Abstract
Patients with coarctation of the aorta develop early onset hypertension in spite of early effective repair. This is associated with significant morbidity and is arguably the single most important outcome variable in this patient group. We discuss the potential pathophysiological mechanisms involved in the development of hypertension with clinical reference to monozygotic twins, and review potential strategies for therapy and prevention in this setting.
Similar content being viewed by others
Main
Coarctation of the aorta (CoA) is classically manifest by a discrete congenital narrowing of the aortic isthmus. It occurs in approximately 1 in 2500 live births and is more prevalent in males.1, 2, 3 Most patients present in infancy, either acutely due to heart failure following closure of the arterial duct, or on routine screening due to absence of the femoral arterial pulse. Some patients will not present until later life due to either a less significant narrowing or rapid post-natal development of collateral circulation that maintains adequate blood supply to the lower body. Treatment of choice in infancy is surgical repair with excellent short-to-medium term outcomes.4 In older patients transcatheter management with endovascular stenting is preferable to surgery in many institutions, and provides relief of pressure gradients across the coarctation site.5 However in both circumstances patients have significant longer term risk for the development of hypertension.6, 7, 8, 9 Indeed, some reports claim that hypertension is the single most important long-term outcome variable in patients with repaired CoA.9 Hypertension is associated with significant morbidity and early mortality and although early treatment appears to delay the onset of hypertension,10 remarkably one third of CoA patients still become hypertensive by adolescence despite early and effective surgical repair.11 Data beyond adolescence show increasing prevalence with age, and by 50–72 years 90% of patients have documented hypertension.12 This suggests that hypertension may be an inevitable consequence of CoA, even when an effective anatomical repair has been achieved early in life. Although it is unclear why this may be the case, it is postulated that there is dysfunction of the normal control mechanisms regulating blood pressure during growth and development in patients with repaired CoA. Identifying and preventing such maladaptive processes in CoA presents a challenge that if successful, will provide more effective treatment in the future.
We discuss these early changes in the setting of male monozygotic twins, one with CoA and the other without, and report results of detailed vascular and autonomic assessment in both infants, changes in which have been postulated as major mechanisms driving hypertension following surgical repair.13, 14, 15, 16 We review the current literature to question whether developmental consequences of CoA condemn individuals to lifelong hypertension, and evaluate whether current treatment strategies are appropriate or whether more targeted interventions could counter the blood pressure dysregulation that is associated with CoA.
Early change—a case in point
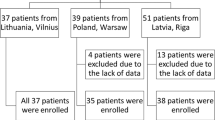
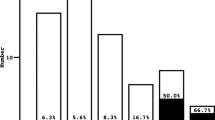
Previously reported data have suggested increased aortic stiffness17 and alteration in autonomic cardiac balance18 in pre-operative neonates with CoA, suggesting an early maladaptive response to mechanisms responsible for longer term blood pressure control (discussed below). With this in mind, we measured non-invasive indices of autonomic balance, large artery stiffness and cardiac output in an 8-month-old male with native CoA and his monozygotic twin. The index case was diagnosed following detection of systolic hypertension (130 mm Hg—95th percentile for patient's length is 104 mm Hg19) while undergoing anesthesia for assessment of airway stridor. Subsequent magnetic resonance imaging demonstrated severe CoA distal to the left subclavian artery, with several collaterals arising from the left subclavian and carotid arteries (Figure 1). Spontaneous baroreceptor reflex sensitivity (sBRS) was analyzed using sequence analysis. To evaluate sympatho-vagal balance both time domain and frequency domain indices of heart rate variability, and frequency domain analysis of blood pressure variability were performed. These assessment techniques have previously been described in detail.20 Pulse wave velocity as an indicator of large artery stiffness was measured in the right arm using a validated21 pulse volume recording technique (Vicorder, Skidmore Medical, Bristol, UK), with an inflatable cuff placed proximally and distally on the limb of interest. Cardiac output was measured non-invasively using electrical velocimetry (ICON, Osypka Medical, Berlin, Germany). This is a transthoracic bioimpedence technique that detects changes in thoracic fluid shifts based on changes in transthoracic conductivity, due to alignment of the erythrocytes during early systole, and shows excellent correlation with direct Fick estimates of cardiac output in patients with congenital heart disease.22 The measurement readings including average resting blood pressure over three recordings are listed in Table 1. Although no meaningful statistical analyses of these data can be made, it is notable that the sBRS was markedly lower in the index case suggesting dampening of the baroreceptor reflex, as demonstrated previously in infants with CoA.18 Time domain analyses of heart rate variability were higher in the control twin across all measurements (Figure 2), suggesting dominance of parasympathetic over sympathetic modulations in the control infant although wide variability may exist with these indices. Right arm pulse wave velocity values were repeatedly higher in the index case again suggesting large artery stiffness, implicated in systolic hypertension may be affected in the pre-CoA arterial bed, although it is unclear whether this is a consequence or a cause of high systolic blood pressure in this case. Repeat measurements following surgery on the index case were not carried out as continued therapy with a beta-blocker, which was required to control blood pressure, therefore acting as a confounding variable on the recorded parameters.
