Abstract
When aiming to provide more expedited cancer diagnosis and treatment of cancer at an earlier stage, it is important to take into account the symptom epidemiology throughout the pathway, from first bodily sensation until the start of cancer treatment. This has implications for how primary-care providers interpret the presentation and decisions around patient management and investigation. Symptom epidemiology has consequences for how the health-care system might best be organised. This paper argues for and describes the organisation of the Danish three-legged strategy in diagnosing cancer, which includes urgent referral pathways for symptoms suspicious of a specific cancer, urgent referral to diagnostic centres when we need quick and profound evaluation of patients with nonspecific, serious symptoms and finally easy and fast access to ‘No-Yes-Clinics’ for cancer investigations for those patients with common symptoms in whom the diagnosis of cancer should not be missed. The organisation of the health-care system must reflect the reality of symptoms presented in primary care. The organisational change is evaluated and monitored with a comprehensive research agenda, data infrastructure and education.
Similar content being viewed by others
Main
In recent years, many health-care systems have implemented specific strategies to ensure timely cancer diagnosis (Department of Health, 2000; Prades et al, 2011). This has been motivated by poor cancer control, public discontent with long waiting times and an organisational and economic attempt for efficiency in standardised diagnostic pathways (Richards, 2009). Reports have shown that cancer survival in the United Kingdom and Denmark is lower than that in other countries (Storm et al, 2010; Coleman et al, 2011). Danish cancer patients are treated at later stages (Maringe et al, 2012; Walters et al, 2013a, 2013b), suggesting delays in presentation, diagnosis and treatment. This is supported by the evidence that waiting times can be long in the Danish cancer care system, which may lead to higher mortality (Tørring et al, 2011, 2012, 2013; Elit et al, 2014; Redaniel et al, 2014; Neal et al, 2015) and stage progression (Jensen et al, 2007; Wang et al, 2012).
In 2008, after several years of investment in cancer treatment and two cancer plans, Denmark introduced urgent referral for suspected cancer (Olesen et al, 2009). Politically, cancer was proclaimed an acute disease for which diagnosis and treatment should be without waiting time (Probst et al, 2012). Such urgent referral pathways are in place in a number of health-care systems and are being developed in others. Based on the defined alarm symptoms, the GP can suspect cancer and refer urgently to a specific pathway, and the speed and logistics of the diagnostic pathway and the standardisation of treatment within the hospital setting can be improved (Toustrup et al, 2011; Vallverdú-Cartié et al, 2011; Valentín-López et al, 2012; Dyrop et al, 2013; Larsen et al, 2013).
In the process that followed the introduction of the urgent referral pathway in Denmark, it became obvious that this pathway was inadequate to ensure timely diagnosis of all cancer patients, and a strategy based on three cornerstones was developed.
This paper argues for and describes the three-legged strategy for cancer diagnosis in Denmark, where the purpose is to accommodate the fact that patients with an early-stage cancer present very differently in general practice and that a single focus on alarm symptoms or red flags might not be sufficient.
Reasons for longer diagnostic pathways
If cancer patients are asked, after treatment completion, what they consider the most important part of the pathway, they report aspects of expedited referral, diagnosis and treatment and short waiting time for all investigations, including the very first ones often prescribed by the GP (Booji et al, 2013). This is also indicated by the finding that Danish cancer patients’ confidence in their GPs decreases with increasing time to diagnosis (Larsen et al, 2011).
A study among Danish GPs in 2010, after the introduction of urgent referral for suspected cancer, asked about their cancer patients, diagnostic pathways, and showed that in about one-third of cases, the GPs reported a quality deviation which was strongly associated with longer diagnostic intervals (Jensen et al, 2014).
There is also evidence that the organisation of the health-care system may have adverse effects. In an ecological study in which we compared a number of European countries’ primary care and their 1-year cancer survival rates, we saw that countries with a strong gatekeeper role also had the lowest cancer survival rates (Vedsted and Olesen, 2011). This could suggest that in some countries where GPs were good gatekeepers, the GPs had become too reluctant to refer early to diagnostic investigations. Further, that access to diagnostic services in the initial phase was slow or rationed, resulting in patients not obtaining timely cancer investigations.
