intimate relationship linking environmental inputs during critical periods of development, cortical maturation, cortical mapping, and adult perceptual behavior; they suggest that aberrant, self-perpetuating cognitive, affective, and behavioral patterns may be set in motion early in life in genetically and constitutionally vulnerable individuals and amplified by dysfunctional environmental inputs. Thus, as we have noted earlier, while multiple genes of small effect contribute to the risk for mental and addictive disorders, extremely powerful developmental brain plasticity mechanisms probably also make a significant contribution to the clinical expression of these disorders.
Experience-dependent plasticity is not limited to early development, but significant differences do exist between adult plasticity and that of the developing brain. For example, while short passive exposures to discrete stimuli such as those described above have no measurable impact on adult cortical maps (Zhang et al, 2001; de Villers-Sidani et al, 2007), very prolonged and dramatic distortions in sensory inputs can influence the frequency representation in A1, as seen after a permanent lesion of a portion of the cochlea (Irvine and Rajan, 1997). In such instances, A1 progressively reorganizes to maximize the area of cortex responsive to the remaining active sensory inputs. Furthermore, prolonged noise exposure can revert A1 to a very immature and plastic state (Zhou et al, 2011). So in effect, cortical circuits constantly triggered by patterned inputs are consolidated, while those engaged in chaotic or undifferentiated activity remain ‘detuned’ and relatively more plastic. This observation has potentially interesting clinical implications. First, several common neuropsychiatric conditions—including autism, schizophrenia, and aging—have been associated with poorly integrated, dyscoordinated, or inefficient brain activity (Caspary et al, 2008; Oblak et al, 2009; Gonzalez-Burgos et al, 2010). This raises the possibility that sources of noise within the brain itself are directly contributing to the emergence of cognitive deficits. Second, the notion that ‘noisy’ or degraded representational systems might be maintained in immature but relatively more plastic states could represent an interesting opportunity for the elaboration of highly specific training strategies aimed at improving processing in systems having the most plastic potential first.
Cognitive Training Remodels Neural Circuits and Depends Heavily on Neuromodulatory Activity
In the mature cortex, the most effective method of achieving directed plastic reorganization of cortical circuits is by using attention-demanding intensive behavioral training strategies (Mahncke et al, 2006a; Seitz and Dinse, 2007). Reinforcement-based operant conditioning refines cortical mapping and processing in A1 in the adult rat (Bao et al, 2004), and induces changes in protein expression, inhibitory circuitry, and supporting glia (Klintsova et al, 2004; Bengtsson et al, 2005; Tokarski et al, 2007). Training can also induce adaptive reorganization in the auditory cortex of aged rats which, at baseline, show evidence of abnormal or degraded cortical maps due to age-related cognitive decline (Dinse, 2006; de Villers-Sidani et al, 2010) (Figure 7).
Targeted auditory training improves functional and structural impairments in the aged brain. (Above) In the aged rat brain, the normally smooth gradient of frequency tuning in the primary auditory cortex (A1) is disorganized and neurons lose their frequency tuning selectivity. Forty sessions of intensive training on a deviant tone detection paradigm completely reverses these impairments. The polygons shown above represent the location of neurons recorded in a typical rat A1 during cortical mapping experiments. On the top row, the color represents the neurons’ frequency tuning (blue for low frequency, red for high), while in the bottom row, the color represents the sharpness of tuning. (Below) Low power photomicrographs demonstrate the loss of parvalbumin (PV) immunoreactivity in the aged A1. PV is contained in a specific class of interneurons involved in salient stimulus detection and noise suppression in the cortex. The same auditory training task described above significantly increased the number of cells staining for PV in the cortex (a, d, g, j), decreased the number of cell staining only lightly for PV (b, e, h, k) and increased dendritic PV immunoreactivity (c, f, i). Error bars are SEM. Scale bar in g (apply for a and d): 200 μm; in h (apply for b and e): 100 μm; in i (apply for c and f): 50 μm. **P<0.01. Adapted from de Villers-Sidani et al (2010).
Training-directed brain plasticity depends heavily on the activity of neuromodulator systems involved in the regulation of arousal, attention, and reward mechanisms (Buonomano and Merzenich, 1998; Weinberger, 2003; Blake et al, 2006; Roelfsema et al, 2010). For example, passive pairing of an acoustic tone with electrical stimulation of cholinergic (nucleus basalis) or noradrenergic (locus ceruleus) nuclei massively increase the area of cortex tuned to the frequency of the tone (Kilgard and Merzenich, 1998; Bao et al, 2001; Froemke et al, 2007; Edeline et al, 2010). Interestingly, the precise timing of the electrical stimulation relative to the stimulus can reverse the direction of the plasticity. Bao et al (2001) showed that stimulation of the ventral tegmental area (VTA) after the occurrence of a 4-kHz tone but before a 9-kHz tone more than triples the area of A1 tuned to 4 kHz and selectively reduces A1 tuning to 9 kHz (Figure 8). Given that VTA activity is tightly linked to behavioral salience of inputs and to reward (Arias-Carrion et al, 2010), this finding suggests that the precise timing and nature of the delivery of rewards is important in developing effective training strategies (Rutkowski and Weinberger, 2005). This may be especially true in the impaired brain, where the response to rewarded events is weakened or biased; for example, in schizophrenia (Morris et al, 2008; Koch et al, 2010).
Pairing auditory tones with VTA stimulation affects plastic changes in A1. In A1, frequency tuning follows a tonotopic gradient where neurons tuned to low frequencies are found at one extremity of the map and neurons tuned to high frequencies are located at the other (a). Here, a sequence of two tones was presented along with stimulation of the VTA, which releases dopamine in the cortex. The first 4 kHz tone preceded the VTA stimulation by 500 ms; the second 9 kHz tone followed the VTA stimulation 500 ms later. This simple paradigm resulted in an ∼300% increase in the A1 area tuned to 4 kHz and a 50% decrease in A1 tuning to 9 kHz (b, c). These findings suggest that the timing of a reward provided in the context of perceptual training has to be carefully considered in order to maximize cortical plasticity responses *P<0.05, **P<0.0005. Adapted from Bao et al (2001).
In an elegant macaque study, Blake et al (2006) showed that a cognitive stimulus-reward association, or the ability to clearly identify a particular stimulus as a to-be-rewarded target vs an unrewarded non-target, is necessary to drive the stimulus-specific plastic changes observed in reinforcement-based learning. In this experiment, the monkeys had to identify a pre-determined target sound presented along with distractors. The animal, kept thirsty, signaled his response by slightly moving his head. If the answer was correct, a fluid reward was delivered through a tube. Since auditory cortical responses were continuously monitored, the authors noted that significant plastic changes in sound coding in A1 only occurred when the animal appeared to ‘know’ what the answer was (ie, the animal began to lick immediately after a correct answer, but before the fluid reward was delivered). In other words, for training to drive significant cortical reorganization, the animal in training must be able to reliably predict that its answer is going to be correct. Guessing a correct answer, even in the presence of a reward, will not be effective to drive plastic changes. Again, this finding highlights the necessity of being able to carefully control both the performance level and the reward schedule of training—learning events must be constructed such that the animal is able to predict with a high degree of accuracy when it has made a correct response. The key is to ‘re-calibrate’ the brain's ability to successfully predict meaningful associations.
In a paired-tone task, Zhou et al (2010) observed that once the initial stimulus in the target sequence was presented, neurons in the primary auditory cortex changed dynamically, specifically to exaggerate further the representation of the ‘predicted’ second stimulus in the target sequence. When the second stimulus occurred within the target sequence, more strongly excited, more coordinated, and more selectively responding neurons represented this over a larger cortical area (Figure 9). This study showed that cortical areas are not static, but instead can be biased moment by moment in time as a function of a prediction state. In a related study performed in rats, Polley et al (2006) demonstrated that ‘top–down’ prefrontal influences are involved in this phenomenon and therefore participate in the gating of training-specific plasticity in sensory cortex. These results are consistent with emerging work in humans.
Moment-to-moment top–down biasing of frequency tuning in A1 occurs after training on a sound sequence. The color of each polygon indicates the frequency tuning of neurons recorded in the A1 of control rats and rats trained to respond to the occurrence of a 7-kHz tone presented only after the occurrence of a 3-kHz tone. (Top row) Training resulted in a slight increase in the representation of each tone presented in isolation. (Middle row) When measured right after the presentation of a 3-kHz tone, the area of A1 tuned to 7 kHz is more than doubled compared with when a different tone is used first in the sequence (bottom row). Dark or light-gray polygons indicate recording sites tuned to 3 or 7 kHz±0.25 octaves, respectively. A, anterior; D, dorsal. Adapted from Zhou et al (2010).
To follow-up on the Zhou et al (2010) experiment, Panizzutti et al (under review) looked for structures in the frontal cortex that could be involved in the enhanced response to the predicted second tone. Rats were trained to recognize a target sequence of two pure tones among non-target two-tone sequences, as in the previous study. Unit and local field potential responses were recorded from the auditory and ventral orbital frontal cortices simultaneously, during presentation of the target and non-target stimuli. Panizzutti et al (under review) found marked θ and γ band oscillation in the ventral orbital cortex during the silence inter-tone interval when the animal was expecting the second tone in the target sequence but not in the non-target condition. These findings again highlight the distributed and dynamic nature of neural changes involved in learning and emphasize the feed-forward and feed-back networks involved in predictions about sensory events.
Three Guiding Principles Emerge from the Neuroscience
Taken in aggregate, these findings from basic systems neuroscience provide us with three guiding principles for the application of cognitive training to neuropsychiatrically impaired brains. We articulate each principle here, and provide a relevant example from current clinical research.
-
1)
The fundamental neural mechanisms that support learning-induced plasticity are in place throughout life and can be harnessed in the impaired brain. The adult brain is not a fixed and rigid system; most often, it has difficulty learning new behaviors due to competitive interference from prior learning successes. Adults have difficulty learning a new language because their primary language is stored in widely distributed, powerful, massively practiced cortical representations that compete with the formation of new language-based neural responses (Merzenich et al, 1991; Merzenich and DeCharms, 1996). This principle helps us to understand the catastrophic and enduring reorganization of cortical representations in neuropsychiatric patients who have experienced multiple episodes of maladaptive high-salience ‘learning events’ (see Figure 10 for a basic science example of this phenomenon, adapted from Wang et al, 1995). Though we do not yet fully understand how illness-related changes in neuroplasticity mechanisms affect the capacity of the impaired brain to respond to training, evidence from persistently ill schizophrenia patients indicates that even in this disabling condition, the brain is capable of significant behavioral and neural activation improvements after appropriate training (Haut et al, 2010; Subramaniam et al, in press).
Figure 10 Cortical reorganization can occur in maladaptive directions: monkeys trained to detect a bar contacting the second, third, and fourth finger simultaneously show a degraded and undifferentiated representation of those digits in somatosensory cortex (Wang et al, 1995); this degraded map leads to focal hand dystonia. Similar principles of maladaptive reorganization of somatosensory cortex underlie the development of phantom limb pain (Yang et al, 1994).
-
2)
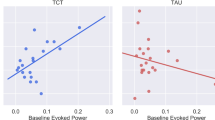
Training-induced enhancements in lower-level perceptual representations have a beneficial effect on higher-level cognitive operations. For example, as a monkey learns to perform a sensory-guided hand movement (eg, to retrieve a small object from a hidden cubby), areas that represent the relevant tactile, proprioceptive, and kinesthetic inputs in sensory cortex, and areas that represent motor planning and output zones of the frontal cortex, all develop more tightly coordinated oscillatory activity to reflect the newly trained hand movements. These practice-driven, coordinated neural networks feed forward and deliver a proportionately more salient and more coherent signal to downstream cortical and subcortical areas involved in prediction, association, encoding, and action control (Merzenich and DeCharms, 1996). Indeed, evidence from older adults shows that successful perceptual training induces more efficient and reliable prefrontal cortical operations, allowing for improved working memory performance (Berry et al, 2010; Gazzaley, 2010). Vinogradov et al have shown increases both in the amplitude of the M100 response in A1 and in very early γ band oscillatory power in lateral prefrontal cortex after intensive auditory training in schizophrenia, concomitant with improved behavioral performance (Dale et al, 2010; Brown et al, under review).
-
3)
Learning-induced plasticity is critically dependent on the behavioral state of the animal, and is profoundly influenced by neuromodulatory neurotransmitters. Cholinergic, dopaminergic, and noradrenergic neuromodulation are fundamental components of learning-induced plasticity in cortical systems (Kilgard and Merzenich, 1998; Bao et al, 2001; Roelfsema et al, 2010). Long-term plastic changes are induced when a behavior is closely attended and rewarded (ie, when the animal is ‘motivated’ to perform the behavior), but not when equivalent schedules of input or action events occur without the animal attending to them. In humans, inducing activation of midbrain regions containing dopamine neurons that project to hippocampus before learning (via monetary incentives) improves memory for events that follow the activation (Adcock et al, 2006). This principle indicates that training must be delivered in such a manner that the learner attends to every trial, and that trials must be delivered with both a sufficiently high reward schedule and a sufficiently challenging difficulty level so that the learner maintains motivation while improving performance. The abnormal neuromodulatory function seen in addictions, schizophrenia, ADD, major depression, and post-traumatic stress disorder (to name a few) likely has a direct effect on cortical plastic responses during learning, as do the medications commonly prescribed for these illnesses. In patients with schizophrenia, for example, higher levels of medication-induced anticholinergic burden adversely affect the response to cognitive training (Vinogradov et al, 2009).
