Abstract
Purpose
Treatment of uveal melanoma can impair patients’ psychological well-being. We evaluated patient-reported outcome measures (PROMs) of anxiety, depression, and quality of life (QoL) over 2 years following treatment in a consecutive sample of uveal melanoma patients, compared observations to population normative values and examined whether outcomes differed according to patients’ age, gender, and whether or not they were treated by enucleation or had a poor prognosis (presence of monosomy 3).
Design
Prospective longitudinal study.
Participants
Patients (N=411) with uveal melanoma treated between 2008 and 2011.
Methods
Self-report questionnaire study. We compared mean PROMs scores obtained 6 months, 1 year, and 2 years after treatment to published population normative values using 2-sample t-tests, and tested the association of these scores with gender, age, treatment by enucleation, and monosomy 3 using mixed-model ANOVAs.
Results
On QoL and depression, patients were similar to or better than normative values at all time points, but there was some evidence that females were more anxious than female normative values (Ps<0.001–<0.05). Younger patients (P<0.01) and female patients (P<0.01) were the most anxious overall. Enucleation was not associated with PROMs. Patients with monosomy 3 showed more depressed mood at all the three time points (P<0.05).
Conclusions
Patients treated for uveal melanoma can expect, within 6 months of treatment, to have a QoL that is similar to that of the general population. Younger female patients and patients with monosomy 3 are more likely to be distressed, and clinicians will need to be alert to this.
Similar content being viewed by others
Introduction
Uveal melanoma is the most common primary intraocular malignancy in adults.1 Although useful vision and the eye itself can be conserved in many patients, 50% of patients die of metastatic disease1, 2 with the survival probability varying greatly according to clinical, histological, and genetic factors. However, it is not only the length of survival that is important but also the quality of that survival.
There are many ways in which the quality of life (QoL) of patients with uveal melanoma might be impaired. First, despite recent therapeutic advances, many patients must come to terms with a high chance of premature death from metastatic disease.3 Although survival prognosis, based on genetic analysis of tumour tissue, can be accurately predicted and patients can be informed of their probable life expectancy, patients report uncertainty, and distress across all prognoses.4 Second, most patients need to cope with some degree of visual loss, which may restrict their activities, and some may also be concerned about cosmetic changes caused by treatment.
Measures such as visual acuity, local tumour control, ocular retention, and disease-free survival provide a picture of clinical outcome but do not capture patient well-being. Patient-reported outcome measures (PROMs) assess psychological health and daily functioning. A better understanding of PROMs would enable practitioners to advise patients about how treatment will affect them, and would also help practitioners to target interventions to improve patients’ well-being.
Several authors have investigated PROMs after treatment of uveal melanoma, focusing particularly on QoL and mood, that is, anxiety and depression.5, 6, 7, 8, 9, 10, 11, 12 These studies show conflicting results, possibly due to small sample sizes (Ns ranging between 20 and 99 in most previous studies)5, 6, 9, 10, 11, 12 and underutilisation of prospective designs. The one study with a large sample size (N=209) and a prospective design restricted sampling to medium-sized tumours only, and excluded patients with life-limiting co-morbidities and those whose visual acuity in the fellow eye was poor.7
The aims of the current study were (1) to document anxiety, depression, and QoL over 2 years after treatment in a large consecutive sample of uveal melanoma patients, and (2) to compare these observations with population normative values to ascertain whether, and to what extent, patients are impaired. Younger age and female gender have been associated with poorer psychological outcomes in patients with cancer,13 and there is inconsistent evidence as to whether treatment by enucleation is associated with impaired QoL in ocular melanoma.5, 7, 8, 12 Estimation of high metastatic disease probability is defined in this study by the presence of monosomy 3 in tumour tissue (loss of one copy of chromosome 3). Monosomy 3 might lead to greater anxiety, depression, and poorer QoL. The one study that examined this found no associations between prognosis and psychological well-being, but is inconclusive because the sample size was small (N=99) and the design cross-sectional.14 Therefore, our third aim was to examine whether anxiety, depression, and QoL differed over time according to: patients’ age and gender; whether or not they had been treated by enucleation; and whether they had monosomy 3.