Symptom epidemiology and the ‘diagnostic funnel’
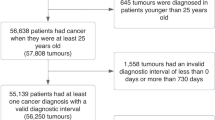
Another aspect is that health-care systems should be organised to support the diagnostic needs. In cancer diagnosis, the processes related to symptom epidemiology must be recalled (Figure 1; Elliott et al, 2011). In line with this, studies have demonstrated the 'symptom iceberg', showing that >15% of adults will have experienced at least one cancer alarm symptom during the last year (Svendsen et al, 2010). Only a small proportion of these will seek help, for example 10% of those with rectal bleeding consult their GP (McAvoy, 2007).
Despite relevant screening activities, ∼85–90% of all cancers are diagnosed on the basis of symptomatic presentation (Hansen et al, 2011; Vedsted and Olesen, 2009; Emery et al, 2014). In health-care systems in which GPs form a specialised first line, data show that 75–85% of all cancer patients start in general practice by presenting signs or symptoms (Allgar and Neal, 2005).
It has been shown that the GP indicates potential alarm symptoms in up to 12% (Ingebrigsten et al, 2013) of all consultations and suspect a serious disease in need of further elucidation in 6% of consultations (Hjertholm et al, 2014) (Figure 1). A study showed that 10% of these patients had a new serious diagnosis within 2 months. This means that when the GP suspects serious illness there are reasons to support the GP in having access to relevant investigations (Nylenna, 1986).
The symptom continuum
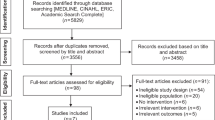
Another important aspect is that, once a symptom is presented in general practice, the severity of a symptom could be thought of as forming a continuum. An example of this continuum could be abdominal pain. In the clinical context, abdominal pain should be understood in terms of the continuum with increasing clinical significance, thus becoming more and more indicative of a serious disease (cancer). In the clinical cancer diagnosis, a symptom does not present as ‘there’ or ‘not there’. Symptoms appear from ‘certainly not serious’ to ‘definitely serious’ (Figure 2).
The first section (left) of the symptom continuum is that in which the symptom presents as harmless. The second section is where the symptom is most probably not a sign of cancer, although cancer cannot be excluded. This is the so-called ‘low-risk-but-not-no-risk’ symptom (Hamilton, 2010). The third section is where the symptom definitely indicates risk of a serious disease and an urgent referral is relevant. Fortunately, in general practice it is rarely cancer, even if it is an alarm symptom (Hamilton, 2009a). However, it is still the GP’s duty to identify the cancer over the whole symptom continuum. Progression along the symptom continuum might, for example, be the reason that we can observe that patients who are later diagnosed with cancer tend to see their GP several months before diagnosis (Christensen et al, 2012; Ahrensberg et al, 2013). Here the GPs may have used time as a diagnostic test (Almond and Summerton, 2009). However, waiting until the symptom becomes definitely serious might also imply a stage progression in some cancers.
The ‘obvious’, ‘difficult’ and ‘common’ cancer presentations
A study in Danish general practice has revealed that, if GPs are allowed simply to categorise the first presentation of cancer, 50% are categorised as alarm symptoms, 20% are serious, but cancer nonspecific symptoms and 30% are categorised as normal vague symptoms (Jensen et al, 2014). This has also been supported by the finding that 50% of cancer patients in United Kingdom general practice did not have a National Institute for Health and Care Excellence guideline symptom suspicious for cancer registered in the patient record (Neal et al, 2014). Thus, some cancer patients do present in general practice, but not with symptoms indicative of cancer.
The three-legged diagnostic strategy
A wish for expedited cancer diagnosis and cancer diagnosis at an earlier stage necessitates that we broaden the focus on alarm symptoms to include the full symptom continuum. A system that focusses on cancer diagnosis based on alarm symptoms alone might also be a health-care system that favours ‘the sick-quick’ and lets down the majority with vague symptoms (Hamilton, 2009a). A Danish study illustrated this by showing that, if the GP regards the symptom as vague, 50% of cancer patients will wait at least one month more and 25% at least 2.5 months longer until diagnosis, compared with those with alarm symptoms (Jensen et al, 2014). Thus, urgent referral for the obvious alarm symptoms must be accompanied by two more referral routes; the urgent referral for nonspecific, serious symptoms and the no-yes-clinics (NYC).