NEUROPLASTICITY-BASED COGNITIVE TRAINING IN NEUROPSYCHIATRIC ILLNESSES
The neuroscience principles discussed above can be translated into specific therapeutic approaches for human disorders whose goal is to harness mechanisms of neuroplasticity and to drive meaningful neural representational change through implicit learning. The goal is to create a brain that is a more efficient learner with more finely tuned and accurate cognitive and affective processing and a better ability to engage in adaptive real-world behaviors. In this section, we delineate some of the key ‘active ingredients’ for a neuroscience-informed approach to cognitive training, and we highlight promising findings using this approach in several clinical populations.
Features of Neuroscience-Informed Cognitive Training Methods
Based on the findings we reviewed earlier, the critical active ingredients for a neuroscience-informed approach to cognitive training in an impaired brain would include the following features:
-
1)
Initial use of training to improve impaired perceptual processes and drive adaptive plastic changes in distributed brain systems of interest, followed by use of stimuli and tasks that support generalization to real-world environments. In other words, there must be precise engineering of stimuli and tasks in order to improve the speed and accuracy of relevant information processing throughout the targeted neural system(s), including lower and higher levels of processing. As extensively reviewed in Ahissar et al (2009), the past 15 years of research into human perceptual learning has unequivocally demonstrated that the specific features of a training protocol have a significant impact on the degree of improvement in a given task as well as the amount of generalization to untrained tasks. To summarize briefly, training that focuses in a blocked manner on a specific lower-level perceptual process (such as visual contrast discrimination) will induce profound improvements in performance, will show a high degree of specificity, and will only transfer if contrast discrimination is relevant to the new task. Training that focuses on a higher-level process, such as scene recognition, especially if delivered in an interleaved or ‘mixed stimuli’ manner, will show only moderate improvements in performance, will generalize to untrained similar tasks, but will be limited by the lower-level information available to the higher levels of operation. Any practice-induced improvements in higher-level discrimination between similar stimuli will be the result of a gradually gained access to more informative, lower-level populations (Ahissar and Hochstein, 2004)—either through a successful ‘back-tracking search’ from higher-level operations (Figure 11a) and/or through massive training of all of the relevant lower-level inputs (Figure 11b). Thus, sensory stimuli used during an initial period of cognitive training for an impaired brain should be exaggerated or emphasized relative to naturalistic stimuli in order to make initial levels of the task easier—in other words, in order to improve the access of potentially impaired higher-level operations to appropriate informative lower-level neural representations (see Lee and Park, 2006; Javitt et al, 2007 for two studies showing that working memory performance can be enhanced in schizophrenia by increasing the sensory salience of the cue). The initial phases of lower-level and mid-level training should focus on the range of processes that contribute to the higher-level operation(s) of interest (Figure 11b). For instance, a social cognition training program might focus initially on blocked exercises designed to improve contrast sensitivity, visual selective attention, visuospatial working memory, and eye-gaze detection, in order to train the learner to generate and maintain strong and accurate lower-level cortical representations of visually informative facial details. As training progresses, performance improves, and the learner becomes more ‘expert’ at processing visual information from the human face, the learner might be provided with higher-level exercises that focus on recognizing facial emotion, identifying changes in facial expression, and interpreting social interactions. In other words, stimuli and tasks are modified to have gradually increasing degrees of spatiotemporal detail, higher degrees of naturalistic appearance, and greater ecological validity, to ensure that training generalizes to real-world situations.
Figure 11 Learning across a distributed neural system can be conceptualized as occurring across hierarchical ‘levels.’ For illustrative purposes only, three levels are shown schematically, ranging from lower-level perceptual representations, to explicit higher-order perceptions and operations, to global high-level ecologically meaningful cognitions and contexts. Mid-level and higher-level representations are influenced by the quality of lower-level perceptual processing, just as pre-attentive perceptual processing is biased or influenced by higher-level predictions and expectancies. (a) During an initial learning phase, higher-level neural representations are strengthened, as the prefrontal cortex orients toward the task at hand, and very few plastic changes occur at lower levels. With sufficient intensive practice, in a healthy brain, plastic changes can propagate backwards from these higher-level representations, resulting in strengthened accuracy and fidelity of processing at lower-levels of the system (eg, the wine expert who is able to taste and identify a very wide range of flavors). In an impaired brain, distortions or limitations at any level will create bottlenecks for learning-induced widespread adaptive changes. (b) If training of sufficient intensity and duration progresses on specific sets of informative lower-level and middle-level stimuli and tasks, plastic changes will feed forward to improve the representational fidelity of information at higher levels, and learning will be partially transferred to higher-level contexts that use the trained lower-level features. Adapted and modified from Ahissar et al (2009).
-
2)
Highly intensive training schedules of carefully controlled and constrained learning events along with individualized adaptation of task difficulty to drive learning and preserve reward schedules. The relevant ‘skills’ (or sets of skills, or component processes) must be identified, isolated, then practiced through hundreds if not thousands of trials on an intensive (ie, quasi-daily) schedule (Roelfsema et al, 2010). Difficulty level must begin at a level where the impaired brain is able to perform with success; it then must be parametrically modified (more complex stimuli, shorter stimulus presentation, higher working memory load, etc.) in an appropriate manner to drive the learner to higher and higher levels of performance over multiple trials. Individualized adaptation of task difficulty ensures that learning trials progress under carefully controlled conditions tailored to the unique capacities of each learner; simultaneously, this maintains a high trial-by-trial reward schedule, improving the brain's ability to engage in successful predictions. As an example, children with anxiety show an attention bias toward threat-related cues. Exercises could be designed to disengage attention from threat cues (eg, angry faces) and focus it on other targets; the goal would be increasingly accurate disengagement at speed from threat stimuli being presented for shorter durations. This in turn would allow prefrontal cortical regions to reduce their expectancy bias toward social threat in the environment, reducing the child's anxiety level (see Bar-Haim et al, 2011). Well-designed training is thus based on: first, precisely defining the specific set of skills to be trained so that the desired generalization will occur, and second, delivering the training with sufficient intensity and duration. For example, Nishi and Kewley-Port found that training Japanese speakers on the entire set of English vowels subsequently generalized across context to other words and speakers, whereas training on a subset of vowels did not (Deiber et al, 2007). Burk and Humes gave subjects either short (5 h) or long (15 h) training on the identification of words in noise, and found that the long but not the short training generalized from isolated words to fluent speech (Molinuevo et al, 2011).
-
3)
Frequent and repetitive engagement of selective attention and reward systems in the brain, and consideration of the psychopharmacologic state of the learner. In order to maximize enduring plastic changes in cortex, the learner must attend to each trial or learning event on a trial-by-trial basis and a very high proportion of the learning trials must be rewarded immediately (rather than at the end of a block of trials or on a trial-and-error basis) (Buonomano and Merzenich, 1998; Beitel et al, 2003; Blake et al, 2006; Roelfsema et al, 2010). The immediate and repeated release of neuromodulators engaged by a dense schedule of successfully predicted learning events is required to drive enduring brain plasticity. In addition, the goal must be to develop training—or a context for the training—that is entertaining, engaging, and motivating for the learner. Finally, though very little research has been done in this area, there is no doubt that medications with effects on dopaminergic, noradrenergic, serotonergic, and cholinergic modulation will influence plasticity mechanisms in ways that we will need to account for as we design more sophisticated training protocols (Vinogradov et al, 2009).
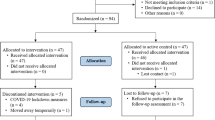
Neuroscience-Informed Cognitive Training: Current Findings
Neuroscience-informed cognitive training based on the three features listed above was first investigated using a computerized auditory processing training program for individuals with language-based learning disabilities (LLD) over 10 years ago (FastForword, Scientific Learning). Two laboratory studies as well as a field study of 500 LLD children who underwent 40 h of training demonstrated significant improvement in language-related cognition and verbal memory in subjects who performed the training but not in control groups (Tallal et al, 1996). MEG studies demonstrated that early cortical representations of auditory inputs were enhanced after training as compared with baseline (Hayes et al, 2003), while functional MRI revealed that the abnormal response patterns during key language tasks seen in both child and adult LLD patients was restored to more normal patterns with training (Temple et al, 2003).
More recent work with neuroscience-informed cognitive training is summarized in Table 5. Mahncke et al (2006a) investigated a training program designed similarly to the LLD studies, but constructed specifically for aging adults, with the goal of intensively training low-level auditory processing and auditory/verbal working memory in order to partially reverse normal age-related losses in verbal memory. Training (40–50 h) focused heavily on auditory perceptual processes and auditory/verbal working memory, with a small amount of training in ecologically meaningful whole-language tasks. Significant improvements were found in the active training group in measures directly related to the training (eg, auditory processing speed) as well as untrained measures of verbal memory, indicating generalization of the training effects, while no such improvements were seen in either active control or no-contact control groups. Memory enhancement was sustained after a 3-month no-contact follow-up (Mahncke et al, 2006b). In a multisite RCT of 487 older adults with this same software training for 40 h, similar improvements were found with an effect size of 0.3 for verbal memory and 0.87 for processing speed in an intent-to-treat analysis (Smith et al, 2009). These two independently conducted, tightly controlled studies using a well-defined neuroscience-informed cognitive training protocol demonstrate clinically significant effect sizes, durability of effects, and indicate that the verbal memory decline of aging may be partially reversible in response to intensive training of lower-level auditory processing and auditory/verbal working memory operations.
The ACTIVE multisite RCT of 2802 older adults compared 10 h of computerized visual speed of processing training (‘Useful Field of View’) vs 10 h of therapist-guided training in a group format in reasoning or in memory techniques. The initial cognitive outcomes showed an effect size of 1.46. More impressively, in independently conducted analyses of long-term follow-up data, there were fewer medical expenditures, less depression, a delay in driving cessation, and better self-rated health in those who received the perceptual speed of processing training compared with those who received direct instruction training (Edwards et al, 2009; Wolinsky et al, 2009a, 2009b, 2010). These studies indicate that intensive perceptual training in older adults shows a gradual generalization to improved real-world functioning over a 5-year period, but that therapist-guided strategy coaching for problem solving or memory does not. We hypothesize that the feed-forward effects of improved perceptual abilities drove enduring adaptive plastic changes in distributed higher-level operations in these at risk older adults, as per Figure 11b.
Vinogradov's group performed interim analyses on a double-blind RCT of 50 h (10 weeks) of neuroplasticity-based cognitive training for auditory/verbal learning deficits as a stand-alone treatment in 55 middle-aged adults with persistent schizophrenia. They applied 50 h of a research version of the software described above in the Mahncke et al study and compared it with 50 h of commercial computer games, examining behavioral outcomes as well as changes in serum biomarkers, MEG indices of early neural processing, and fMRI patterns of activation during untrained memory tasks (Adcock et al, 2009; Fisher et al, 2009, 2010; Dale et al, 2010; Hinckley et al, under review; Subramaniam et al, in press). Schizophrenia participants showed significant improvement in verbal learning and memory and in general cognition in response to training (effect sizes of 0.86 in a per protocol analysis); cognitive improvements were associated with improved quality of life at 6 months; subjects exposed to training showed significant increases in serum BDNF levels, while computer games control subjects did not; medication-induced serum anticholinergic activity was negatively correlated with the cognitive response to training; training increased resting-state α band functional connectivity in cortex; and also increased BOLD activation patterns in medial prefrontal cortex during an untrained memory task and restored the association between level of activation and task performance. More compellingly, training-induced increases in prefrontal activation were associated with improved ratings of social functioning 6 months later. Keefe et al (in press) performed a double-blind multisite feasibility study using 40 h (over 8–12 weeks) of the same software in 47 subjects with schizophrenia and found an effect size of 0.69 in verbal learning after 20 h of training, and 0.39 after 40 h of training. (Differences in study methods with the Fisher et al report include fewer hours of training delivered over a longer time period, the addition of a therapist coaching ‘bridging group’ component, an intent-to-treat analysis on all enrolled participants vs a per protocol analysis on all study completers; and differences in definition of cognitive outcome variables: z-scores from MATRICS-derived measures vs T-scores from MCCB-defined domains.) Despite some differences in design and magnitude of cognitive change, these two tightly controlled double-blind studies using a well-defined cognitive training protocol based on the neuroscience principles described earlier demonstrate that patients with schizophrenia who have been ill for 20 years can still mount a positive response to intensive training, with improvements in verbal learning and memory. The Fisher et al follow-up study suggests that subjects who respond to training show generalization to real-world quality of life improvements 6 months later (Fisher et al, 2010). Haut et al performed an RCT with 21 schizophrenia patients who received 25 h of intensive computerized training in attention and working memory (CogPack Marker Software) plus training in verbal and picture N-back tasks (training followed some but not all of the neuroscience-informed elements described above); participants were compared with subjects receiving group-based social skills training. An effect size of 0.89 in verbal working memory and 1.4 in picture working memory was found, as well as increased fMRI activation in dorsolateral prefrontal cortex, anterior cingulate and frontopolar cortex (with correlations between improved performance and increased activation in a subset of regions) (Haut et al, 2010). Together with the data from Vinogradov's laboratory, these findings indicate that (1) after intensive training, individuals with schizophrenia can show significant plasticity in distributed cortical systems, with activation patterns appearing more similar to those of healthy individuals than they did at baseline and (2) training-induced increases in cortical activation are correlated with improvements in behavioral performance. These findings should help to address some of the therapeutic nihilism that has characterized the field of schizophrenia treatment research.