Materials and methods
Participants
The study sample comprised a consecutive series of adult patients living in England and Wales who were treated for uveal melanoma (choroid and ciliary body) from April 1st 2008 to December 31st 2011 at the Liverpool Ocular Oncology Centre (LOOC).
Melanomas were diagnosed according to generally-accepted clinical signs.15 If these were inconclusive, the diagnosis was established by documenting growth or by biopsy.16 Treatment choice was decided based on tumour size and clinical features taking into account patients’ preferences and wishes.17 The first choice of treatment was ruthenium plaque radiotherapy. Proton beam radiotherapy was preferred for posterior uveal melanomas that were unsuitable for plaque radiotherapy because of size or location. Trans-scleral local resection was performed if large tumour size and/or extensive retinal detachment indicated a high risk of neovascular glaucoma (‘toxic tumour syndrome’) after radiotherapy. Endoresection was selected if it offered the only chance of conserving useful vision and if the patient accepted the controversial nature of the procedure. Enucleation was considered if the risk profile of other treatment modalities was thought unfavourable or on the patient’s request.
Patient information and consent procedures are fully explained elsewhere.17 After diagnosis of uveal melanoma, patients’ conditions were explained to them alongside the potential benefits and iatrogenic effects of differing therapies. Patients were encouraged to be involved in treatment decisions. Patients were then informed about the possibility of survival prognostication and asked to decide whether they would like this information. Prognostication was based on clinical stage, histologic grade of malignancy and genetic indicators of lethality (ie, monosomy 3). Patients who underwent successful genetic analysis of tumour tissue were provided with a 10-year risk profile.18 For patients where genetic analysis failed prognosis was based on the clinical features of the tumour. Following discussion about their prognosis, patients were referred to a medical oncologist for screening for metastases if the risk of metastatic death was considered significant (ie, exceeding 20% at 10 years). Patients at low risk were told that they had a near normal life expectancy for their age and gender. All patients regardless of treatment and prognosis had access to specialist ocular oncology nurses and were offered psychological support from a health psychologist.
Enucleated patients had a clinical review 1 month post-operatively. Patients who underwent eye-conserving treatment were reviewed 1 month post-operatively, then every 6 months for 5 years, then annually. Assessments generally alternated between our centre and the referring hospital until the risk of local tumour recurrence was considered to be <1%, when the patient was discharged from our centre.
Data collected
This audit was approved by the Liverpool Research Ethics Committee (03/06/072/A) and was conducted in accordance with the Declaration of Helsinki. All patients who consented to participate were sent by mail the PROMs self-report questionnaire (see below) 6 months following treatment, then annually on the anniversary of their treatment thereafter. Here, we report data to 2 years. No questionnaires were sent before the first data collection point at 6 months. Anxiety and depression were assessed using the Hospital Anxiety & Depression Scale (HADS),19 higher scores indicating greater distress. QoL was measured using the total score from the Functional Assessment of Cancer Therapy scale (FACT-G),20, 21 higher scores indicating better QoL. To characterize the sample, we noted clinical and demographic variables from clinical records: gender; age (categorized in two groups by median split); marital status; employment status; eye laterality; treatment modality (eye conserved vs enucleation); and visual acuity in the fellow eye at diagnosis. The presence or absence of monosomy 3 is determined from genetic analysis of material from tumour biopsy. Biopsy outcomes are: monosomy 3 (high likelihood of death from metastatic disease); disomy 3 (low likelihood of metastatic death); and an inconclusive result whereby prognosis cannot be accurately determined. Some patients may decline a biopsy, or a biopsy may not be possible. For the present study, we compared those with confirmed monosomy 3 to those in whom it was not confirmed (combining those with disomy 3 or an inconclusive result and those who did not undergo successful biopsy).
