Abstract
Background and aims:
In a population-based cohort study with older subjects and without specific interventions, we investigated the impact of body mass index (BMI) and BMI change (as well as waist circumference and change of waist circumference) on reversion from prediabetes to normal glucose tolerance (NGT) and on long-term persistence of NGT.
Materials and methods:
Oral glucose tolerance tests were conducted at baseline and at follow-up in a cohort study in Southern Germany (KORA S4/F4; 1223 subjects without diabetes aged 55–74 years at baseline in 1999–2001; 887 subjects (73%), of whom 436 had prediabetes at baseline, participated in the follow-up 7 years later).
Results:
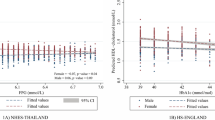
BMI reduction, but not initial BMI, predicted reversion from prediabetes to NGT. The odds ratio (OR) for returning to NGT was 1.43 (95% CI: 1.18–1.73) for a BMI decrease of 1 kg m−2, after adjustment for age, sex, baseline glucose values and lifestyle factors. Initial BMI had no effect on reversion to NGT (OR=0.98, 95% CI: 0.91–1.06, per kg m−2). Persistence of NGT was associated with baseline BMI (OR=0.94, 95% CI: 0.88–0.998) and BMI reduction (OR=1.16, 95% CI: 1.02–1.33, per decrease by 1 kg m−2). For waist circumference and change of waist circumference similar results were obtained.
Conclusion:
In older adults, weight loss strongly increased the chances of returning from prediabetes to NGT irrespective of initial BMI. Long-term persistence of NGT depended both on initial BMI and on BMI change.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Wannamethee SG, Papacosta O, Whincup PH, Carson C, Thomas MC, Lawlor DA et al. Assessing prediction of diabetes in older adults using different adipositas measures: a 7 year prospective study in 6923 older men and women. Diabetologia 2010; 53: 890–898.
Qin L, Knol MJ, Corpeleijn E, Stolk RP . Does physical activity modify the risk of obesity for type 2 diabetes: a review of epidemiological data. Eur J Epidemiol 2010; 25: 5–12.
Oguma Y, Sesso HD, Paffenbarger RS, Lee IM . Weight change and risk of developing type 2 diabetes. Obesity Res 2005; 13: 945–951.
Koh-Banerjee P, Wang Y, Hu FB, Spiegelman D, Willett WC, Rimm EB . Changes in body weight and body fat distribution as risk factors for clinical diabetes in US men. Am J Epidemiol 2004; 159: 1150–1159.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention of metformin. N Engl J Med 2002; 346: 393–403.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Qiao Q, Keinänen-Kiukaanniemi S, Rajala U, Uusimäki A, Kivelä SL . Risk for diabetes and persistent impaired glucose tolerance among middle-aged Finns. Diabetes Res Clin Pract 1996; 33: 191–198.
Forouhi NG, Luan J, Hennings S, Wareham NJ . Incidence of Type 2 diabetes in England and its association with baseline impaired fasting glucose: The Ely study 1990-2000. Diabet Med 2007; 24: 200–207.
Kleber M, Lass N, Papcke S, Wabitsch M, Reinehr T . One-year follow-up of untreated obese white children and adolescents with impaired glucose tolerance: high conversion rate to normal glucose tolerance. Diabet Med 2010; 27: 516–521.
Weiss R, Taksali SE, Tamborlane WV, Burgert TS, Savoye M, Caprio S . Predictors of changes in glucose tolerance status in obese youth. Diabetes Care 2005; 28: 902–909.
Janghorbani M, Amini M . Normalization of glucose intolerance in first-degree relatives of patients with type 2 diabetes. Diabetes Res Clin Pract 2010; 88: 295–301.
Alvarsson M, Hilding A, Östenson CG . Factors determining normalization of glucose intolerance in middle-aged Swedish men and women: a 8-10-year follow-up. Diabet Med 2009; 26: 345–353.
Wong MS, Gu K, Heng D, Chew SK, Chew LS, Tai ES . The Singapore impaired glucose tolerance follow-up study. Diabetes Care 2003; 26: 3024–3030.