Klingberg et al (2005) performed a multicenter double-blind RCT of 17 h of intensive computerized visuospatial working memory training based explicitly on the neuroscience principles described earlier. Fifty-three children with ADD trained for 40 min a day over a 5-week period (20 days), and 42 were evaluated at follow-up 3 months later. A significant improvement from baseline to post-intervention on an untrained visual working memory task was found in the treatment group compared with the comparison group in a per protocol analysis (effect size of 0.93 at post-intervention, and 0.92 at 3 months follow-up). Significant treatment effects were also observed on measures of response inhibition, complex reasoning, and verbal working memory, indicating generalization of training. Significant decreases in parent-rated symptoms of inattention and hyperactivity/impulsivity were seen at post-intervention and at 3 months follow-up. Klingberg (2010) also performed imaging studies in healthy subjects that demonstrate changes in frontoparietal activation patterns as an effect of training, a possible basis for generalization of training between different working memory tasks. He found that after 5 weeks of training, the increase in working memory capacity for each subject was positively correlated with changes in cortical D1 receptors, suggesting that training was associated with an increase in endogenous dopamine release and that training may improve capacity partly by tuning dopaminergic transmission (as would be predicted by the basic science). Rabiner et al (2010) have examined the positive behavioral effects of 28 h of computerized attention training in children with ADD based in part on the principles described earlier, while Hoekzema et al (2010) have demonstrated behavioral gains plus enhanced activity in frontal and cerebellar networks after a 10-day trial of cognitive training in unmedicated children with ADD. Taken together, these data indicate that working memory impairments in ADD respond to intensive training, and that the most robust and sustained effects to date are seen from the Klingberg et al group, who explicitly designed their training based on harnessing neuroplasticity mechanisms in the brain.
Three other recent interesting studies deserve mention as they have been based at least in part on the neuroscience principles described earlier. Bickel et al (2011) performed a trial with 27 adults receiving treatment for stimulant use, with the aim of targeting delay discounting in substance-abusing adults. His hypothesis was that an improvement in working memory function would improve impairments in delay discounting, and that this could have implications for real-world addictive behavior. Participants were randomly assigned to receive computerized working memory training (PSS Cog Rehab) or a ‘sham’ control training experience (no learning progression) using a yoked experimental design. The training that each subject received was not specified (in terms of session content or duration) but appears to have had some of all three of the features described earlier (simplified stimuli, intensive training, frequent and repetitive engagement of attention and reward systems); training was given for 9–44 days (an average of 25 days). Rates of discounting of delayed rewards were significantly reduced by about 50% among those who received working memory training but were unchanged in those who received the control condition. This study supports the notion that neuroscience-informed training can be used to target the impairments that underlie impulse dyscontrol and executive dysfunction in people with addictions. Hopkins et al (2011) performed a well-controlled RCT of 5 h of computerized training in eye-gaze detection and facial emotion recognition in 49 children with autism and saw improvements in the trained domains, as well as improved social interactions in a natural environment, indicating that improvements in relatively low-level and mid-level processing of facial features and emotions can show real-world generalization of effects. Bar-Haim et al (2011) performed a randomized placebo-controlled trial of computerized training for threat-related attention biases in 34 highly anxious 10-year old children (four 1-h sessions on 4 different days over a 2-week period). They found that training facilitated attention disengagement from threat cues and reduced state anxiety during a stressor task, suggesting that it could be beneficial for reducing stress vulnerability in anxious children. These latter two studies in children show that repetitive training (implicit learning) that focuses on relatively lower-level impairments can result in clinically meaningful generalized improvements in real-world behavior and affect. Taken together, this emerging body of work underscores the extremely high clinical potential of carefully constructed cognitive training that is based on an understanding of systems neuroscience. Indeed, active research is underway in TBI, PTSD, bipolar illness, substance abuse, and anxiety disorders.
FUTURE RESEARCH DIRECTIONS
While the emerging data are very promising, much important work remains to be done. Our understanding of how to deliver ‘neural systems’ training with optimal efficiency and efficacy to individuals with impaired neurocognition is in its infancy. We are at the place that physical fitness training was 100 years ago—we know that it is good to run and lift weights, but we do not yet grasp the nuances of how to tailor a maximally efficient training program that targets an individual person's unique strengths and weaknesses. In this section, we present some of the exciting and challenging areas for future research in this area.
We Must Improve Our Understanding of the Neural Mechanisms that Underlie Successful Training
Perhaps the most basic challenge is for cognitive neuroscience to develop a more sophisticated understanding of pre-attentive processing and implicit learning mechanisms in health and disease and their relationship to higher-order cognitive operations in humans such as working memory, declarative memory, cognitive control, emotion regulation, delay discounting, and problem solving; we must also investigate the ways in which this relationship can be exploited in order to design the most efficient and successful forms of training possible.
Another key challenge is to more fully understand the specific training methods that promote maximal gains in the impaired brain—the exact intensity and duration of training, to what degree there must be a focus on perceptual and pre-attentive processing, whether and how competitive interference occurs during training, and the training modalities that promote generalization across cortical sectors and across behaviors. Dose–response curves must be generated for specific sets of exercises that target specific neural system impairments in specific clinical populations. Studies must be designed to control for common confounds: some of these include participant selection bias; effects of uncontrolled exposure to social reinforcers or psychosocial therapies; lack of ‘blinds’ for participants and personnel performing assessment procedures; inconsistent definitions of outcome variables and analytic approaches. Method development must be coincident with investigation of the brain's responses to training, during both early and late phases of learning as well as weeks or months after cessation of training. Future studies must employ well-defined neurological outcome measures based on EEG, MEG, and fMRI methods (eg, as championed by the CNTRICS initiative (Cognitive Neuroscience Treatment Research to Improve Cognition in Schizophrenia; Carter et al, 2011))—preferably with a sophisticated analysis of the precise timing and changes in neural oscillatory patterns that support successful learning, as well as the changes in functional connectivity that occur as a result of treatment and that are related to improvements in real-world behavior.
We Must Improve Our Development of Training Content
In addition to these improvements in our understanding of optimal neuroplasticity-based cognitive training methods, our field must move forward to develop improved training content that is based on experimental evidence of the neural system dysfunctions that are relevant to neuropsychiatric disorders. Our field awaits the development and evaluation of carefully designed cognitive exercises that adaptively train cognitive control, delay discounting, emotion regulation, source memory, self-referential processing, and social cognition, to name just a few. Ideally, randomized controlled trials will be conducted to identify the necessary and sufficient domains of training, and the optimal sequence of training (critical sets and ordering of exercises) for specific profiles of dysfunction and will examine their generalization to real-world demands in order to develop the most efficient treatment approaches possible. We emphasize that exercises will need to be developed to target neural system dysfunction in critical cognitive/affective processing domains, rather than to target specific diagnoses. Any given set of exercises might be useful across multiple disorders—social cognition training, for example, would be important in schizophrenia and autism, while training in delay discounting would be important in addictions and impulse control disorders.
Additionally, evidence from basic neuroscience (Berridge, 2004; Barch, 2005; Huitt and Cain, 2005; Adcock et al, 2006) indicates that motivation, rewards, and learning are intimately linked, and this association can be exploited for therapeutic purposes in well-designed exercises. For example, the Klingberg et al (2005) and Bickel et al (2011) control groups did the exact same exercises as the active training group, but with no progression in difficulty and thus no rewards—and they showed no cognitive improvements. Adcock and colleagues have recently shown that motivation to obtain reward in humans is instantiated by a transfer of information from the DLPFC to the nucleus accumbens and VTA (Ballard et al, 2011); dopaminergic neuromodulation via activation of these reward pathways is critical for increasing the salience of stimuli or actions (incentives) that promote learning (Berridge and Robinson, 2003). Training that drives prefrontal cortex to create strong and predictable associations between successful learning events and rewards will not only lead to stronger learning, but may also improve the functioning of the distributed neural system related to incentive salience and motivation. Similarly, disturbances in working memory are related to impaired motivation, presumably because they impede the ability to represent goal or reward information (Berridge, 2004); thus, training that focuses on working memory (perhaps especially on affective working memory) and reward representation could have beneficial effects on motivated behavior. Indeed, the Bickel et al (2011) study represents a first foray into this area. Future research must determine to what extent these various cognitive training approaches translate into meaningful improvements in patients’ motivated behavior in the real world.
We Must Improve Our Understanding of the Factors that Influence the Response to Training
Our field must learn to characterize the relationship between an individual patient's characteristics at baseline—including genetic factors, developmental stage, possible neurophysiologic biosignatures, and neurocognitive profile—and their ability to make and retain benefits from neuroplasticity-based cognitive training (Bell et al, 2003; Fiszdon et al, 2005; Bosia et al, 2007). For instance, a small study found that schizophrenia patients with the catechol-O-methyl transferase Met (COMT) allele made greater gains in cognitive flexibility after computerized cognitive training than patients without the Met allele, while Vinogradov et al have preliminary data indicating that polymorphisms in the COMT gene may be associated with cognitive gains after training (Bosia et al, 2007; Panizzutti et al, under review). This group has also found that baseline α band resting-state functional disconnectivity in key cortical regions in schizophrenia predicted the response to cognitive training (Hinckley et al, under review), while Klingberg et al have found that lower activation patterns in DLPFC are associated with greater cognitive improvement after training in ADD patients (personal communication). In healthy subjects, it has been shown that an individual's intrinsic neural dynamics affects their rate of learning and the nature of their learning-induced neural response patterns (Vernon et al, 2003; Mukai et al, 2007; Hickok et al, 2011). A better understanding of the relationship between an individual's underlying genetics, neurobiology, and developmental stage and their ability to benefit from cognitive training will permit an evidence-based adaptation of programs to a broader range of clinical needs.
We must also examine the ways that commonly prescribed medications with anticholinergic and antidopaminergic effects—as well as those with noradrenergic and serotonergic effects—can influence the response to plasticity-based cognitive training. As noted earlier, Vinogradov et al (2009) have shown that the amount of serum anticholinergic activity assessed in patients with schizophrenia via radioreceptor assay (due to their medications) is inversely correlated with the overall improvement in cognition seen in these patients after 50 h of neuroplasticity-based auditory training. It is naive to believe that the standard current psychopharmacologic armementarium is without impact on the brain's ability to engage in successful learning (see also the implications of Klingberg, 2010) findings on dopamine receptor changes during successful training).
Similarly, as our field eagerly turns to the promise of cognitive-enhancing medications, we must be prepared to explore the most advantageous ways in which these agents can—and probably should—be combined with training in order to optimize cognitive gains in patients (Keefe et al, 2010). Again, it is probably naive to assume that administering such agents in a behavioral vacuum to patients will, absent any engagement of the brain in new and adaptive learning events, result in significant functional gains. Indeed, some agents may be of no value when given alone, but may substantially facilitate the effects of cognitive training.
Medications are not the only possible adjuvants to enhance the brain's response to cognitive training. The use of transcranial magnetic stimulation (TMS) and direct current stimulation (tDCS), in combination with sensory stimulation, have both shown to be inducers of cortical plasticity (Celnik et al, 2009; Khedr et al, 2010). Anecdotal reports suggest that these methods may improve working memory (Jo et al, 2009), attention (Kang et al, 2009), and aphasia (Monti et al, 2008) in stroke patients. Pascual-Leone's group showed that when a night with sleep follows rTMS to M1, the capacity to induce subsequent plasticity in M1 is enhanced (Cohen et al, 2010). Exercise is another potent, safe, and valuable ‘neurotrophic agent’ that could be combined in innovative ways with cognitive training regimens to maximize a patient's response to treatment (see Pajonk et al, 2010).
We Must Translate Cognitive Training into Meaningful Interventions that Change People's Lives
No cognitive training program, however precisely engineered, can substitute for meaningful and developmentally appropriate psychosocial rehabilitation for people with serious neuropsychiatric illness. Evidence from the educational field, including electrophysiologic data, indicate that beliefs can influence learning success through top–down biasing of attention and conceptual processing toward goal-congruent information (Mangels et al, 2006). Vinogradov et al have early results indicating that schizophrenia participants who believe that intelligence is malleable show better cognitive outcomes after computerized training than those who believe it is a fixed entity, even though they were blind to group assignment and even after controlling for baseline cognition and number of hours of training (unpublished data). We predict that beliefs, expectations, and self-representations will turn out to have powerful neurobiologic influences on the brain's ability to make use of cognitive training and will be another therapeutic leverage point that can be purposefully harnessed to maximize treatment response. Indeed, prior research has already shown, at least in schizophrenia, that integration of cognitive remediation with other psychosocial treatments provides significant synergistic benefits (McGurk et al, 2007; Wykes et al, 2011). As a corollary, we predict that cognitive neurotherapeutic approaches that explicitly and continuously demonstrate to patients their ongoing cognitive improvements will challenge their assumptions about the chronic, fixed nature of their impairments. Future work can explore whether this approach helps patients to develop more adaptive internalized beliefs about their capacity for change, and whether it increases motivation and engagement with the larger therapeutic learning environment (Meltzoff et al, 2009).