This led to the development of the three-legged cancer diagnosis strategy in Denmark (Figure 3). It acknowledges that we need diagnostic routes for what the GPs recognise as alarm symptoms (the obvious cancer suspicion), the nonspecific symptoms (the difficult diagnosis) and the vague symptoms (the common symptom).
The urgent referral pathway
From UK-based practice research, it is known that the risk of having cancer given a single alarm symptom is often in the range of 3–8% (Jones et al, 2007; Hamilton, 2009b; Shapley et al, 2010). Meechan and colleagues (2012) showed that, among those referred to the urgent referral pathway, the risk of cancer was 11%. Thus, the urgent referral strategy seems to be effective. However, what is also shown – and forms the platform for introducing further diagnostic possibilities – is that on average only 40–45% (with differences between cancer types) of all cancer patients are primarily referred to specific pathways (Meechan et al, 2012; Jensen et al, 2014). This means that the largest group of cancer patients is not offered this faster and perhaps most appropriate route to diagnosis (Elliss-Brookes et al, 2012; Guldbrandt et al, 2015).
Urgent referral for unspecific, serious symptoms and the diagnostic centres
The urgent referral for unspecific, serious symptoms was implemented nationally by the National Board of Health and Danish Regions in 2012. When a GP has a patient that is clearly sick, and where cancer is one of several diagnostic possibilities, they can be referred. The pathway consists of a two-step approach with a filter function performed by the GP and, if still relevant, a referral to a diagnostic centre. The filter function is a standard battery of diagnostic investigations consisting of blood and urine tests and diagnostic imaging. The results of the investigations are sent electronically to the GP within four working days. The GP subsequently decides further diagnostic steps within eight working days. If there is no explanation for the symptoms the GP can refer to the diagnostic centre and no longer has the diagnostic responsibility for the patient.
A diagnostic centre is a medical unit with comprehensive facilities for medical investigation, including easy access to expertise in a wide range of relevant specialities. Patients are appointed a responsible doctor for the outpatient trajectory.
Each of the five Danish regions must have at least one diagnostic centre, and ∼15 centres have now been established. The symptoms most often seen at referral are weight loss, fatigue, unspecific pain and nausea. ‘Problems with general health’ and ‘GP’s gut feeling’ are among the most likely clinical signs for referral to a diagnostic centre. The proportion with cancer among those referred is ∼15–20%. The cancers most often seen are lung, colorectal and haematological cancers. There are ongoing publications of these specific results.
The NYC
For the 30–40% of cancer patients with vague, ‘low-risk-but-not-no-risk’, symptoms, Denmark now, by a governmental regulation, implements the ‘NYC’. These are services conducted in hospitals or specialist clinics. The GP has direct access to fast investigations as part of the classical iterative diagnostic process (Norman et al, 2009) where the GP can raise a possibility of cancer – the serious diagnosis that the GP does not want to fail to spot.
The principle is to keep it simple; the GP is responsible for the diagnostic actions and the patient is not admitted to the hospital, thus avoiding use of resources, for example, history taking, blood tests, patient records and other administrative or clinical resources demanding activity. Studies indicate that the strategy can be both effective and efficient. A Dutch study of direct access to colonoscopy for abdominal symptoms showed reduced time to diagnosis and more efficient use of tests (Klemann et al, 2011). This is supported by studies from the United Kingdom (Maruthachalam et al, 2005; Ahmed et al, 2013). A randomised Danish study giving GPs direct access to a low-dose CT scan for suspected lung cancer showed that the use of CT scans did not increase, compared with the usual ‘double gatekeeping’ by the lung specialist (Guldbrandt et al, 2013).
There are ongoing studies on the specific ways of organising this, which patients to refer and what investigations should be provided.
Conclusion and perspectives
When aiming to provide more expedited cancer diagnosis and treatment of cancer at an earlier stage, it is important to take into account the symptom epidemiology throughout the pathway, from the first bodily sensation until the start of cancer treatment. This has implications for how primary care providers interpret the presentation and decisions around patient management and investigation. Symptom epidemiology has consequences for how the health-care system might best be organised.