Statistical analysis
The possibility of bias in sample attrition over time was assessed by comparing patients retained in the study at the final (2-year) measurement point to those who provided 6-month data but were lost to follow-up. Using chi-squared tests and t-tests, we compared these groups on socio-demographic variables (age group (median split at age 64), sex, marital status, employment status) clinical variables (eye laterality, enucleation vs eye conserved, visual acuity in the fellow eye at diagnosis and monosomy 3), and 6-month HADS and FACT-G scores.
To compare mean scores for anxiety, depression, and QoL at each time point to published normative values using 2-sample t-tests, we obtained normative data that were as comprehensive as possible. We selected studies reporting on large community samples in the previous 15 years in countries culturally similar to the UK. For anxiety and depression, normative values were available from community samples in Germany: N=4410,22 Sweden: N=624,23 and two data sets from the Netherlands: Ns=199 and 5194 24 (relevant UK data were not available). For FACT-G, normative values were available from community samples in the USA: N=1075,25 Australia: N=2719 26 and Austria: N=926 27 (relevant UK data were not available). Where available, data were compared separately for males and females.
To determine if outcomes were associated with gender, age group (categorized by median split), whether the patient was enucleated or not and whether monosomy 3 was detected or not, we used 2 × 3 mixed-model analyses of variance. Separate analyses were performed for anxiety, depression and QoL outcomes, and for each independent variable (gender, age group, enucleation, and monosomy 3). For all analyses, the repeated-measures factor was the score at the 6-months, 1-year, and 2-year assessments. Only participants who had contributed data at all time points were included in these analyses. Visual acuity in the fellow eye influences visual function if vision in the affected eye is reduced or lost.12 Thus, we assessed fellow eye acuity using Snellen scores and converted these to the logarithm of the minimum angle of resolution (logMAR).28 All analyses were initially conducted using logMAR scores (fellow eye) as covariates. Although logMAR scores were associated with depression at times 1 (r=0.16, P<0.01) and 2 (r=0.17, P<0.01) and FACT-G at time 1 (r=−0.14, P<0.01), they did not affect the outcomes of analyses when used as covariates. For simplicity, the analyses are presented without logMAR as a covariate.
Results
Sample characteristics
Of 716 patients who were treated at LOOC for uveal melanoma (choroid and ciliary body) during the study period, 554 (77%) consented to participate, of whom 411 of 554 (74.2%) patients provided data at 6 months. Their socio-demographic and clinical characteristics are summarised in Table 1. Median age at the time of treatment was 64 years (range: 23–94). Of 39 (9.3%) who died over the 2 year period, 13/411 (3.2%) had died by year 1 and a further 26/411 died (3%) by year 2. Of the remaining patients, 325/398 (81.7%) and 291/372 (78.2%) provided data at 1 and 2 years, respectively.
Attrition analysis
Patients who were retained at 2 years did not differ from those who were not retained on pre-treatment socio-demographic or clinical characteristics. Patients with monosomy 3 were less likely to be retained than others (85/134 (63.4%) vs 203/277 (73.3%), χ2 4.18, df 1, P<0.51) but this did not achieve significance. Of the 49 patients with monosomy 3 not retained at follow-up, 26 were known to have died. Another predictor of sample retention that approached but did not achieve significance was ocular conservation: patients whose eye was conserved were more likely to be retained than were those who were enucleated (215/295 (72.9%) vs 73/116 (62.9%), χ2 3.93, df 1, P=0.56). The 6-month psychological characteristics (anxiety, depression, QoL) of patients who provided data at 2 years did not differ from those who did not.
Comparison with normative values
Mean values of mood and QoL are shown in Tables 2 and 3, where they are compared with normative values. Anxiety (Table 2) was higher in our female patients compared with female patients in Hinz and Brähler22 at 6 months and 1 year, and in Lisspers et al23 at all three times points. Anxiety in males did not differ from the normative values.
Depression (Table 2) was generally lower in our sample than normative values. Males in our cohort were less depressed throughout the follow-up period than those in Hinz and Brähler22 and Lisspers et al.23 Females, although significantly less depressed throughout the follow-up period than those in Hinz’s sample,22 did not differ from females in Lisspers’ sample23 at any time.
