Abstract
Objective:
The objective of this study was to determine whether arrhythmia in the setting of maternal cardiac disease (MCD) affects perinatal outcomes.
Study Design:
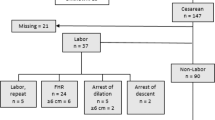
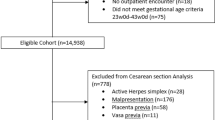
This is a retrospective cohort study of pregnant women with MCD who delivered during 2008 to 2013. Perinatal outcomes among women with an arrhythmia were compared with those without.
Results:
Among 143 women, 36 (25%) had an arrhythmia. Those with an arrhythmia were more likely to have a spontaneous vaginal delivery (64 vs 43%, P<0.05) and required fewer operative vaginal births (8 vs 27%, P=0.02). Pregnancies were more likely to be complicated by intrauterine growth restriction (IUGR) (17 vs 5%, P<0.05), although there were no differences in the rate of small for gestational age. The risk of IUGR remained increased after controlling for confounding (adjusted odds ratio 6.98, 95% confidence interval 1.59 to 30.79, P=0.01). Two cases of placental abruption were identified among mothers with arrhythmia while none were identified in the controls (P<0.05).
Conclusion:
Patients with arrhythmias were more likely to have a spontaneous vaginal delivery. Our data suggest that these pregnancies were an increased risk for IUGR.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Huisman CM, Zwart JJ, Roos-Hesselink JW, Duvekot JJ, van Roosmalen J . Incidence and predictors of maternal cardiovascular mortality and severe morbidity in the Netherlands: a prospective cohort study. PLoS ONE 2013; 8 (2): e56494.
Alonso-Gonzalez R, Swan L . Treating cardiac disease in pregnancy. Women's Health 2014; 10 (1): 79–90.
Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation 2001; 104 (5): 515–521.
Gowda RM, Khan IA, Mehta NJ, Vasavada BC, Sacchi TJ . Cardiac arrhythmias in pregnancy: clinical and therapeutic considerations. Int J Cardiol 2003; 88 (2–3):129–133.
Laksman Z, Harris L, Silverside CK . Cardiac arrhythmias during pregnancy: a clinical approach. Fetal and Maternal Medicine Review 2011; 22: 123–143.
Enriquez AD, Economy KE, Tedrow UB . Contemporary management of arrhythmias during pregnancy. Circ Arrhythm Electrophysiol 2014; 7 (5): 961–967.
Hoffman JIE, Kaplan S, Liberthson RR . Prevalence of congenital heart disease. Am Heart J 2004; 147 (3): 425–439.
Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA . Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005; 366 (9499): 1797–1803.
Ray JG, Schull MJ, Kingdom JC, Vermeulen MJ . Heart failure and dysrhythmias after maternal placental syndromes: HAD MPS Study. Heart 2012; 98 15 1136–1141.
Ersbøll AS, Hedegaard M, Søndergaard L, Ersbøll M, Johansen M . Treatment with oral beta-blockers during pregnancy complicated by maternal heart disease increases the risk of fetal growth restriction. BJOG 2014; 121 (5): 618–626.
European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM) European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Regitz-Zagrosek V European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Blomstrom Lundqvist C European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Borghi C European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Cifkova R European Society of Gynecology (ESG), Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM), Ferreira R et al. ESC Guidelines on the management of cardiovascular diseases during pregnancy: The Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011; 32 (24): 3147–3197.
McAnulty JH . Arrhythmias in pregnancy. Cardiol Clin 2012; 30 (3): 425–434.
Alexander GR, Kogan MD, Himes JH, Alexander GR . 1994-1996 U.S. singleton birth weight percentiles for gestational age by race, Hispanic origin and gender. Maternal. Child Health J 1999; 3 (4): 231–455.
Acknowledgements
We would like to acknowledge Ms Valerie Bosco, NP, for her invaluable contribution to the study and her tireless dedication to UCSF PACT program patients. Dr Katherine Bianco was supported by the Eunice Kennedy Shiever NIH/NICHD Clinical Investigator Award (K08HD069518-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Henry, D., Gonzalez, J., Harris, I. et al. Maternal arrhythmia and perinatal outcomes. J Perinatol 36, 823–827 (2016). https://doi.org/10.1038/jp.2016.90
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.90
This article is cited by
-
Association between the number of pregnancies and cardiac target organ damages: a cross-sectional analysis of data from the Korean women’s chest pain registry (KoROSE)
BMC Women's Health (2023)
-
Comparison of minimal versus zero-fluoroscopic catheter ablation in gestational supraventricular arrhythmias
Journal of Interventional Cardiac Electrophysiology (2022)
-
Cardiac Arrhythmias and Pregnancy
Current Treatment Options in Cardiovascular Medicine (2018)