Contrast magnetic resonance image in the sagittal plane demonstrating the heart anteriorly and descending aortic arch and descending aorta posteriorly. Discrete coarctation of the aorta is indicated by the white arrow after the origin left subclavian artery. Numerous prominent collateral arteries providing collateral flow are seen.
Graphical representation of heart rate variability indicating number of successive normal-to-normal RR intervals greater than 5, 10, 20, 30, 40 and 50 ms expressed as a ratio of the total number of normal-to-normal RR intervals in the recording period (pNN5, 10, and so on). The variability is more pronounced in the control twin at all intervals indicating greater high-frequency variations in HR, representative of more pronounced parasympathetic modulation of heart rate variability.
Potential mechanisms involved in the hypertensive response
The trend in these measurements is consistent with previous reports suggesting reduced arterial compliance and blunted sBRS in infants with CoA, compared with controls.17, 18 The genetic homogeneity in this case is interesting and provides a unique opportunity to assess variances in arterial compliance, BRS and cardiac autonomic balance between twin infants, and postulates on how this may affect longer term control of blood pressure.
Hypertension in patients following CoA repair provides a unique insight into the developmental pathophysiology of blood pressure control. Earlier age of repair appears to be somewhat protective, and current practice is to perform surgical repair in neonatal life. However even in these cases there is a period of adequate control in the early years following surgical repair, with significant rises in systolic blood pressure with increasing age. Prevalence ranges vary according to the report; however many investigators would accept that hypertension is an inevitable consequence of CoA. For example, Clarkson et al.6 reported on 160 patients and observed that only 20% of patients were alive without complications and with a normal blood pressure at 25 years follow-up. As discussed, malfunction in a number of systems has been implicated including autonomic control of blood pressure,13, 14 impaired vascular function15, 16 and hyperactivation of the renin-angiotensin system;23, 24 however, studies to date have mostly concentrated on individual systems.
Endothelial dysfunction
Apart from reduced arterial compliance and blunted baroreceptor sensitivity, other systems have been implicated in the early hypertensive response seen in post-operative CoA patients. Reduced endothelial function has been demonstrated in post-coarctectomy patients, and has been suggested as a cause of hypertension. Reduced vascular reactivity appears to be restricted to the pre-stenotic arterial tree,25 and subsequent studies have demonstrated that these changes do not appear to be related to timing of surgery suggesting early changes in control of vascular reactivity.10, 26 Whether this represents early programming is unclear, as this mechanism has not been studied in young pre-operative patients, and adult studies generally recognize endothelial dysfunction as a consequence rather than a cause of hypertension. Diffuse endothelial dysfunction is also likely to affect peripheral vascular resistance, which has the most profound effects on mean and diastolic blood pressure values rather than systolic values and pulse pressure that are commonly raised in hypertensive CoA patients.