In general, QoL (Table 3) was better in our cohort than the normative values. Males in our cohort had better QoL at all three time points than males in two studies (Cella25 and Janda et al26) and those at 6 months had better QoL than males in the third (Holzner et al27). Females had better QoL at all 3 time points compared with Cella25 and those at 2 years had better QoL than females in Janda et al26 and Holzner et al.27
Effects of age group, gender, enucleation, and monosomy 3
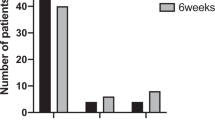
Table 4 shows anxiety, depression, and QoL at each time point according to age group, gender, enucleation, and monosomy 3. Only analyses involving gender, age group, and monosomy 3 showed significant effects. A significant main effect of gender showed that females were more anxious than males overall (F=13.21, df 1259, P<0.01). A significant main effect of age group showed that younger patients were more anxious than older patients overall (F=19.75, df 1259, P<0.01). However, there was also a significant interaction of age group with time (F=4.89, df 1259, P<0.01). Simple effects analysis showed that anxiety decreased over time in younger patients (F=6.23, df 2131, P<0.01) whereas in older patients it did not change (F=0.76, df 2126, P=0.46). There were no differences in outcomes at any point depending on whether patients were enucleated or not. Monosomy 3 patients were more depressed than others at each time point (F=6.75, df 1259, P<0.05).
Discussion
The most striking finding was that generally, regardless of age and gender, and regardless of whether or not treatment conserved the eye, these patients had similar or better QoL and less depression compared with general population normative values. This finding was present by 6 months and persisted through the 2-year follow-up period. For anxiety, the findings were less consistent, with some evidence that female patients were more anxious than general population normative values early in the follow-up period. Females and younger patients were more anxious overall, but their mean scores were substantially below the HADS cut-off score of 8 that indicates probable clinically-relevant anxiety. Enucleated patients had similar outcomes to those whose eye was conserved. Patients with monosomy 3 had more depressed mood at all time points, although their mean scores were substantially below the HADS cut-off score for probable clinically-relevant depression.29
Although it may seem surprising that patients treated for uveal melanoma describe less depressed mood and better QoL than the normal population, it is well established that people in adversity, including patients with life-threatening or disabling chronic conditions, can value life more than healthy individuals.30, 31 Furthermore, there is some evidence that patients with cancer have better mood 32 and similar QoL33 compared with normal populations. The finding that females and younger patients were more vulnerable to anxiety is consistent with previous work in cancer patients generally.13 That outcomes were as good in enucleated patients as in those who did not lose the eye is consistent with two previous reports.5, 7
Major strengths of this study were its prospective design and the large sample of patients with uveal melanoma. To our knowledge, this study provides the largest prospective evaluation of PROMs in a consecutive sample of patients treated for uveal melanoma (choroid and ciliary body), regardless of tumour size and co-morbidities. Because it is not feasible to obtain information on PROMs premorbidly, we compared patients’ data with several normative samples. Our study has some limitations, however. First of all, of eligible participants, 298/716 (42%) declined to enter the study; 124/716 (17%) were not retained at 2-year follow-up. The disproportionately high loss of monosomy 3 patients will slightly decrease depression scores at each time point. Nevertheless, those providing data at 2 years were broadly similar to those who withdrew on key clinical and socio-demographic characteristics, and all initial PROMs measures at 6 months. Moreover, retention is within the range of previous studies (40–93%; 5, 6, 7, 8, 9, 10, 12). Second, we did not make an assessment of mood disturbance or QoL before treatment because we did not wish to burden patients during this period of acute distress. Not doing so means that we cannot assess changes from pre-treatment to the six-month follow-up. Finally, the findings are from a single study centre. Other centres could use a similar design to test the generalizability of these findings.