Finally, and perhaps most ambitiously, we believe that the greatest gains will occur when neuroplasticity-based restorative cognitive training is implemented in conjunction with early detection and intervention in young people who are in the very earliest phases of clinical expression of a neuropsychiatric illness. In schizophrenia, for example, neuropsychological data indicate unequivocally that cognitive deficits are found in prodromal and ‘first-episode’ individuals; these deficits appear to worsen as the individual progresses into the illness and predict functioning several years later (Brewer et al, 2005; Keefe et al, 2006). Vinogradov et al (unpublished data) have demonstrated that neuroplasticity-based cognitive training can be successfully delivered to young early psychosis individuals at home via laptop, with significant improvements in cognition. These young patients have not yet experienced the repeated psychotic episodes that induce catastrophic cortical reorganization and that impede psychosocial development, and have not yet been subjected to years of anticholinergic and antidopaminergic medication. Successful cognitive training may thus result in enduring gains in these individuals and may go a long way to significantly improving their clinical outcomes. It is certainly conceivable that well-designed and thoughtfully applied training for impaired neural system functioning, when applied early, could normalize some of the aberrant neurodevelopmental trajectories that characterize mental and addictive disorders, and could pre-empt the full-blown expression of a chronic and deteriorating illness. Much the way we vigorously treat amblyopia in very young children by ‘forcing’ the lazy eye to work, we can envision a day when we ‘force’ impaired distributed neural systems to become strengthened through appropriate training.
CONCLUSION
Though we have focused this review on the impaired brain, it is obvious that many of the principles we have outlined are applicable to improving the cognitive processing capacities of healthy brains as well. As such, carefully designed cognitive training exercises will undoubtedly promote neuroresilience in healthy individuals, much the way that physical fitness training promotes cardiovascular and immune system resilience. Neuroresilience may encompass not only improved ‘resistance’ to the cognitive effects of aging (as already shown in the ACTIVE study), and to various processes associated with the dementias, but also to physical and psychological stressors, such as sleep deprivation, emotional trauma, cognitive or affective loading, and changing social demands.
It is not surprising—in fact, it is inevitable—that the science behind our understanding of how to develop effective training is occurring in parallel with the development of extremely sophisticated entertainment software that is already engaging millions—perhaps hundreds of millions—of brains of all ages in learning experiences with cognitive and affective impact. These advances in entertainment software indicate that cognitive training can be developed that will generate the same interest, engagement, perceived value, and social acceptability as web-based games. Indeed, novel collaborative efforts are already underway to join technological expertise from the entertainment software industry with neuroscience efforts aimed at improving performance in neural systems. The likely outcomes will be browser-based treatment tools available on a scale never before imagined for any other therapeutic intervention—‘neural network treatments’ that not only engage inherent brain reward mechanisms through their entertainment value, but that also allow the learner to ‘neurally network’ with other learners and participate in a socially rewarding and developmentally appropriate therapeutic activity that is free of stigma.
We began this review by pointing out that successful cognitive training for neuropsychiatric illnesses will need to induce specific and substantial distributed changes in cortical and subcortical representations and will need to be delivered in a scalable and developmentally appropriate manner that is engaging and motivating. The science we have reviewed here describes key steps to accomplish the former goal. We will be limited only by our creativity and imagination in accomplishing the latter.
FUTURE RESEARCH ISSUES
Improve Our Understanding of Fundamental Mechanisms in Order to Design the most Efficient and Successful Forms of Training
-
Develop a more sophisticated understanding—in health and disease—of the interaction between implicit learning mechanisms and higher-order cognitive operations in humans such as working memory, declarative memory, and cognitive control.
-
Investigate the specific training methods that promote maximal gains in the impaired brain—the exact intensity and duration of training, to what degree there must be a focus on perceptual processing, and the training modalities that promote generalization.
-
Examine the brain's responses to training, both within early and later phases of learning—preferably with a sophisticated analysis of the precise timing and neural oscillatory patterns that support successful learning, as well as the changes in functional connectivity that occur as a result of treatment and that are related to improvements in real-world behavior.
Improve Our Development of Training Content
-
Develop and test cognitive training exercises using an evidence-based approach to known neural system dysfunctions relevant to neuropsychiatric disorders.
-
Explore the neural systems linking motivation and cognition in order to exploit this association for therapeutic purposes; determine the appropriate methods of enhancing reward representation during training and explore transfer to real-world functioning.
Improve Our Understanding of the Factors that Influence the Response to Training
-
Characterize the relationship between an individual patient's status at baseline—including genetic factors, developmental stage, possible neurophysiologic biosignatures, and neurocognitive profile—and their ability to make and retain benefits from neuroplasticity-based cognitive training.
-
Examine the ways that commonly prescribed medications with anticholinergic, antidopaminergic, noradrenergic, and serotonergic effects can influence plasticity-based neurocognitive improvement.
-
Explore the most advantageous ways in which cognitive-enhancing agents can—and probably should—be combined with training in order to optimize cognitive gains in patients.
-
Study other adjuvants to enhance the brain's response to cognitive training, such as TMS, tDCS, and exercise.
Translate Cognitive Training into Meaningful Interventions that Change People's Lives
-
Discover the manner in which cognitive training can best be combined with meaningful and developmentally appropriate psychosocial rehabilitation for people with serious neuropsychiatric illness. Explicitly foster beliefs, expectations, and representations that enhance the response to training.
-
Implement neuroplasticity-based cognitive training in conjunction with early detection and intervention in young people who are in the very earliest phases of clinical expression of a neuropsychiatric illness; focus on pre-empting the full-blown expression of a chronic and deteriorating illness.
-
Investigate novel and creative ways in which cognitive training can be combined with entertainment software to create scalable web-based treatment tools; ideally such ‘neural network treatment tools’ will not only engage inherent brain reward mechanisms through their entertainment value, but will also allow the learner to ‘neurally network’ with other learners and participate in a socially rewarding and developmentally appropriate therapeutic activity that is free of stigma.
References
Adcock RA, Dale C, Fisher M, Aldebot S, Genevsky A, Simpson GV et al (2009). When top-down meets bottom-up: auditory training enhances verbal memory in schizophrenia. Schizophr Bull 35: 1132–1141.
Adcock RA, Thangavel A, Whitfield-Gabrieli S, Knutson B, Gabrieli JD (2006). Reward-motivated learning: mesolimbic activation precedes memory formation. Neuron 50: 507–517. This study was one of the first to demonstrate that meso-limbic activation induced by reward anticipation precedes successful memory formation in humans.
Ahissar M, Hochstein S (2004). The reverse hierarchy theory of visual perceptual learning. Trends Cogn Sci 8: 457–464.
Ahissar M, Nahum M, Nelken I, Hochstein S (2009). Reverse hierarchies and sensory learning. Philos Trans R Soc Lond B Biol Sci 364: 285–299.
Airaksinen E, Wahlin A, Forsell Y, Larsson M (2007). Low episodic memory performance as a premorbid marker of depression: evidence from a 3-year follow-up. Acta Psychiatr Scand 115: 458–465.
Akiyama T, Kato M, Muramatsu T, Maeda T, Hara T, Kashima H (2008). Gaze-triggered orienting is reduced in chronic schizophrenia. Psychiatry Res 158: 287–296.
Anjana Y, Khaliq F, Vaney N (2010). Event-related potentials study in attention deficit hyperactivity disorder. Funct Neurol 25: 87–92.
Antila M, Partonen T, Kieseppa T, Suvisaari J, Eerola M, Lonnqvist J et al (2009). Cognitive functioning of bipolar I patients and relatives from families with or without schizophrenia or schizoaffective disorder. J Affect Disord 116: 70–79.
Aou S, Woody CD, Birt D (1992). Increases in excitability of neurons of the motor cortex of cats after rapid acquisition of eye blink conditioning. J Neurosci 12: 560–569.
Arias-Carrion O, Stamelou M, Murillo-Rodriguez E, Menendez-Gonzalez M, Poppel E (2010). Dopaminergic reward system: a short integrative review. Int Arch Med 3: 24.
Arlinger S, Lunner T, Lyxell B, Pichora-Fuller MK (2009). The emergence of cognitive hearing science. Scand J Psychol 50: 371–384.
Arts B, Jabben N, Krabbendam L, van Os J (2008). Meta-analyses of cognitive functioning in euthymic bipolar patients and their first-degree relatives. Psychol Med 38: 771–785.
Aupperle RL, Melrose AJ, Stein MB, Paulus MP (2011). Executive function and PTSD: disengaging from trauma. Neuropharmacology (e-pub ahead of print 22 February 2011).
Axmacher N, Cohen MX, Fell J, Haupt S, Dumpelmann M, Elger CE et al (2010). Intracranial EEG correlates of expectancy and memory formation in the human hippocampus and nucleus accumbens. Neuron 65: 541–549. This study used intracranial EEG from the hippocampus of epilepsy patients and from the nucleus accumbens of depressed patients to show that unexpected (unpredicted) stimuli enhance a late potential from hippocampus that predicts successful encoding; the nucleus accumbens shows a late potential which increases in magnitude during unexpected items, but with no subsequent memory effect.
Ballard IC, Murty VP, Carter RM, Macinnes JJ, Huettel SA, Adcock RA (2011). Dorsolateral prefrontal cortex drives mesolimbic dopaminergic regions to initiate motivated behavior. J Neurosci 31: 10340–10346.
Balu DT, Coyle JT (2011). Neuroplasticity signaling pathways linked to the pathophysiology of schizophrenia. Neurosci Biobehav Rev 35: 848–870.
Bao S, Chan VT, Merzenich MM (2001). Cortical remodelling induced by activity of ventral tegmental dopamine neurons. Nature 412: 79–83. The first experiment to show the potent stimulus-specific, long-lasting and asymmetrical effects of dopamine release on cortical maps when paired with simple sensory inputs.
Bao S, Chang EF, Woods J, Merzenich MM (2004). Temporal plasticity in the primary auditory cortex induced by operant perceptual learning. Nat Neurosci 7: 974–981.
Barch DM (2005). The relationships among cognition, motivation, and emotion in schizophrenia: how much and how little we know. Schizophr Bull 31: 875–881.
Bar-Haim Y, Morag I, Glickman S (2011). Training anxious children to disengage attention from threat: a randomized controlled trial. J Child Psychol Psychiatry 52: 861–869.
Barnes DE, Covinsky KE, Whitmer RA, Kuller LH, Lopez OL, Yaffe K (2009). Predicting risk of dementia in older adults: the late-life dementia risk index. Neurology 73: 173–179.
Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Brown CR, Heaven PC (2009). Event-related potentials in adults with Attention-Deficit/Hyperactivity Disorder: an investigation using an inter-modal auditory/visual oddball task. Int J Psychophysiol 71: 124–131.
Batty M, Meaux E, Wittemeyer K, Roge B, Taylor MJ (2011). Early processing of emotional faces in children with autism: an event-related potential study. J Exp Child Psychol 109: 430–444.
Baune BT, Miller R, McAfoose J, Johnson M, Quirk F, Mitchell D (2010). The role of cognitive impairment in general functioning in major depression. Psychiatry Res 176: 183–189.
Beitel RE, Schreiner CE, Cheung SW, Wang X, Merzenich MM (2003). Reward-dependent plasticity in the primary auditory cortex of adult monkeys trained to discriminate temporally modulated signals. Proc Natl Acad Sci USA 100: 11070–11075.
Bell M, Bryson G, Wexler BE (2003). Cognitive remediation of working memory deficits: durability of training effects in severely impaired and less severely impaired schizophrenia. Acta Psychiatrica Scandinavica 108: 101–109.
Bellucci DM, Glaberman K, Haslam N (2002). Computer-assisted cognitive rehabilitation reduces negative symptoms in the severely mentally ill. Schizophr Res 59: 225–232.
Bengtsson SL, Nagy Z, Skare S, Forsman L, Forssberg H, Ullen F (2005). Extensive piano practicing has regionally specific effects on white matter development. Nat Neurosci 8: 1148–1150.
Berridge KC (2004). Motivation concepts in behavioral neuroscience. Physiol Behav 81: 179–209.
Berridge KC, Robinson TE (2003). Parsing reward. Trends Neurosci 26: 507–513.