Renin-angiotensin system
Early studies examining the impact of the renin-angiotensin system on hypertension in CoA, concentrated on plasma renin levels with equivocal results, mostly demonstrating no significant increases in these levels in CoA patients.27, 28, 29 Subsequent studies have evaluated renin levels following alterations to resting homeostasis, such as fluid depletion or exercise.30, 31 Although Parker et al.30 demonstrated increased pre-operative plasma renin levels following significant volume depletion, the subjects studied were older children (5–16 years) and the values were normalized post-operatively including in those who remained hypertensive, thereby making a causal link for sustained long-term hypertension unlikely. Currently most centers repair CoA in neonatal life, and thus a prolonged period of renal hypoperfusion is not normal with transductal flow ensuring adequate renal perfusion before birth. In patients with late presentation of CoA, there is often significant collateral circulation ensuring that renal perfusion is not significantly affected. However, hypertension remains common suggesting that persistently elevated levels of renal renin or angiotensin are not the primary mechanism involved in the development of long-term hypertension in these patients. It is less clear whether the upper body blood pressure increases, seen with developing coarctation, induce changes in the overall number or sensitivity of angiotensin II type I receptors in the brain. Sangaleti et al.32 have demonstrated that coarctation hypertension in the rat is associated with hyperactivity of the brain renin-angiotensin system as indicated by increased expression of angiotensin II type I receptors mRNA in brainstem areas, known to participate in cardiovascular control. It is possible that these receptors are involved in the progression of hypertension in post-coarctectomy patients involving the cardiac baroreceptor. This is more likely than a direct effect of angiotensin II on the arteriolar bed, as this would not explain the differential changes seen in the upper and lower body although it is possible that tissue angiotensin II production may be increased from vessels exposed to high-shear stress. Also the expected effect of increased peripheral vascular resistance with angiotensin II is not typical of the systolic hypertension seen in CoA.
Multiple system involvement
It is possible that more than one of the systems described above are involved in the delayed hypertensive response seen in patients following CoA repair. Initial evidence for links between abnormal arterial structure and baroreceptor functioning was suggested by Sehested et al.14 The authors examined fresh resected coarctation tissue and demonstrated reduced isometric tension induced by potassium, noradrenaline and prostaglandin in the pre-stenotic aortic tissue compared with the post-stenotic area indicating reduced contractility of the pre-stenotic aorta. This was associated with increased collagen and reduced smooth muscle content of the pre-stenotic aortic wall. The authors postulated that aortic arch baroreceptors in this pre-stenotic area may be activated less at a given pressure than receptors placed in a vessel, with normal distensibility thus allowing a higher pressure to be tolerated by the cardiac baroreflex. The inter-relationship between reduced arterial compliance and a less sensitive baroreceptor reflex has been examined in other forms of secondary hypertension,33 but has yet to be reported in patients with CoA. The progression in this inter-relationship throughout childhood when control mechanisms are potentially set for life, is also of significant interest. For example, it is unclear whether the baroreceptor reflex is dysfunctional from an early age, and is therefore predictive of those likely to develop hypertension, or whether it becomes progressively less sensitive throughout childhood in conjunction with changes in vascular function. Our group has previously demonstrated a reduction in baroreceptor gain and heart rate variability of approximately 40% in pre-operative neonates, with CoA compared with controls, suggesting early maladaptive autonomic control of blood pressure.18 We postulated that failure of these control mechanisms to normalize in some patients could cause long-term impediments to normal blood pressure control, possibly leading to hypertension. Since then we have followed up this group of patients and found that the initial autonomic dysfunction between the two groups had normalized by 5 years of age.20 As there was no difference in blood pressure between the two groups at this early age, it is difficult to be sure of the implications of these findings, but they do mirror findings in animal work.34 As previously mentioned, similar studies have been carried out in neonates looking at aortic compliance in order to examine the effects of CoA on fetal and early neonatal arterial stiffness. Vogt et al.17 measured local arterial stiffness indices and distensibility in the ascending and descending aortas of pre- and post-operative CoA neonates, and compared these values to matched controls. The authors demonstrated significantly reduced distensibility and increased stiffness indices in the ascending aortas of the pre- and post operative group, when compared with controls. There was no difference in the elastic properties of the descending aorta between the two groups. The same group was prospectively re-evaluated at 3 years of age, and aortic elastic properties were measured in a similar fashion.35 Persisting impairment of local elastic properties of the ascending aorta was noted in the CoA group, when compared with controls; however, again correlation between these findings and the longer term risk of hypertension was not possible.