This paper provides several reasons to support and test a three-legged strategy, in particular for diagnosing cancer in earlier stages. The GPs need diagnostic routes that, first, take into account the fact that symptoms present on a continuum from ‘certainly not serious’ to ‘definitely serious’ and, second, that cancers present with symptoms that sometimes obviously indicate cancer but for the majority are nonspecific and serious or vague and common. Since our previous paper in 2009 about the Danish example (Olesen et al, 2009), the focus in Denmark has been to develop broad support for the GPs’ different tasks in diagnosing cancer. The continuous growing evidence on cancer diagnosis is implemented into daily clinical practice and health policy to ensure structural support. Thus, it should be remembered that in a modern health-care system the best pathways from symptom to cancer treatment are established only if there is a culture of responsibility – making these changes requires political, administrative and clinical leadership.
To improve and optimise this differentiated approach we call for a large research agenda and precise evidence-based implementation strategies. The effectiveness and efficiency of the diagnostic centres and the NYC need further research and monitoring, and the Danish government and regions are engaged in this work. Intervention studies are needed to test whether there is an effect on stage distribution and survival, quality of life, health economics and patient evaluation. There is a need for more clinical research, including research into primary care and specialised diagnostic investigations. Finally, we must also ensure practical implementation by education (Guldbrandt et al, 2014) and facilities for primary diagnosis (Toftegaard et al, 2014).
References
Ahmed J, Mehmood S, Khan SA, Rao MM (2013) Direct access colonoscopy in primary care: is it a safe and practical approach? Scott Med J 58: 168–172.
Ahrensberg JM, Fenger-Grøn M, Vedsted P (2013) Use of primary care during the year before childhood cancer diagnosis: a nationwide population-based matched comparative study. PLoS One 8 (3): e59098.
Allgar VL, Neal RD (2005) Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients. Br J Cancer 92: 1959–1970.
Almond SC, Summerton N (2009) Test of time. BMJ 338: b1878.
Booij JC, Zegers M, Evers PM, Hendriks M, Delnoij DM, Rademakers JJ (2013) Improving cancer patient care: development of a generic cancer consumer quality index questionnaire for cancer patients. BMC Cancer 13: 203.
Christensen KG, Fenger-Grøn M, Flarup KR, Vedsted P (2012) Use of general practice, diagnostic investigations and hospital services before and after cancer diagnosis—a population-based nationwide registry study of 127,000 incident adult cancer patients. BMC Health Serv Res 12: 224.
Coleman MP, Forman D, Bryant H, Butler J, Rachet B, Maringe C, Nur U, Tracey E, Coory M, Hatcher J, McGahan CE, Turner D, Marrett L, Gjerstorff ML, Johannesen TB, Adolfsson J, Lambe M, Lawrence G, Meechan D, Morris EJ, Middleton R, Steward J, Richards MA ICBP Module 1 Working Group (2011) Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995-2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 377: 127–138.
Department of Health (2000) The NHS Cancer Plan. A Plan for Investment, a plan for reform. Department of Health: London, UK.
Dyrop HB, Safwat A, Vedsted P, Maretty-Nielsen K, Hansen BH, Jørgensen PH, Baad-Hansen T, Bünger C, Keller J (2013) Cancer Patient Pathways shortens waiting times and accelerates the diagnostic process of suspected sarcoma patients in Denmark. Health Policy 113: 110–117.
Elit LM, O'Leary EM, Pond GR, Seow HY (2014) Impact of wait times on survival for women with uterine cancer. J Clin Oncol 32: 27–33.
Elliott AM, McAteer A, Hannaford PC (2011) Revisiting the symptom iceberg in today's primary care: results from a UK population survey. BMC Fam Pract 12: 16.
Elliss-Brookes L, McPhail S, Ives A, Greenslade M, Shelton J, Hiom S, Richards M (2012) Routes to diagnosis for cancer—determining the patient journey using multiple routine data sets. Br J Cancer 107: 1220–1226.
Emery JD, Shaw K, Williams B, Mazza D, Fallon-Ferguson J, Varlow M, Trevena LJ (2014) The role of primary care in early detection and follow-up of cancer. Nat Rev Clin Oncol 11: 38–48.