Berry AS, Zanto TP, Clapp WC, Hardy JL, Delahunt PB, Mahncke HW et al (2010). The influence of perceptual training on working memory in older adults. PLoS One 5: e11537. This study used EEG to evaluate older participants before and after intensive visual perception training, and showed that training-induced modifications in early visual processing during stimulus encoding predicted working memory accuracy improvements. These findings demonstrate the strength of the perceptual discrimination training approach by offering clear psycholophysical evidence of transfer-of-benefit and neural evidence of functional plasticity in older adult brains underlying the cognitive improvement.
Bickel WK, Yi R, Landes RD, Hill PF, Baxter C (2011). Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry 69: 260–265.
Blake DT, Heiser MA, Caywood M, Merzenich MM (2006). Experience-dependent adult cortical plasticity requires cognitive association between sensation and reward. Neuron 52: 371–381. Demonstrates that training-specific cortical reorganization during perceptual learning only occur if the participant has a reliable perception of the stimulus seeked (rewarded target).
Bora E, Yucel M, Pantelis C (2009). Cognitive functioning in schizophrenia, schizoaffective disorder and affective psychoses: meta-analytic study. Br J Psychiatry 195: 475–482.
Bora E, Yucel M, Pantelis C (2010). Neurocognitive markers of psychosis in bipolar disorder: a meta-analytic study. J Affect Disord 127: 1–9.
Bosia M, Bechi M, Marino E, Anselmetti S, Poletti S, Cocchi F et al (2007). Influence of catechol-O-methyltransferase Val158Met polymorphism on neuropsychological and functional outcomes of classical rehabilitation and cognitive remediation in schizophrenia. Neurosci Lett 417: 271–274.
Boutros NN, Gelernter J, Gooding DC, Cubells J, Young A, Krystal JH et al (2002). Sensory gating and psychosis vulnerability in cocaine-dependent individuals: preliminary data. Biol Psychiatry 51: 683–686.
Brewer WJ, Francey SM, Wood SJ, Jackson HJ, Pantelis C, Phillips LJ et al (2005). Memory impairments identified in people at ultra-high risk for psychosis who later develop first-episode psychosis. Am J Psychiatry 162: 71–78.
Brown E, Herman AB, Nagarajan S, Vinogradov S (under review) Increases in cortical gamma oscillatory activity correlate with improved behavior after computerized cognitive training in schizophrenia.
Buonomano DV, Merzenich MM (1998). Cortical plasticity: from synapses to maps. Annu Rev Neurosci 21: 149–186.
Burdick KE, Goldberg JF, Harrow M (2010). Neurocognitive dysfunction and psychosocial outcome in patients with bipolar I disorder at 15-year follow-up. Acta Psychiatr Scand 122: 499–506.
Bush G (2010). Attention-deficit/hyperactivity disorder and attention networks. Neuropsychopharmacology 35: 278–300.
Butler PD, Abeles IY, Weiskopf NG, Tambini A, Jalbrzikowski M, Legatt ME et al (2009). Sensory contributions to impaired emotion processing in schizophrenia. Schizophr Bull 35: 1095–1107.
Butler PD, Martinez A, Foxe JJ, Kim D, Zemon V, Silipo G et al (2007). Subcortical visual dysfunction in schizophrenia drives secondary cortical impairments. Brain 130: 417–430. This study was one of the first to conclusively demonstrate the presence of pervasive magnocellular dysfunction at the subcortical level that leads to secondary impairment in activation of cortical visual structures within dorsal and ventral stream visual pathways. These findings argue strongly for bottom-up dysfunction within the early visual pathway that may represent an organizing principle for understanding neurocognitive dysfunction in schizophrenia.
Buzsaki G (2006). Rhythms of the Brain. Oxford University Press: New York. This book is an erudite tour-de-force on the nature and function of neural oscillatory processes in the brain. Should be required reading for anyone interested in the science of mental operations.
Cao Q, Zang Y, Zhu C, Cao X, Sun L, Zhou X et al (2008). Alerting deficits in children with attention deficit/hyperactivity disorder: event-related fMRI evidence. Brain Res 1219: 159–168.
Carter CS, Barch DM, Bullmore E, Breiling J, Buchanan RW, Butler P et al (2011). Cognitive neuroscience treatment research to improve cognition in schizophrenia II: developing imaging biomarkers to enhance treatment development for schizophrenia and related disorders. Biol Psychiatry 70: 7–12.
Caspary DM, Ling L, Turner JG, Hughes LF (2008). Inhibitory neurotransmission, plasticity and aging in the mammalian central auditory system. J Exp Biol 211: 1781–1791.
Celnik P, Paik NJ, Vandermeeren Y, Dimyan M, Cohen LG (2009). Effects of combined peripheral nerve stimulation and brain polarization on performance of a motor sequence task after chronic stroke. Stroke 40: 1764–1771.
Chamberlain SR, Robbins TW, Winder-Rhodes S, Muller U, Sahakian BJ, Blackwell AD et al (2011). Translational approaches to frontostriatal dysfunction in attention-deficit/hyperactivity disorder using a computerized neuropsychological battery. Biol Psychiatry 69: 1192–1203.
Chang EF, Merzenich MM (2003). Environmental noise retards auditory cortical development. Science 300: 498–502.
Chang Y, Xu J, Shi N, Pang X, Zhang B, Cai Z (2011). Dysfunction of preattentive visual information processing among patients with major depressive disorder. Biol Psychiatry 69: 742–747.
Cherbuin N, Sachdev P, Anstey KJ (2010). Neuropsychological predictors of transition from healthy cognitive aging to mild cognitive impairment: the PATH through life study. Am J Geriatr Psychiatry 18: 723–733.
Classen J, Liepert J, Wise SP, Hallett M, Cohen LG (1998). Rapid plasticity of human cortical movement representation induced by practice. J Neurophysiol 79: 1117–1123.
Cohen DA, Freitas C, Tormos JM, Oberman L, Eldaief M, Pascual-Leone A (2010). Enhancing plasticity through repeated rTMS sessions: the benefits of a night of sleep. Clin Neurophysiol 121: 2159–2164.
Cooper RJ, Todd J, McGill K, Michie PT (2006). Auditory sensory memory and the aging brain: a mismatch negativity study. Neurobiol Aging 27: 752–762.
Cramer SC, Sur M, Dobkin BH, O’Brien C, Sanger TD, Trojanowski JQ et al (2011). Harnessing neuroplasticity for clinical applications. Brain 134 (Pt 6): 1591–1609.
Cruikshank SJ, Weinberger NM (1996). Evidence for the Hebbian hypothesis in experience-dependent physiological plasticity of neocortex: a critical review. Brain Res Brain Res Rev 22: 191–228.
Dale CL, Findlay AM, Adcock RA, Vertinski M, Fisher M, Genevsky A et al (2010). Timing is everything: neural response dynamics during syllable processing and its relation to higher-order cognition in schizophrenia and healthy comparison subjects. Int J Psychophysiol 75: 183–193.
Dalton KM, Nacewicz BM, Johnstone T, Schaefer HS, Gernsbacher MA, Goldsmith HH et al (2005). Gaze fixation and the neural circuitry of face processing in autism. Nat Neurosci 8: 519–526.
Degabriele R, Lagopoulos J, Malhi G (2011). Neural correlates of emotional face processing in bipolar disorder: an event-related potential study. J Affect Disord 133: 212–220.
Degutis JM, Van Vleet TM (2010). Tonic and phasic alertness training: a novel behavioral therapy to improve spatial and non-spatial attention in patients with hemispatial neglect. Front Hum Neurosci 4: pii: 60.
Deiber MP, Missonnier P, Bertrand O, Gold G, Fazio-Costa L, Ibanez V et al (2007). Distinction between perceptual and attentional processing in working memory tasks: a study of phase-locked and induced oscillatory brain dynamics. J Cogn Neurosci 19: 158–172.
Dennis NA, Cabeza R (2010). Age-related dedifferentiation of learning systems: an fMRI study of implicit and explicit learning. Neurobiol Aging 32: e17–e30.
de Villers-Sidani E, Alzghoul L, Zhou X, Simpson KL, Lin RC, Merzenich MM (2010). Recovery of functional and structural age-related changes in the rat primary auditory cortex with operant training. Proc Natl Acad Sci USA 107: 13900–13905. First demonstration of the recovery of inhibitory interneurons in the aged brain after behavioral training.
de Villers-Sidani E, Chang EF, Bao S, Merzenich MM (2007). Critical period window for spectral tuning defined in the primary auditory cortex (A1) in the rat. J Neurosci 27: 180–189.
de Villers-Sidani E, Simpson KL, Lu YF, Lin RC, Merzenich MM (2008). Manipulating critical period closure across different sectors of the primary auditory cortex. Nat Neurosci 11: 957–965.
Dias EC, Butler PD, Hoptman MJ, Javitt DC (2011). Early sensory contributions to contextual encoding deficits in schizophrenia. Arch Gen Psychiatry 68: 654–664.
Dickerson F, Boronow JJ, Stallings C, Origoni AE, Cole SK, Yolken RH (2004). Cognitive functioning in schizophrenia and bipolar disorder: comparison of performance on the Repeatable Battery for the Assessment of Neuropsychological Status. Psychiatry Res 129: 45–53.
Dickinson D, Tenhula W, Morris S, Brown C, Peer J, Spencer K et al (2010). A randomized, controlled trial of computer-assisted cognitive remediation for schizophrenia. Am J Psychiatry 167: 170–180.
Dinse HR (2006). Cortical reorganization in the aging brain. Prog Brain Res 157: 57–80.
Dockstader C, Gaetz W, Cheyne D, Tannock R (2009). Abnormal neural reactivity to unpredictable sensory events in attention-deficit/hyperactivity disorder. Biol Psychiatry 66: 376–383.
Dong X, Simon MA, Wilson RS, Mendes de Leon CF, Rajan KB, Evans DA (2010). Decline in cognitive function and risk of elder self-neglect: finding from the Chicago Health Aging Project. J Am Geriatr Soc 58: 2292–2299.
Edeline JM, Manunta Y, Hennevin E (2010). Induction of selective plasticity in the frequency tuning of auditory cortex and auditory thalamus neurons by locus coeruleus stimulation. Hear Res 274: 75–84.
Edwards JD, Delahunt PB, Mahncke HW (2009). Cognitive speed of processing training delays driving cessation. J Gerontol A Biol Sci Med Sci 64: 1262–1267.
Eisenberg DP, Berman KF (2010). Executive function, neural circuitry, and genetic mechanisms in schizophrenia. Neuropsychopharmacology 35: 258–277.
Falconer EM, Felmingham KL, Allen A, Clark CR, McFarlane AC, Williams LM et al (2008). Developing an integrated brain, behavior and biological response profile in posttraumatic stress disorder (PTSD). J Integr Neurosci 7: 439–456.
Fell J, Axmacher N (2011). The role of phase synchronization in memory processes. Nat Rev Neurosci 12: 105–118. This review examines evidence on how processes underlying working and long-term memory interact in the medial temporal lobe. The authors propose that this is accomplished by neural operations involving phase-phase and phase-amplitude synchronization in oscillatory patterns, and that this mechanism supports the flexibility of and interaction between memory systems. This suggests that phase synchronization of operations n key neural systems may be an important treatment target for impaired brains.
Fisher M, Holland C, Merzenich MM, Vinogradov S (2009). Using neuroplasticity-based auditory training to improve verbal memory in schizophrenia. Am J Psychiatry 166: 805–811. The first report of using an explicitly neuroplasticity-based cognitive training approach in a psychiatric illness.
Fisher M, Holland C, Subramaniam K, Vinogradov S (2010). Neuroplasticity-based cognitive training in schizophrenia: an interim report on the effects 6 months later. Schizophr Bull 36: 869–879.
Fiszdon JM, Cardenas AS, Bryson GJ, Bell MD (2005). Predictors of remediation success on a trained memory task. J Nerv Ment Dis 193: 602–608.
Franz CE, Lyons MJ, O’Brien R, Panizzon MS, Kim K, Bhat R et al (2011). A 35-year longitudinal assessment of cognition and midlife depression symptoms: the Vietnam Era Twin Study of Aging. Am J Geriatr Psychiatry 19: 559–570.
Friedman-Hill SR, Wagman MR, Gex SE, Pine DS, Leibenluft E, Ungerleider LG (2010). What does distractibility in ADHD reveal about mechanisms for top-down attentional control? Cognition 115: 93–103.
Froemke RC, Merzenich MM, Schreiner CE (2007). A synaptic memory trace for cortical receptive field plasticity. Nature 450: 425–429.
Gazzaley A (2010). Influence of early attentional modulation on working memory. Neuropsychologia 49: 1410–1424.
Gazzaley A, Clapp W, Kelley J, McEvoy K, Knight RT, D’Esposito M (2008). Age-related top-down suppression deficit in the early stages of cortical visual memory processing. Proc Natl Acad Sci USA 105: 13122–13126.
Gonzalez-Burgos G, Hashimoto T, Lewis DA (2010). Alterations of cortical GABA neurons and network oscillations in schizophrenia. Curr Psychiatry Rep 12: 335–344.
Gordon E, Palmer DM, Cooper N (2010). EEG alpha asymmetry in schizophrenia, depression, PTSD, panic disorder, ADHD and conduct disorder. Clin EEG Neurosci 41: 178–183.