As the studies discussed above have not been able to correlate changes in autonomic control or arterial compliance to blood pressure values, we recruited adolescent CoA patients and related autonomic, vascular and cardiac output measurements to ambulatory blood pressure.36 Our results are similar to those of previous studies demonstrating a 30% incidence of hypertension in this age group, despite early effective surgical repair. We demonstrated increased aortic pulse wave velocity in the hypertensive CoA patients, compared with both normotensive CoA patients and controls. This was associated with a compensatory increase in sBRS in the normotensive CoA group compared with controls, which is not present in the hypertensive group. There was also a reduction in stroke volume in the normotensive group compared with the hypertensive group, suggesting the possibility that increased sBRS in the normotensive CoA group may generate normal blood pressure control via effects on cardiac output. Failure of this control mechanism may be the final pathway to establishing hypertension in these patients.
Treatment
In the case discussed above, the CoA twin was treated before surgery with atenolol due to some evidence that beta-blockade reduces the degree of acute post-operative hypertension.37 Commonly, patients develop significant increases in their blood pressure in the early post-operative phase. Reports have suggested that this is related to resetting of the systemic arterial baroreceptor to the elevated blood pressure.13, 14 The subsequent acute unloading of the baroreceptors in the post-operative phase may then lead to an increase in sympathetic outflow, and thus an increase in arterial pressure.38 There appears to be a phase of adaptation following surgery and in most cases where early surgical repair has taken place, blood pressure settles down to normal levels throughout early childhood. However, increases in both resting- and exercise-induced blood pressure are reported from adolescence. Indeed exercise-induced hypertension is thought to predict the onset of established hypertension, and is therefore considered important in the overall assessment of this patient group.39, 40 It is possible that the increases in cardiac output, seen with exercise, ejected into a less compliant aorta lead to significant increases in systolic blood pressure, which normalizes when cardiac output returns to normal. Further aortic remodeling and stiffening induced by continuing low velocity shear may lead to changes in baroreceptor sensitivity and progression toward established hypertension.
However, without fully understanding the exact mechanisms involved in the development of established hypertension in patients with CoA, optimum medical treatment cannot be fully elucidated. Most published reports focus on treatment of early post-operative hypertension; however, it is the established increases in systolic blood pressure that are associated with long-term morbidity and mortality and thus should be the focus of our attention. It is clear from numerous studies that hypertension is inadequately treated in these patients,11, 12 with Hager et al.12 demonstrating up to 40% of patients with established hypertension in the setting of repaired CoA are without anti-hypertensive medication. The mainstay of treatment in many units consists of continuation of initial therapy with beta-blockade, and although there is some evidence that this may be effective against mechanisms driving hypertension in the early post-operative phase, there are no published data on its efficacy in older patients with established disease. A recent report has demonstrated that ramipril decreases the expression of pro-inflammatory cytokines in normotensive patients with CoA.41 Targeting agents with potential anti-inflammatory effects may be prudent, as the endothelial dysfunction seen in patients with CoA may be a consequence of inflammation driven by abnormal flow dynamics at the repair site, or as a consequence of a more widespread vasculopathy as part of the ‘syndrome’ of CoA. Either way, more vigilant follow-up of blood pressure is required along with trials of anti-hypertensive agents in CoA, in order to determine the most appropriate agent to control blood pressure.