Shimizu S, Kawata Y, Kawakami N, Aoyama H . Effects of changes in obesity and exercise on the development of diabetes and return to normal fasting plasma glucose levels at one-year follow-up in middle-aged subjects with impaired fasting glucose. Environ Health Prev Med 2001; 6: 127–131.
Hiltunen L, Kivelä SL, Läärä E, Keinänen-Kiukaanniemi S . Progression of normal glucose tolerance to impaired glucose tolerance or diabetes in the elderly. Diabetes Res Clin Pract 1997; 35: 99–106.
Henkel E, Köhler C, Temelkova-Kurktschiev T, Hanefeld M . Predictors of abnormal glucose tolerance in persons at risk of type 2 diabetes: the RIAD study. Dtsch Med Wochenschr 2002; 127: 953–957.
Ferrannini E, Nannipieri M, Williams K, Gonzales C, Haffner SM, Stern MP . Mode of onset of type 2 diabetes from normal or impaired glucose tolerance. Diabetes 2004; 53: 160–165.
Genuth S, Alberti KGMM, Bennett P, Buse J, Defronzo R, Kahn R et al. The expert committee on the diagnosis and classification of diabetes mellitus: follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003; 26: 3160–3167.
Rathmann W, Haastert B, Icks A, Löwel H, Meisinger C, Holle R et al. High prevalence of undiagnosed diabetes mellitus in Southern Germany: target populations for efficient screening. The KORA Survey 2000. Diabetologia 2003; 46: 182–189.
Winkler G, Döring A . Validation of a short qualitative food frequency list used in several German large scale surveys. Z Ernaehrungswiss 1998; 37: 234–241.
Raji A, Seely EW, Arky RA, Simonson DC . Body fat distribution and insulin resistance in healthy asian indians and caucasians. J Clin Endocrinol Metab 2001; 86: 5366–5371.
Nyamdorj R, Pitkäniemi J, Tuomilehto J, Hammar N, Stehouwer CDA, Lam TH et al. Ethnic comparison of the association of undiagnosed diabetes with obesity. Int J Obes 2010; 34: 332–339.
Shai I, Jiang R, Manson JE, Stampfer MJ, Willett WC, Colditz GA et al. Ethnicity, obesity, and risk of type 2 diabetes in women: a 20-year follow-up study. Diabetes Care 2006; 29: 1585–1590.
Balion CM, Raina PS, Gerstein HC, Santaguida PL, Morrison KM, Booker L et al. Reproducibility of impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) classification: a systematic review. Clin Chem Lab Med 2007; 45: 1180–1185.
Acknowledgements
The Diabetes Cohort Study was funded by a German Research Foundation project grant to the second author (DFG; RA 459/2-1). The German Diabetes Center is funded by the German Federal Ministry of Health, and the Ministry of Innovation, Science, Research and Technology of the State of North-Rhine-Westfalia. The KORA research platform and the KORA Augsburg studies are financed by the Helmholtz Zentrum München, German Research Center for Environmental Health, which is funded by the German Federal Ministry of Education, Science, Research and Technology and by the State of Bavaria. We thank the field staff in Augsburg who were involved in the conduct of the studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Kowall, B., Rathmann, W., Heier, M. et al. Impact of weight and weight change on normalization of prediabetes and on persistence of normal glucose tolerance in an older population: the KORA S4/F4 study. Int J Obes 36, 826–833 (2012). https://doi.org/10.1038/ijo.2011.161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.161
Keywords
This article is cited by
-
Prediabetes and risk of mortality, diabetes-related complications and comorbidities: umbrella review of meta-analyses of prospective studies
Diabetologia (2022)
-
The heterogeneity of reversion to normoglycemia according to prediabetes type is not explained by lifestyle factors
Scientific Reports (2021)
-
Impact of weight gain on the evolution and regression of prediabetes: a quantitative analysis
European Journal of Clinical Nutrition (2017)
-
Weight Loss and Physical Activity for Disease Prevention in Obese Older Adults: an Important Role for Lifestyle Management
Current Diabetes Reports (2014)
-
Longitudinal changes in health-related quality of life in normal glucose tolerance, prediabetes and type 2 diabetes: results from the KORA S4/F4 cohort study
Quality of Life Research (2014)