Grande I, Fries GR, Kunz M, Kapczinski F (2010). The role of BDNF as a mediator of neuroplasticity in bipolar disorder. Psychiatry Investig 7: 243–250.
Grossman AW, Churchill JD, McKinney BC, Kodish IM, Otte SL, Greenough WT (2003). Experience effects on brain development: possible contributions to psychopathology. J Child Psychol Psychiatry 44: 33–63.
Han YK, Kover H, Insanally MN, Semerdjian JH, Bao S (2007). Early experience impairs perceptual discrimination. Nat Neurosci 10: 1191–1197.
Hartley CA, Phelps EA (2010). Changing fear: the neurocircuitry of emotion regulation. Neuropsychopharmacology 35: 136–146.
Haut KM, Lim KO, MacDonald 3rd A (2010). Prefrontal cortical changes following cognitive training in patients with chronic schizophrenia: effects of practice, generalization, and specificity. Neuropsychopharmacology 35: 1850–1859. The first report of changes in prefrontal cortical activation patterns after cognitive training in schizophrenia, demonstrating that the impaired brain still retains the capacity for significant functional plasticity.
Hayes EA, Warrier CM, Nicol TG, Zecker SG, Kraus N (2003). Neural plasticity following auditory training in children with learning problems. Clin Neurophysiol 114: 673–684.
Heckers S, Rauch SL, Goff D, Savage CR, Schacter DL, Fischman AJ et al (1998). Impaired recruitment of the hippocampus during conscious recollection in schizophrenia. Nat Neurosci 1: 318–323.
Heinz A, Schlagenhauf F (2010). Dopaminergic dysfunction in schizophrenia: salience attribution revisited. Schizophr Bull 36: 472–485.
Henson RN, Gagnepain P (2010). Predictive, interactive multiple memory systems. Hippocampus 20: 1315–1326. Thoughtful review on the nature of feedforward and feedback interactions among perceptual, semantic, and episodic memory systems in humans. Very helpful overview for considerations on how impairment in any of these systems will have distributed repercussions.
Hermanutz M, Gestrich J (1991). Computer-assisted attention training in schizophrenics. A comparative study. Eur Arch Psychiatry Clin Neurosci 240: 282–287.
Hermens DF, Naismith SL, Redoblado Hodge MA, Scott EM, Hickie IB (2010). Impaired verbal memory in young adults with unipolar and bipolar depression. Early Interv Psychiatry 4: 227–233.
Hickok G, Houde J, Rong F (2011). Sensorimotor integration in speech processing: computational basis and neural organization. Neuron 69: 407–422.
Hileman CM, Henderson H, Mundy P, Newell L, Jaime M (2011). Developmental and individual differences on the P1 and N170 ERP components in children with and without autism. Dev Neuropsychol 36: 214–236.
Hinckley L, Findlay AM, Dale C, Subramaniam K, Luks TL, Vinogradov S (under review) Changes in alpha band resting state functional connectivity after cognitive training in patients with schizophrenia.
Hitoglou M, Ververi A, Antoniadis A, Zafeiriou DI (2010). Childhood autism and auditory system abnormalities. Pediatr Neurol 42: 309–314.
Hoekzema E, Carmona S, Tremols V, Gispert JD, Guitart M, Fauquet J et al (2010). Enhanced neural activity in frontal and cerebellar circuits after cognitive training in children with attention-deficit/hyperactivity disorder. Hum Brain Mapp 31: 1942–1950.
Hofer A, Bodner T, Kaufmann A, Kemmler G, Mattarei U, Pfaffenberger NM et al (2011). Symptomatic remission and neurocognitive functioning in patients with schizophrenia. Psychol Med 41: 2131–2139.
Hopkins IM, Gower MW, Perez TA, Smith DS, Amthor FR, Casey Wimsatt F et al (2011). Avatar assistant: improving social skills in students with an ASD through a computer-based intervention. J Autism Dev Disord (e-pub ahead of print November 2011).
Huitt W, Cain S (2005). An Overview of the Conative Domain. Valdosta State University: Valdosta, GA: Retrieved 6 April 2007 from http://teach.valdosta.edu/whuitt/brilstar/chapters/conative.doc.
Irvine DR, Rajan R (1997). Injury-induced reorganization of frequency maps in adult auditory cortex: the role of unmasking of normally-inhibited inputs. Acta Otolaryngol Suppl 532: 39–45.
Javitt DC (2009). When doors of perception close: bottom-up models of disrupted cognition in schizophrenia. Annu Rev Clin Psychol 5: 249–275.
Javitt DC, Rabinowicz E, Silipo G, Dias EC (2007). Encoding vs. retention: differential effects of cue manipulation on working memory performance in schizophrenia. Schizophr Res 91: 159–168.
Jenkins WM, Merzenich MM, Ochs MT, Allard T, Guic-Robles E (1990). Functional reorganization of primary somatosensory cortex in adult owl monkeys after behaviorally controlled tactile stimulation. J Neurophysiol 63: 82–104.
Jo JM, Kim YH, Ko MH, Ohn SH, Joen B, Lee KH (2009). Enhancing the working memory of stroke patients using tDCS. Am J Phys Med Rehabil 88: 404–409.
Kalkstein S, Hurford I, Gur RC (2010). Neurocognition in schizophrenia. Curr Top Behav Neurosci 4: 373–390.
Kang EK, Baek MJ, Kim S, Paik NJ (2009). Non-invasive cortical stimulation improves post-stroke attention decline. Restor Neurol Neurosci 27: 645–650.
Kanne SM, Gerber AJ, Quirmbach LM, Sparrow SS, Cicchetti DV, Saulnier CA (2010). The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. J Autism Dev Disord 41: 1007–1018.
Karni A, Meyer G, Jezzard P, Adams MM, Turner R, Ungerleider LG (1995). Functional MRI evidence for adult motor cortex plasticity during motor skill learning. Nature 377: 155–158.
Karni A, Meyer G, Rey-Hipolito C, Jezzard P, Adams MM, Turner R et al (1998). The acquisition of skilled motor performance: fast and slow experience-driven changes in primary motor cortex. Proc Natl Acad Sci USA 95: 861–868. One of the first studies to demonstrate the neural correlates of early and later phases of skill learning in human cortex.
Keefe RS, Kraus MS, Krishnan RR (2011). Failures in learning-dependent predictive perception as the key cognitive vulnerability to psychosis in schizophrenia. Neuropsychopharmacology 36: 367–368. A well-written review on the nature of prefrontally-mediated predictive operations in perceptual processing and how a disruption in these operations may lead to psychotic symptoms.
Keefe RS, Perkins DO, Gu H, Zipursky RB, Christensen BK, Lieberman JA (2006). A longitudinal study of neurocognitive function in individuals at-risk for psychosis. Schizophr Res 88: 26–35.
Keefe RE, Vinogradov S, Medalia A, Buckley PF, Caroff SN, D’Souza DC et al (in press). Feasibility and pilot efficacy results from the multi-site cognitive remediation in the Schizophrenia trials network (CRSTN) study. J Clin Psychiatry (in press).
Keefe RS, Vinogradov S, Medalia A, Silverstein SM, Bell MD, Dickinson D et al (2010). Report from the working group conference on multisite trial design for cognitive remediation in schizophrenia. Schizophr Bull 37: 1057–1065.
Khader PH, Jost K, Ranganath C, Rosler F (2010). Theta and alpha oscillations during working-memory maintenance predict successful long-term memory encoding. Neurosci Lett 468: 339–343.
Khedr EM, Etraby AE, Hemeda M, Nasef AM, Razek AA (2010). Long-term effect of repetitive transcranial magnetic stimulation on motor function recovery after acute ischemic stroke. Acta Neurol Scand 121: 30–37.
Kilgard MP (2002). How sensory experience shapes cortical representations. In: Squire L, Schacter D (eds). Neuropsychology of Memory. Guilford Press: NY, USA.
Kilgard MP, Merzenich MM (1998). Cortical map reorganization enabled by nucleus basalis activity. Science 279: 1714–1718. Shows that pairing between a simple sensory stimulus and cholinergic release results in a rapid and long lasting retuning of cortical maps to favor the detection of the paired stimulus.
Kirchner JC, Hatri A, Heekeren HR, Dziobek I (2011). Autistic symptomatology, face processing abilities, and eye fixation patterns. J Autism Dev Disord 41: 158–167.
Kleim JA, Hogg TM, VandenBerg PM, Cooper NR, Bruneau R, Remple M (2004). Cortical synaptogenesis and motor map reorganization occur during late, but not early, phase of motor skill learning. J Neurosci 24: 628–633.
Kleim JA, Lussnig E, Schwarz ER, Comery TA, Greenough WT (1996). Synaptogenesis and Fos expression in the motor cortex of the adult rat after motor skill learning. J Neurosci 16: 4529–4535.
Kleim JA, Pipitone MA, Czerlanis C, Greenough WT (1998). Structural stability within the lateral cerebellar nucleus of the rat following complex motor learning. Neurobiol Learn Mem 69: 290–306.
Klimkowicz-Mrowiec A, Slowik A, Krzywoszanski L, Herzog-Krzywoszanska R, Szczudlik A (2008). Severity of explicit memory impairment due to Alzheimer’s disease improves effectiveness of implicit learning. J Neurol 255: 502–509.
Klingberg T (2010). Training and plasticity of working memory. Trends Cogn Sci 14: 317–324.
Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlstrom K et al (2005). Computerized training of working memory in children with ADHD—a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry 44: 177–186. The first report of a neuroscience-informed approach to training of working memory dysfunction in children with ADD.
Klintsova AY, Dickson E, Yoshida R, Greenough WT (2004). Altered expression of BDNF and its high-affinity receptor TrkB in response to complex motor learning and moderate exercise. Brain Res 1028: 92–104.
Koch K, Schachtzabel C, Wagner G, Schikora J, Schultz C, Reichenbach JR et al (2010). Altered activation in association with reward-related trial-and-error learning in patients with schizophrenia. Neuroimage 50: 223–232.
Kofler MJ, Rapport MD, Bolden J, Sarver DE, Raiker JS, Alderson RM (2011). Working memory deficits and social problems in children with ADHD. J Abnorm Child Psychol 39: 805–817.
Koob GF, Volkow ND (2010). Neurocircuitry of addiction. Neuropsychopharmacology 35: 217–238.
Koskinen SM, Ahveninen J, Kujala T, Kaprio J, BF OD, Osipova D et al (2011). A longitudinal twin study of effects of adolescent alcohol abuse on the neurophysiology of attention and orienting. Alcohol Clin Exp Res 35: 1339–1350.
Kurtz MM, Moberg PJ, Gur RC, Gur RE (2001). Approaches to cognitive remediation of neuropsychological deficits in schizophrenia: a review and meta-analysis. Neuropsychol Rev 11: 197–210.
Kurtz MM, Seltzer JC, Shagan DS, Thime WR, Wexler BE (2007). Computer-assisted cognitive remediation in schizophrenia: what is the active ingredient? Schizophr Res 89: 251–260.
Laubach M, Wessberg J, Nicolelis MA (2000). Cortical ensemble activity increasingly predicts behaviour outcomes during learning of a motor task. Nature 405: 567–571.
Lee J, Park S (2006). The role of stimulus salience in CPT-AX performance of schizophrenia patients. Schizophr Res 81: 191–197.
Leekam SR, Nieto C, Libby SJ, Wing L, Gould J (2007). Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord 37: 894–910.
Leonardo ED, Hen R (2008). Anxiety as a developmental disorder. Neuropharmacol Rev 33: 134–140.
Leskin LP, White PM (2007). Attentional networks reveal executive function deficits in posttraumatic stress disorder. Neuropsychology 21: 275–284.
Liang H, Bressler SL, Ding M, Truccolo WA, Nakamura R (2002). Synchronized activity in prefrontal cortex during anticipation of visuomotor processing. Neuroreport 13: 2011–2015.
Light GA, Swerdlow NR, Braff DL (2007). Preattentive sensory processing as indexed by the MMN and P3a brain responses is associated with cognitive and psychosocial functioning in healthy adults. J Cogn Neurosci 19: 1624–1632. An important demonstration of the association between impaired pre-attentive perceptual processing and higher order cognitive and psychosocial impairments in healthy individuals. Provides clear evidence of the co-occurence of functionally meaningful higher-level cognitive limitations and lower-level perceptual processing deficits.
Lijffijt M, Moeller FG, Boutros NN, Steinberg JL, Meier SL, Lane SD et al (2009). Diminished P50, N100 and P200 auditory sensory gating in bipolar I disorder. Psychiatry Res 167: 191–201.
Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L (2011). Hearing loss and incident dementia. Arch Neurol 68: 214–220.
Mahncke HW, Bronstone A, Merzenich MM (2006a). Brain plasticity and functional losses in the aged: scientific bases for a novel intervention. Prog Brain Res 157: 81–109.
Mahncke HW, Connor BB, Appelman J, Ahsanuddin ON, Hardy JL, Wood RA et al (2006b). Memory enhancement in healthy older adults using a brain plasticity-based training program: a randomized, controlled study. Proc Natl Acad Sci USA 103: 12523–12528. The first report of an RCT of a neuroplasticity-based cognitive training method for memory loss in healthy aging.