A more important question may be whether we can alter the course of changes in blood pressure with early treatment. It is accepted that early surgical intervention reduces the incidence of hypertension on follow-up, but whether or not this merely delays onset is not yet clear, with most recent data suggesting the latter.11 Early surgery limits the time period in which the aortic arch and arterial baroreceptor system is subjected to increased blood pressure, as well as the arterial remodeling that may accompany the upper body hypertension. It is possible that early prophylactic treatment for hypertension with targeted agents may prevent changes that are associated with hypertension from occurring, and thus improve the long-term outlook for these patients. Significant work remains to be done to provide the platform for such therapies.
References
Anderson R, Baker EJ, Macartney FJ, Rigby ML, Shinebourne EA, Tynan M . Paediatric Cardiology (2nd Edition). London: Churchill Livingstone, 2002.
Samanek M, Voriskova M . Congenital heart disease among 815 569 children born between 1980 and 1990 and their 15-year survival: a prospective bohemia survival study. Ped Cardiol 1999; 20: 411–417.
Fyler DC BD, Hellenbrand WC, Cohn HE . Report on the new England regional infant cardiac program. Pediatrics 1980; 65: 375–461.
Kaushal SBC, Patel JN, Patel SK, Walker BL, Weigel TJ, Randolph G, Wax D, Mavroudis C . Coarctation of the aorta: midterm outcomes of resection with extended end-to-end anastomosis. Ann Thorac Surg 2009; 88: 1932–1938.
Hamdan MA, Maheshwari S, Fahey JT, Hellenbrand WE . Endovascular stents for coarctation of the aorta: Initial results and intermediate-term follow-up. J Am Coll Cardiol 2001; 38: 1518–1523.
Clarkson PM, Nicholson MR, Barrattboyes BG, Neutze JM, Whitlock RM . Results after repair of coarctation of the aorta beyond infancy—a 10 year to 28 year follow-up with particular reference to late systemic hypertension. Am J Cardiol 1983; 51: 1481–1488.
Koller M, Rothlin M, Senning A . Coarctation of the aorta—review of 362 operated patients—long-term follow-up and assessment of prognostic variables. Eur Heart J 1987; 8: 670–679.
Maron BJ, Humphrie JO, Rowe RD, Mellits ED . Prognosis of surgically corrected coarctation of aorta—20-year postoperative appraisal. Circulation 1973; 47: 119–126.
Cohen M, Fuster V, Steele PM, Driscoll D, McGoon DC . Coarctation of the aorta—long-term follow-up and prediction of outcome after surgical-correction. Circulation 1989; 80: 840–845.
de Divitiis M, Pilla C, Kattenhorn M, Zadinello M, Donald A, Leeson P, Wallace S, Redington A, Deanfield JE . Vascular dysfunction after repair of coarctation of the aorta—impact of early surgery. Circulation 2001; 104: I165–I170.
O’Sullivan JJ, Derrick G, Darnell R . Prevalence of hypertension in children after early repair of coarctation of the aorta: a cohort study using casual and 24 h blood pressure measurement. Heart 2002; 88: 163–166.
Hager A, Kanz S, Kaemmerer H, Schreiber C, Hess J . Coarctation long-term assessment (COALA): significance of arterial hypertension in a cohort of 404 patients up to 27 years after surgical repair of isolated coarctation of the aorta, even in the absence of restenosis and prosthetic material. J Thorac Cardiovasc Surg 2007; 134: 738–745.
Johnson D, Perrault H, Vobecky SJ, Trudeau F, Delvin E, Fournier A, Davignon A . Resetting of the cardiopulmonary baroreflex 10 years after surgical repair of coarctation of the aorta. Heart 2001; 85: 318–325.
Sehested J, Baandrup U, Mikkelsen E . Different reactivity and structure of the pre-stenotic and post-stenotic aorta in human coarctation—implications for baroreceptor function. Circulation 1982; 65: 1060–1065.