Overall, our findings indicate a positive picture: that uveal melanoma patients are largely able to respond to challenges to their well-being associated with the disease and its treatment. It is worth mentioning that patients were advised against eye-conserving therapy if significant ocular morbidity was anticipated. Furthermore, enucleation was performed according to strict protocols that minimized post-operative pain and optimized the chances of a satisfactory cosmetic appearance. Importantly, special measures were taken to counsel patients at the time of treatment selection, to ensure that consent was truly informed (ie, patients received audio-recordings of consultations, printed information sheets, and counselling by specialist ocular oncology nurses). Finally, patients were routinely offered an assessment with a health psychologist during the peri-operative period so that psychological support could be provided to distressed individuals who sought it. If all these measures are taken, clinicians can reassure patients that they can expect to have as good a QoL as the normal population. However, there is some evidence of elevated anxiety in younger and female patients and of more depressed mood in patients with monosomy 3, and interventions to help patients tolerate the uncertainty associated with this disease are needed. Further, generally positive group data should not obscure the plight of individual patients who struggle. Clinicians need to be alert to the possibility that younger and female patients and those with monosomy 3 may experience poorer mood.

References
Singh AD, Turell ME, Topham AK . Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology 2011; 118: 1881–1885.
Kujala E, Mäkitie T, Kivelä T . Very long-term prognosis of patients with malignant uveal melanoma. Invest Ophthalmol Vis Sci 2003; 44: 4651–4659.
Augsburger JJ, Corrêa ZM, Shaikh AH . Effectiveness of treatments for metastatic uveal melanoma. Am J Ophthalmol 2009; 148: 119–127.
Hope-Stone L, Brown SL, Heimann H, Damato B, Salmon P . How do patients with uveal melanoma experience and manage uncertainty? A qualitative study. Psycho-Oncology 2015; 24: 1485–1491.
Brandberg Y, Kock E, Oskar K, Trampe E, Seregard S . Psychological reactions and quality of life in patients with posterior uveal melanoma treated with ruthenium plaque therapy or enucleation: a one year follow-up study. Eye 2000; 14: 839–846.
Chabert S, Velikay-Parel M, Zehetmayer M . Influence of uveal melanoma therapy on patients’ quality of life: a psychological study. Acta Ophthalmol Scand 2004; 82: 25–31.
Collaborative Ocular Melanoma Study-Quality of Life Study Group. Quality of Life after iodine 125 brachytherapy vs enucleation for choroidal melanoma: 5-year results from the collaborative ocular melanoma study: COMS QOLS report no. 3. Arch Ophthalmol 2006; 124: 226–238.
Cruickshanks KJ, Fryback DG, Nondahl DM, Robinson N, Keesey U, Dalton DS et al. Treatment choice and quality of life in patients with choroidal melanoma. Arch Ophthalmol 1999; 117: 461–467.
Reimer J, Esser J, Fleiss A, Hessel A, Anastassiou G, Krausz M et al. Quality of life in patients with malignant choroidal melanoma after radiotherapy. Graefes Arch Clin Exp Ophthalmol 2003; 241: 371–377.
Reimer J, Voigtlaender-Fleiss A, Karow A, Bornfeld N, Esser J, Helga Franke G . The impact of diagnosis and plaque radiotherapy treatment of malignant choroidal melanoma on patients’ quality of life. Psycho-Oncology 2006; 15: 1077–1085.
Amaro TAC, Yazigi L, Erwenne C . Depression and quality of life during treatment of ocular bulb removal in individuals with uveal melanoma. Eur J Cancer Care (Engl) 2010; 19: 476–481.
Wiley JF, Laird K, Beran T, McCannel TA, Stanton AL . Quality of life and cancer-related needs in patients with choroidal melanoma. Br J Ophthalmol 2013; 97: 1471–1474.
Linden W, Vodermaier A, MacKenzie R, Grieg D . Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender and age. J Affect Disorders 2012; 141: 343–351.
Beran TM, McCannel TA, Stanton AL, Straatsma BR, Burgess BL . Reactions to and desire for prognostic testing in choroidal melanoma patients. J Genet Couns 2009; 18: 265–274.