Mangels JA, Butterfield B, Lamb J, Good C, Dweck CS (2006). Why do beliefs about intelligence influence learning success? A social cognitive neuroscience model. Soc Cogn Affect Neurosci 1: 75–86. A critically important overview of a body of work that demonstrates that internalized beliefs about intelligence influence an individual’s response to learning events. Required reading for anyone interested in developing behavioral interventions for the impaired brain.
Marco J, Fuentemilla L, Grau C (2005). Auditory sensory gating deficit in abstinent chronic alcoholics. Neurosci Lett 375: 174–177.
Martinez-Aran A, Vieta E, Reinares M, Colom F, Torrent C, Sanchez-Moreno J et al (2004). Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. Am J Psychiatry 161: 262–270.
Marx BP, Doron-Lamarca S, Proctor SP, Vasterling JJ (2009). The influence of pre-deployment neurocognitive functioning on post-deployment PTSD symptom outcomes among Iraq-deployed Army soldiers. J Int Neuropsychol Soc 15: 840–852.
Maviel T, Durkin TP, Menzaghi F, Bontempi B (2004). Sites of neocortical reorganization critical for remote spatial memory. Science 305: 96–99.
McGurk SR, Mueser KT, Pascaris A (2005). Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial. Schizophr Bull 31: 898–909.
McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT (2007). A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry 164: 1791–1802.
Meltzoff AN, Kuhl PK, Movellan J, Sejnowski TJ (2009). Foundations for a new science of learning. Science 325: 284–288. An extremely important overview of what is now known about how humans learn. Emphasizes the critical role of social interactions during the implicit acquisition of skills. A good springboard into deeper reading about some of the elements that promote successful learning of new skills.
Menning H, Renz A, Seifert J, Maercker A (2008). Reduced mismatch negativity in posttraumatic stress disorder: a compensatory mechanism for chronic hyperarousal? Int J Psychophysiol 68: 27–34.
Mercado 3rd E, Myers CE, Gluck MA (2001). A computational model of mechanisms controlling experience-dependent reorganization of representational maps in auditory cortex. Cogn Affect Behav Neurosci 1: 37–55.
Merzenich MM, DeCharms RC (1996). Neural Representations, Experience and Change. MIT Press: Boston.
Merzenich MM, Recanzone GH, Jenkins WM (1991). How the Brain Functionally Rewires Itself. MIT Press: New York.
Miller BT, Deouell LY, Dam C, Knight RT, D’Esposito M (2008). Spatio-temporal dynamics of neural mechanisms underlying component operations in working memory. Brain Res 1206: 61–75.
Minshew NJ, Goldstein G, Siegel DJ (1997). Neuropsychologic functioning in autism: profile of a complex information processing disorder. J Int Neuropsychol Soc 3: 303–316.
Molinuevo JL, Gomez-Anson B, Monte GC, Bosch B, Sanchez-Valle R, Rami L (2011). Neuropsychological profile of prodromal Alzheimer’s disease (Prd-AD) and their radiological correlates. Arch Gerontol Geriatr 52: 190–196.
Monti A, Cogiamanian F, Marceglia S, Ferrucci R, Mameli F, Mrakic-Sposta S et al (2008). Improved naming after transcranial direct current stimulation in aphasia. J Neurol Neurosurg Psychiatry 79: 451–453.
Moriyama Y, Mimura M, Kato M, Yoshino A, Hara T, Kashima H et al (2002). Executive dysfunction and clinical outcome in chronic alcoholics. Alcohol Clin Exp Res 26: 1239–1244.
Morris SE, Heerey EA, Gold JM, Holroyd CB (2008). Learning-related changes in brain activity following errors and performance feedback in schizophrenia. Schizophr Res 99: 274–285.
Mukai I, Kim D, Fukunaga M, Japee S, Marrett S, Ungerleider LG (2007). Activations in visual and attention-related areas predict and correlate with the degree of perceptual learning. J Neurosci 27: 11401–11411.
Nahum M, Daikhin L, Lubin Y, Cohen Y, Ahissar M (2010). From comparison to classification: a cortical tool for boosting perception. J Neurosci 30: 1128–1136.
Naismith SL, Lagopoulos J, Ward PB, Davey CG, Little C, Hickie IB (2010). Fronto-striatal correlates of impaired implicit sequence learning in major depression: an fMRI study. J Affect Disord 125: 256–261.
Nemeth D, Janacsek K, Balogh V, Londe Z, Mingesz R, Fazekas M et al (2010). Learning in autism: implicitly superb. PLoS One 5: e11731.
Nomoto K, Schultz W, Watanabe T, Sakagami M (2010). Temporally extended dopamine responses to perceptually demanding reward-predictive stimuli. J Neurosci 30: 10692–10702. A recent study showing that dopamine neurons reflect the reward value of perceptually complicated and temporally extended stimuli; the results suggest that dopamine neurons use the moment-to-moment reward prediction associated with environmental stimuli to compute a reward prediction error.
Nudo RJ, Milliken GW, Jenkins WM, Merzenich MM (1996). Use-dependent alterations of movement representations in primary motor cortex of adult squirrel monkeys. J Neurosci 16: 785–807.
Oblak A, Gibbs TT, Blatt GJ (2009). Decreased GABAA receptors and benzodiazepine binding sites in the anterior cingulate cortex in autism. Autism Res 2: 205–219.
Oie M, Sundet K, Ueland T (2011). Neurocognition and functional outcome in early-onset schizophrenia and attention-deficit/hyperactivity disorder: a 13-year follow-up. Neuropsychology 25: 25–35.
Owen AM, Hampshire A, Grahn JA, Stenton R, Dajani S, Burns AS et al (2010). Putting brain training to the test. Nature 465: 775–778.
Pajonk FG, Wobrock T, Gruber O, Scherk H, Berner D, Kaizl I et al (2010). Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry 67: 133–143.
Panizzutti R, de Villers-Sidani E, Zhou J, Merzenich M (under review) Ventral orbital cortical activation during sequence learning in the rat.
Panizzutti R, Vinogradov S, Hamilton S (under review) Poymorphisms of COMT and DISC 1 genes associated with response to cognitive training in schizophrenia.
Passetti F, Clark L, Mehta MA, Joyce E, King M (2008). Neuropsychological predictors of clinical outcome in opiate addiction. Drug Alcohol Depend 94: 82–91.
Patten SB (2008). Sensitization: the sine qua non of the depressive disorders? Med Hypotheses 71: 872–875.
Penades R, Catalan R, Salamero M, Boget T, Puig O, Guarch J et al (2006). Cognitive remediation therapy for outpatients with chronic schizophrenia: a controlled and randomized study. Schizophr Res 87: 323–331.
Poldrack RA, Packard MG (2003). Competition among multiple memory systems: converging evidence from animal and human brain studies. Neuropsychologia 41: 245–251.
Polley DB, Steinberg EE, Merzenich MM (2006). Perceptual learning directs auditory cortical map reorganization through top-down influences. J Neurosci 26: 4970–4982.
Price JL, Drevets WC (2010). Neurocircuitry of mood disorders. Neuropsychopharmacology 35: 192–216.
Rabiner DL, Murray DW, Skinner AT, Malone PS (2010). A randomized trial of two promising computer-based interventions for students with attention difficulties. J Abnorm Child Psychol 38: 131–142.
Ragland JD, Censits DM, Gur RC, Glahn DC, Gallacher F, Gur RE (1996). Assessing declarative memory in schizophrenia using Wisconsin Card Sorting Test stimuli: the Paired Associate Recognition Test. Psychiatry Res 60: 135–145.
Reynolds B (2006). A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol 17: 651–667.
Rioult-Pedotti MS, Friedman D, Hess G, Donoghue JP (1998). Strengthening of horizontal cortical connections following skill learning. Nat Neurosci 1: 230–234.
Roberts DL, Penn DL (2009). Social cognition and interaction training (SCIT) for outpatients with schizophrenia: a preliminary study. Psychiatry Res 166: 141–147.
Robinson TE, Berridge KC (2008). Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci 363: 3137–3146.
Roelfsema PR, van Ooyen A, Watanabe T (2010). Perceptual learning rules based on reinforcers and attention. Trends Cogn Sci 14: 64–71. This state-of-the-art review summarizes the roles of two factors that guide plasticity in visual learningsystems; reinforcers, that cause the release of diffusive neuromodulatory signals that gate plasticity, and attentional feedback signals, that highlight the network of neurons responsible for the learned action.
Rohling ML, Faust ME, Beverly B, Demakis G (2009). Effectiveness of cognitive rehabilitation following acquired brain injury: a meta-analytic re-examination of Cicerone et al’s (2000, 2005) systematic reviews. Neuropsychology 23: 20–39.
Rutkowski RG, Weinberger NM (2005). Encoding of learned importance of sound by magnitude of representational area in primary auditory cortex. Proc Natl Acad Sci USA 102: 13664–13669. Shows that behavioral relevance (reward/punishment) is a potent inducer of plasticity in cortical sensory maps.
Rutman AM, Clapp WC, Chadick JZ, Gazzaley A (2010). Early top-down control of visual processing predicts working memory performance. J Cogn Neurosci 22: 1224–1234.
Sartory G, Zorn C, Groetzinger G, Windgassen K (2005). Computerized cognitive remediation improves verbal learning and processing speed in schizophrenia. Schizophr Res 75: 219–223.
Satterfield JH, Schell AM, Nicholas T (1994). Preferential neural processing of attended stimuli in attention-deficit hyperactivity disorder and normal boys. Psychophysiology 31: 1–10.
Schultz W, Dickinson A (2000). Neuronal coding of prediction errors. Annu Rev Neurosci 23: 473–500. Landmark paper on the role of prediction errors in associative learning.
Seitz AR, Dinse HR (2007). A common framework for perceptual learning. Curr Opin Neurobiol 17: 148–153.
Shen IH, Tsai SY, Duann JR (2011). Inhibition control and error processing in children with attention deficit/hyperactivity disorder: an event-related potentials study. Int J Psychophysiol 81: 1–11.
Shestyuk AY, Deldin PJ (2010). Automatic and strategic representation of the self in major depression: trait and state abnormalities. Am J Psychiatry 167: 536–544.
Simons CJ, Jacobs N, Derom C, Thiery E, Jolles J, van Os J et al (2009). Cognition as predictor of current and follow-up depressive symptoms in the general population. Acta Psychiatr Scand 120: 45–52.
Smith GE, Housen P, Yaffe K, Ruff R, Kennison RF, Mahncke HW et al (2009). A cognitive training program based on principles of brain plasticity: results from the Improvement in Memory with Plasticity-based Adaptive Cognitive Training (IMPACT) study. J Am Geriatr Soc 57: 594–603.
Spaulding WD, Reed D, Sullivan M, Richardson C, Weiler M (1999). Effects of cognitive treatment in psychiatric rehabilitation. Schizophr Bull 25: 657–676.
Spaulding WD, Storms L, Goodrich V, Sullivan M (1986). Applications of experimental psychopathology in psychiatric rehabilitation. Schizophr Bull 12: 560–577.
Subramaniam K, Luks T, Fisher M, Simpson G, Nagarajan S, Vinogradov S (in press) Restoring reality monitoring in schizophrenia. Neuron. First paper to show that intensive neuroscience-guided training of component cognitive processes restores both behavioral performance and neural correlates of a complex meta-cognitive operation in subjects with schizophrenia. Also demonstrates that training-induced improvement in prefrontal cortical activation patterns is associated with improved social functioning 6 months after training.
Swettenham J, Baron-Cohen S, Charman T, Cox A, Baird G, Drew A et al (1998). The frequency and distribution of spontaneous attention shifts between social and nonsocial stimuli in autistic, typically developing, and nonautistic developmentally delayed infants. J Child Psychol Psychiatry 39: 747–753.
Takashima A, Jensen O, Oostenveld R, Maris E, van de Coevering M, Fernandez G (2006). Successful declarative memory formation is associated with ongoing activity during encoding in a distributed neocortical network related to working memory: a magnetoencephalography study. Neuroscience 139: 291–297.
Tallal P, Miller SL, Bedi G, Byma G, Wang X, Nagarajan SS et al (1996). Language comprehension in language-learning impaired children improved with acoustically modified speech. Science 271: 81–84. The first report of a trial of neuroplasticity-based cognitive training in a human learning disorder.
Temple E, Deutsch GK, Poldrack RA, Miller SL, Tallal P, Merzenich MM et al (2003). Neural deficits in children with dyslexia ameliorated by behavioral remediation: evidence from functional MRI. Proc Natl Acad Sci USA 100: 2860–2865.
Teufel C, Kingdon A, Ingram JN, Wolpert DM, Fletcher PC (2010). Deficits in sensory prediction are related to delusional ideation in healthy individuals. Neuropsychologia 48: 4169–4172.
Thoma RJ, Monnig MA, Lysne PA, Ruhl DA, Pommy JA, Bogenschutz M et al (2011). Adolescent substance abuse: the effects of alcohol and marijuana on neuropsychological performance. Alcohol Clin Exp Res 35: 39–46.
Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry 67: 614–623.
Tokarski K, Urban-Ciecko J, Kossut M, Hess G (2007). Sensory learning-induced enhancement of inhibitory synaptic transmission in the barrel cortex of the mouse. Eur J Neurosci 26: 134–141.
Torralva T, Gleichgerrcht E, Torrente F, Roca M, Strejilevich SA, Cetkovich M et al (2010). Neuropsychological functioning in adult bipolar disorder and ADHD patients: a comparative study. Psychiatry Res 186: 261–266.
Turner LM, Stone WL, Pozdol SL, Coonrod EE (2006). Follow-up of children with autism spectrum disorders from age 2 to age 9. Autism 10: 243–265.
Ungerleider LG, Doyon J, Karni A (2002). Imaging brain plasticity during motor skill learning. Neurobiol Learn Mem 78: 553–564.
Veltmeyer MD, Clark CR, McFarlane AC, Felmingham KL, Bryant RA, Gordon E (2005). Integrative assessment of brain and cognitive function in post-traumatic stress disorder. J Integr Neurosci 4: 145–159.
Vernon D, Egner T, Cooper N, Compton T, Neilands C, Sheri A et al (2003). The effect of training distinct neurofeedback protocols on aspects of cognitive performance. Int J Psychophysiol 47: 75–85.
Victor TA, Furey ML, Fromm SJ, Ohman A, Drevets WC (2010). Relationship between amygdala responses to masked faces and mood state and treatment in major depressive disorder. Arch Gen Psychiatry 67: 1128–1138.
Vinogradov S, Fisher M, Holland C, Shelly W, Wolkowitz O, Mellon SH (2009). Is serum brain-derived neurotrophic factor a biomarker for cognitive enhancement in schizophrenia? Biol Psychiatry 66: 549–553.
Vinogradov S, Fisher M, Loewy R, Lee A, Moua K, Pham L (unpublished data) Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia.
Voss JL, Gonsalves BD (2010). Time to go our separate ways: opposite effects of study duration on priming and recognition reveal distinct neural substrates. Front Hum Neurosci 4: 227.
Wagner BR (1968). The training of attending and abstracting responses in chronic schizophrenia. J Exp Res Pers 3: 77–88.
Wang X, Merzenich MM, Sameshima K, Jenkins WM (1995). Remodelling of hand representation in adult cortex determined by timing of tactile stimulation. Nature 378: 71–75. Shows that Hebbian principles apply to somatosensory cortical plasticity: in the context of a rewarded task, sensory inputs reaching the brain synchronously are represented together while those activating the cortex asynchronously are represented separately.
Weinberger NM (2003). The nucleus basalis and memory codes: auditory cortical plasticity and the induction of specific, associative behavioral memory. Neurobiol Learn Mem 80: 268–284.
Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R et al (2011). Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depress Anxiety 28: 686–695.
Witton C (2010). Childhood auditory processing disorder as a developmental disorder: the case for a multi-professional approach to diagnosis and management. Int J Audiol 49: 83–87.
Wolinsky FD, Mahncke H, Vander Weg MW, Martin R, Unverzagt FW, Ball KK et al (2010). Speed of processing training protects self-rated health in older adults: enduring effects observed in the multi-site ACTIVE randomized controlled trial. Int Psychogeriatr 22: 470–478.
Wolinsky FD, Mahncke HW, Kosinski M, Unverzagt FW, Smith DM, Jones RN et al (2009a). The ACTIVE cognitive training trial and predicted medical expenditures. BMC Health Serv Res 9: 109. A large multi-trial RCT of cognitive training in at-risk older adults and its subsequent effects on lowering medical expenditures in the years after training.
Wolinsky FD, Mahncke HW, Weg MW, Martin R, Unverzagt FW, Ball KK et al (2009b). The ACTIVE cognitive training interventions and the onset of and recovery from suspected clinical depression. J Gerontol B Psychol Sci Soc Sci 64: 577–585. A large multi-trial RCT of cognitive training in at-risk older adults and its subsequent effects on reducing rates of depression.
Wölwer W, Frommann N, Halfmann S, Piaszek A, Streit M, Gaebel W (2005). Remediation of impairments in facial affect recognition in schizophrenia: efficacy and specificity of a new training program. Schizophr Res 80: 295–303.
Wong TK, Fung PC, Chua SE, McAlonan GM (2008). Abnormal spatiotemporal processing of emotional facial expressions in childhood autism: dipole source analysis of event-related potentials. Eur J Neurosci 28: 407–416.
Wykes T, Huddy V, Cellard C, McGurk SR, Czobor P (2011). A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry 168: 472–485.
Wykes T, Reeder C, Corner J, Williams C, Everitt B (1999). The effects of neurocognitive remediation on executive processing in patients with schizophrenia. Schizophr Bull 25: 291–307.
Wykes T, Reeder C, Landau S, Everitt B, Knapp M, Patel A et al (2007). Cognitive remediation therapy in schizophrenia: randomised controlled trial. Br J Psychiatry 190: 421–427.
Wynn JK, Sugar C, Horan WP, Kern R, Green MF (2010). Mismatch negativity, social cognition, and functioning in schizophrenia patients. Biol Psychiatry 67: 940–947. A carefully constructed study that demonstrates the association between pre-attentive perceptual processing abnormalities and social functioning in schizophrenia.
Yang TT, Gallen CC, Ramachandran VS, Cobb S, Schwartz BJ, Bloom FE (1994). Noninvasive detection of cerebral plasticity in adult human somatosensory cortex. Neuroreport 5: 701–704.
Yang W, Zhu X, Wang X, Wu D, Yao S (2011). Time course of affective processing bias in major depression: an ERP study. Neurosci Lett 487: 372–377.
Yeap S, Kelly SP, Reilly RB, Thakore JH, Foxe JJ (2009). Visual sensory processing deficits in patients with bipolar disorder revealed through high-density electrical mapping. J Psychiatry Neurosci 34: 459–464.
Zanto TP, Gazzaley A (2009). Neural suppression of irrelevant information underlies optimal working memory performance. J Neurosci 29: 3059–3066. A key investigation into the deleterious role of irrelevant information (interference) on working memory performance in healthy subjects. Suggests the key neural mechanism in which a failure to suppress task-irrelevant sensory information very early in the pre-attentive processing stream can have an impact on higher-level cognitive operations.
Zanto TP, Rubens MT, Thangavel A, Gazzaley A (2011). Causal role of the prefrontal cortex in top-down modulation of visual processing and working memory. Nat Neurosci 14: 656–661.
Zedkova L, Woodward ND, Harding I, Tibbo PG, Purdon SE (2006). Procedural learning in schizophrenia investigated with functional magnetic resonance imaging. Schizophr Res 88: 198–207.
Zhang LI, Bao S, Merzenich MM (2001). Persistent and specific influences of early acoustic environments on primary auditory cortex. Nat Neurosci 4: 1123–1130.
Zhou X, de Villers-Sidani E, Panizzutti R, Merzenich MM (2010). Successive-signal biasing for a learned sound sequence. Proc Natl Acad Sci USA 107: 14839–14844. Shows how top-down influences dynamically retune sensory cortices to maximize the detection of behaviorally relevant stimuli.
Zhou X, Panizzutti R, de Villers-Sidani E, Madeira C, Merzenich MM (2011). Natural restoration of critical period plasticity in the juvenile and adult primary auditory cortex. J Neurosci 31: 5625–5634.
Acknowledgements
We thank Henry Mahncke, Michael Merzenich, Srikantan Nagarajan, and Rogerio Panizzutti for their input on many of the topics covered in this review. We also gratefully acknowledge Rachel So, Karuna Subramaniam, Danielle Schlosser, Virginia Powell and Toby Pillinger for help during preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Vinogradov is a paid consultant to Brain Plasticity Inc., a company with a commercial interest in cognitive training software.
Additional information
SUMMARY POINTS
• Neuropsychiatric illnesses are associated with dysfunction in distributed prefrontal neural systems that underlie perception, cognition, social interactions, emotion regulation, and motivation. The high degree of learning-dependent brain plasticity in these networks suggests that we should be able to engineer very specific training programs that drive meaningful and enduring improvements in their operations.
• Neuropsychiatric illnesses have features that set them apart from other neurological disorders, including possible inherent limitations in the underlying brain ‘learning machinery’ due to pathophysiology. They are also characterized by the presence of complex overlearned maladaptive patterns of neural functioning. Cognitive training must therefore be designed to induce specific and substantial distributed changes in cortical and subcortical representations and processing efficiency. It must also be delivered in a scalable manner that is engaging and motivating for the learner.
• We propose that several considerations from basic and clinical neuroscience should inform the design of the next generation of cognitive training approaches for the impaired brain: (1) training must address any significant limitations in perceptual and pre-attentive processing due to the critical interactions that link prefrontal predictive operations with perceptual processes and working memory; (2) constrained and intensive training must be employed in order to induce robust and enduring plastic changes in cortex; and (3) training must harness implicit learning mechanisms in order to ‘re-tune’ degraded working memory and long-term memory functions.
• These considerations are supported by a wealth of data from the past two decades of basic research in systems neuroscience. These data demonstrate that (1) the fundamental neural mechanisms supporting learning-induced plasticity are in place throughout life; (2) learning-induced enhancements in lower-level processing can drive improvements in higher-order cognitive operations; that is, successful skill learning induces large-scale distributed changes in cortical representations; and (3) learning-induced plasticity is profoundly influenced by behavioral state and neuromodulatory neurotransmitters.
• These basic science principles can be translated into key elements for the design of cognitive training exercises for the impaired human brain. Such elements include (1) use of stimuli and exercises that drive plasticity in both lower and higher levels of processing in impaired neural systems; that is, precise engineering of stimuli and tasks to improve the speed and accuracy of information processing targeting the impaired neural system(s) of interest; (2) highly intensive training schedules of carefully controlled and constrained learning events, as well as individualized adaptation of task difficulty to drive learning and to preserve reward schedules; and (3) frequent and repetitive engagement of attention and reward systems in the brain, and attention to the psychopharmacologic status of the learner.
• Early research using computerized cognitive training based on these principles is very promising. Data from trials in the elderly, in adults with schizophrenia, and in children with attention deficit disorder, demonstrate robust effect sizes, generalization to untrained tasks, durability of effects, evidence of plasticity in both frontal and sensory systems, and a relationship with improved functioning. Studies are underway using this approach in autism, anxiety disorders, PTSD, bipolar illness, and traumatic brain injury. New collaborations between clinical neuroscientists and experts in entertainment software suggest an emerging era of highly engaging ‘neural network training’ that can potentially occur on a massive scale.
Appendix
DEFINITION OF KEY TERMS
Neural Systems: Groups of neuronal assemblies that interact with each other and the environment to drive a physiological system (eg, visual perception).
Neural Networks: Groups of neurons that are chemically or functionally associated to perform a specific set of computations. Sometimes used interchangeably with Neural Systems.
Cortical Representations: Neuronal ensembles in cortex that are devoted to representing behaviorally important stimuli.
Neuroplasticity/Brain Plasticity: The ability of the human brain to change as a result of experience.
Neural Inputs: The integration of spatial and temporal electrical and chemical information a neuron receives (or a group of neurons receive); input information may be related to sensory data (from the external world) or cognitive data (from the internal world).
Neural Outputs: The electrical and chemical information a neuron transmits (or a group of neurons transmits). Output information may result in motor or cognitive actions.
Sensory Processing/Perceptual Processing: The processing of information received through our sense organs from the environment.
Perceptual Learning: The process that generates long-lasting improvement in the performance of perceptual tasks (ie, evaluating, organizing, and responding to information received from sense organs).
Pre-attentive processing: Early or lower-level operations on sensory data that precede conscious awareness or focused attention. These occur very rapidly in low-level sensory systems, typically within 200 ms or less after stimulus onset, and are often assessed using event-related potentials. Both stimulus salience and expectancy can influence pre-attentive processes.
Working Memory: The short-term temporary storage and manipulation of the information necessary for higher-order cognitive tasks.
Implicit Learning and Memory: The encoding and learning of complex information without conscious awareness of what has been learned.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Vinogradov, S., Fisher, M. & de Villers-Sidani, E. Cognitive Training for Impaired Neural Systems in Neuropsychiatric Illness. Neuropsychopharmacol 37, 43–76 (2012). https://doi.org/10.1038/npp.2011.251
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2011.251
Keywords
This article is cited by
-
Computer-based multiple component cognitive training in children with ADHD: a pilot study
Child and Adolescent Psychiatry and Mental Health (2023)
-
Synaptic plasticity and mental health: methods, challenges and opportunities
Neuropsychopharmacology (2023)
-
Assessing Trial-to-Trial Variability in Auditory ERPs in Autism and Schizophrenia
Journal of Autism and Developmental Disorders (2023)
-
Prospective longitudinal assessment of sensorimotor gating as a risk/resiliency factor for posttraumatic stress disorder
Neuropsychopharmacology (2022)
-
A Systematic Review and Meta-Analysis of Cognitive Training in Adults with Major Depressive Disorder
Neuropsychology Review (2022)