Brili S, Dima I, Ioakeimidis N, Alexopoulos N, Vlachopoulos C, Antoniades C, Tousoulis D, Stefanadis C . Evaluation of aortic stiffness and wave reflections in patients after successful coarctation repair. Eur Heart J 2005; 26: 1394.
De Divitiis M, Kattenhorn M, Donald AE, Zadinello M, Pilla CB, Leeson P, Wallace S, Redington AN, Deanfield JE . Reduced vascular function determines high blood pressure and increased left ventricular mass in patients with repaired aortic coarctation. Circulation 2000; 102: II .768.Abstract.
Vogt M, Kuhn A, Baumgartner D, Baumgartner C, Busch R, Kostolny M, Hess J . Impaired elastic properties of the ascending aorta in newborns before and early after successful coarctation repair—proof of a systemic vascular disease of the prestenotic arteries? Circulation 2005; 111: 3269–3273.
Polson JW, McCallion N, Waki H, Thorne G, Tooley MA, Paton JFR, Wolf AR . Evidence for cardiovascular autonomic dysfunction in neonates with coarctation of the aorta. Circulation 2006; 113: 2844–2850.
Roccella EJ . The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114: 555–576.
Kenny D, Polson JW, Martin RP, Paton JFR, Wolf AR . Normalization of autonomic function in children with coarctation of the aorta after surgical correction in infancy. Hypertension 2009; 54: E21–E22.
Hickson SS BM, Broad J, Avolio AP, Wilkinson IB, McEniery CM . Validity and repeatability of the vicorder apparatus: a comparison with the sphygmocor device. Hypertension Res 2009; 32: 1079–1085.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H . Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth 2008; 100: 88–94.
Langdorn T, Boerboom L, Declusin R, Olinger G, Bonchek L, Liu TZ . Renin activity in aortic coarctation repair. Am Heart Assoc Monogr 1986; II-467 (Abstract).
Parker FBJ, Streeten DHP, Farrell B, Blackman MS, Sondheimer HM, Anderson GHJ . Pre operative and post operative renin levels in coarctation of the aorta. Circulation 1982; 66: 513–514.
Gidding SS, Rocchini AP, Moorehead C, Schork MA, Rosenthal A . Increased forearm vascular reactivity in patients with hypertension after repair of coarctation. Circulation 1985; 71: 495–499.
de Divitiis M, Rubba P, Calabro R . Arterial hypertension and cardiovascular prognosis after successful repair of aortic coarctation: a clinical model for the study of vascular function. Nutr Metab Cardiovasc Dis 2005; 15: 382–394.
Amsterdam EA, Albers WH, Christli AR, Morgan CL, Nadas AS, Hickler RB . Plasma renin activity in children with coarctation of aorta. Am J Cardiol 1969; 23: 396–399.
Markiewicz A, Wojczuk D, Kokot F, Cicha A . Plasma-renin activity in coarctation of aorta before and after surgery. Br Heart J 1975; 37: 721–725.
Werning C, Schonbec M, Weidmann P, Baumann K, Gysling E, Wirz P, Siegenth W . Plasma renin activity in patients with coarctation of aorta—a comment on pathogenesis of prestenotic hypertension. Circulation 1969; 40: 731–737.
Parker FB, Farrell B, Streeten DHP, Blackman MS, Sondheimer HM, Anderson GH . Hypertensive mechanisms in coarctation of the aorta—further-studies of the renin-angiotensin system. J Thorac Cardiovasc Surg 1980; 80: 568–573.
Ross RD, Clapp SK, Gunther S, Paridon SM, Humes RA, Farooki ZQ, Pinsky WW . Augmented norepinephrine and renin output in response to maximal exercise in hypertensive coarctectomy patients. Am Heart J 1992; 123: 1293–1299.
Sangaleti CT, Crescenzi A, Michelini LC . Endogenous angiotensin and pressure modulate brain angiotensinogen and at(1a) mrna expression. Hypertension 2004; 43: 317–323.