Sheilds CL, Shields JA, Singh AD, Santos MC, Carvalho C . Combination of clinical factors predictive of growth of small choroidal melanocytic tumors. Arch Ophthalmol 2000; 118: 360–364.
Sen J, Groenewald C, Hiscott PS, Smith PA, Damato BE . Transretinal choroidal tumor biopsy with 25-gauge vitrector. Ophthalmology 2006; 113: 1028–1031.
Damato B, Heimann H . Personalized treatment of uveal melanoma. Eye 2013; 27: 172–179.
Damato B, Eleuteri A, Taktak AFG, Coupland SE . Estimating prognosis for survival after treatment of choroidal melanoma. Prog Retin Eye Res 2011; 30: 285–295.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol 1993; 11: 570–579.
Webster K, Yost K . The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications and interpretations. Health Qual Life Outcomes 2003; 1: 79–86.
Hinz A, Brähler E . Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J Psychosom Res 2011; 71: 74–78.
Lisspers J, Nygren A, Soderman E . Hospital anxiety and depression scale (HAD): some psychometric data for a Swedish sample. Acta Psychiatr Scand 1997; 96: 281–286.
Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM . A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychol Med 1997; 27: 363–370.
Cella DF . Manual of the Functional Assessment of Chronic Illness Therapy (FACIT Scales) (Version 4.1). Center on Outcomes Research and Education, North Western Health Care: Evanston, IL, 2004.
Janda M, DiSipio T, Hurst C, Cella DF, Newman B . The Queensland cancer risk study: general population norms for the functional assessment of cancer therapy-general (FACT-G). Psycho-Oncology 2009; 18: 606–614.
Holzner B, Kemmler G, Cella DF, De Paoli C, Meraner V, Kopp M et al. Normative data for functional assessment of cancer therapy—general scale and its use for the interpretation of quality of life scores in cancer survivors. Acta Oncol 2004; 43: 153–160.
Holladay JT . Visual acuity measurements. J Cataract Refract Surg 2004; 30: 287–290.
Vodermaier A, Millman R . Accuracy of the hospital anxiety and depression scale as a screening tool in cancer patients: a systematic review and meta-analysis. Support Care Cancer 2011; 19: 1899–1908.
Affleck G, Tennen H . Construing benefits from adversity: adaptional significance and dispositional underpinnings. J Pers 1996; 64: 899–922.
Helgeson VS, Reynolds KA, Tomich PL . A meta-analytic review of benefit finding and growth. J Consult Clin Psychol 2006; 74: 797–816.
Osbourne R, Elsworth GR, Sprangers MAG, Ort FJ, Hopper JL . The value of the hospital anxiety and depression scale (HADS) for comparing women with early onset breast cancer with population-based reference women. Qual Life Res 2004; 13: 191–206.
Herce Lopez J, Rollon Mayordomo A, Lozano Rosado R, Salazar Fernandez CI, Gallana S . Quality of life in long-term oral cancer survivors: a comparison with Spanish general population norms. J Oral Maxillofac Surg 2009; 67: 1607–1614.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hope-Stone, L., Brown, S., Heimann, H. et al. Two-year patient-reported outcomes following treatment of uveal melanoma. Eye 30, 1598–1605 (2016). https://doi.org/10.1038/eye.2016.188
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.188
This article is cited by
-
Quality of life among people with eye cancer: a systematic review from 2012 to 2022
Health and Quality of Life Outcomes (2024)
-
Cooperative phototherapy based on bimodal imaging guidance for the treatment of uveal melanoma
Journal of Nanobiotechnology (2023)
-
Predictors of emotional distress in uveal melanoma survivors: a systematic review
Eye (2023)
-
Fear of prognosis? How anxiety, coping, and expected burden impact the decision to have cytogenetic assessment in uveal melanoma patients
Supportive Care in Cancer (2022)
-
Quality of life and treatment-related burden during ocular proton therapy: a prospective trial of 131 patients with uveal melanoma
Radiation Oncology (2021)