Chesterton LJ, Sigrist MK, Bennett T, Taal MW, McIntyre CW . Reduced baroreflex sensitivity is associated with increased vascular calcification and arterial stiffness. Nephrol Dial Transplant 2005; 20: 1140–1147.
Igler FO, Boerboom LE, Werner PH, Donegan JH, Zuperku EJ, Bonchek LI, Kampine JP . Coarctation of the aorta and baroreceptor resetting—a study of carotid baroreceptor stimulus-response characteristics before and after surgical repair in the dog. Circ Res 1981; 48: 365–371.
Kuhn A, Baumgartner D, Baumgartner C, Horer J, Schreiber C, Hess J, Vogt M . Impaired elastic properties of the ascending aorta persist within the first 3 years after neonatal coarctation repair. Ped Cardiol 2009; 30: 46–51.
Kenny D, Polson JW, Martin RP, Cockcroft JR, Wilson DG, Caputo M, Paton JFR, Wolf AR . Relationship of aortic pulse wave velocity and baroreceptor sensitivity to blood pressure control in patients with repaired coarctation of the aorta. Cardiol Young 2010; 20 (Supp II): S10–S11.
Gidding SS, Rocchini AP, Beekman R, Szpunar CA, Moorehead C, Behrendt D, Rosenthal A . Therapeutic effect of propranolol on paradoxical hypertension after repair of coarctation of the aorta. N Engl J Med 1985; 312: 1224–1228.
Sealy WC, Harris JS, Young WG, Callaway HA . Paradoxical hypertension following resection of coarctation of aorta. Surgery 1957; 42: 135–147.
Vriend JWJ, van Montfrans GA, Romkes HH, Vliegen HW, Veen G, Tijssen JGP, Mulder BJM . Relation between exercise-induced hypertension and sustained hypertension in adult patients after successful repair of aortic coarctation. J Hypertens 2004; 22: 501–509.
Ou P, Celermajer DS, Mousseaux E, Pedroni E, Brunelle F, Vouhe P, Sidi D, Bonnet D . Exercise-related hypertension predicts resting hypertension, left ventricular and vascular hypertrophy late after coarctation repair. Circulation 2006; 114: 504.
Brill S, Tousoulis D, Antonlades C, Vasilladou C, Karall M, Papageorgiou N, Loakelmidis N, Marinou K, Stefanadi E, Stefanadis C . Effects of ramipril on endothelial function and the expression of proinflammatory cytokines and adhesion molecules in young normotensive subjects with successfully repaired coarctation of aorta. J Am Coll Cardiol 2008; 51: 742–749.
Acknowledgements
We would like to thank the Biomedical Research Unit for their support of this work. Sources of funding: Dr Kenny was funded through a Biomedical Research Unit grant obtained through the National Health Service (NHS). Dr Martin and Professor Wolf were salaried by the NHS. Professor Paton was salaried by the University of Bristol and was a recipient of the Royal Society Wolfson Research Merit Award, and Dr Polson was funded through the British Heart Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kenny, D., Polson, J., Martin, R. et al. Hypertension and coarctation of the aorta: an inevitable consequence of developmental pathophysiology. Hypertens Res 34, 543–547 (2011). https://doi.org/10.1038/hr.2011.22
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.22
Keywords
This article is cited by
-
Coral reef aorta: a rare form of obstruction of the ascending aorta in adolescent with aortopathy- case report
Journal of Cardiothoracic Surgery (2024)
-
Vascular dysfunction caused by loss of Brn-3b/POU4F2 transcription factor in aortic vascular smooth muscle cells is linked to deregulation of calcium signalling pathways
Cell Death & Disease (2023)
-
Cardiovascular Prevention Among Young Adults with Congenital Heart Disease
Current Atherosclerosis Reports (2022)
-
Two decades of aortic coarctation treatment in children; evaluating techniques
Netherlands Heart Journal (2021)
-
Prevalence of arterial hypertension, hemodynamic phenotypes, and left ventricular hypertrophy in children after coarctation repair: a multicenter cross-sectional study
Pediatric Nephrology (2020)