Guldbrandt LM, Fenger-Grøn M, Folkersen BH, Rasmussen TR, Vedsted P (2013) Reduced specialist time with direct computed tomography for suspected lung cancer in primary care. Dan Med J 60: A4738.
Guldbrandt L, Fenger-Grøn M, Rasmussen T, Jensen H (2015) The role of general practice in routes to diagnosis of lung cancer in Denmark: a population-based study of general practice involvement, diagnostic activity and diagnostic intervals. BMC Health Serv Res 22, 15(1): 21.
Guldbrandt LM, Rasmussen TR, Rasmussen F, Vedsted P (2014) Implementing direct access to low-dose computed tomography in general practice-method, adaption and outcome. PLoS One 9: e112162.
Hamilton W (2009a) Five misconceptions in cancer diagnosis. Br J Gen Pract 59: 441–445.
Hamilton W (2009b) The CAPER studies: five case-control studies aimed at identifying and quantifying the risk of cancer in symptomatic primary care patients. Br J Cancer 101: S80–S86.
Hamilton W (2010) Cancer diagnosis in primary care. Br J Gen Pract 60: 121–128.
Hansen R, Vedsted P, Sokolowski I, Søndergaard J, Olesen F (2011) Time intervals from first symptom to treatment of cancer: a cohort study of 2,212 newly diagnosed cancer patients. BMC Health Serv Res 11: 284.
Hjertholm P, Moth G, Ingeman ML, Vedsted P (2014) Predictive values of GPs' suspicion of serious disease: a population-based follow-up study. Br J Gen Pract 64: 346–353.
Ingebrigtsen SG, Scheel BI, Hart B, Thorsen T, Holtedahl K (2013) Frequency of 'warning signs of cancer' in Norwegian general practice, with prospective recording of subsequent cancer. Fam Pract 30: 153–160.
Jensen AR, Nellemann HM, Overgaard J (2007) Tumor progression in waiting time for radiotherapy in head and neck cancer. Radiother Oncol 84: 5–10.
Jensen H, Nissen A, Vedsted P (2014) Quality deviations in cancer diagnosis: prevalence and time to diagnosis in general practice. Br J Gen Pract 64: e92–e98.
Jensen H, Tørring ML, Olesen F, Overgaard J, Vedsted P (2014) Cancer suspicion in general practice, urgent referral and time to diagnosis: a population-based GP survey and registry study. BMC Cancer 14: 636.
Jones R, Latinovic R, Charlton J, Gulliford MC (2007) Alarm symptoms in early diagnosis of cancer in primary care: cohort study using General Practice Research Database. BMJ 334: 1040.
Klemann VM, Wolters FL, Konsten JL (2011) Benefits of a well-structured diagnostic process in colon cancer. Dig Surg 28: 15–21.
Larsen MB, Hansen RP, Hansen DG, Olesen F, Vedsted P (2013) Secondary care intervals before and after the introduction of urgent referral guidelines for suspected cancer in Denmark: a comparative before-after study. BMC Health Serv Res 13: 348.
Larsen MB, Hansen RP, Olesen F, Vedsted P (2011) Patients' confidence in their GP before and after being diagnosed with cancer. Br J Gen Pract. 61: e215–e222.
Maringe C, Walters S, Butler J, Coleman MP, Hacker N, Hanna L, Mosgaard BJ, Nordin A, Rosen B, Engholm G, Gjerstorff ML, Hatcher J, Johannesen TB, McGahan CE, Meechan D, Middleton R, Tracey E, Turner D, Richards MA, Rachet B ICBP Module 1 Working Group (2012) Stage at diagnosis and ovarian cancer survival: Evidence from the International Cancer Benchmarking Partnership. Gynecol Oncol 127: 75–82.
Maruthachalam K, Stoker E, Chaudhri S, Noblett S, Horgan AF (2005) Evolution of the two-week rule pathway—direct access colonoscopy vs outpatient appointments: one year's experience and patient satisfaction survey. Colorectal Dis 7: 480–485.
McAvoy B (2007) General practitioners and cancer control. Med J Aust 187: 115–117.
Meechan D, Gildea C, Hollingworth L, Richards MA, Riley D, Rubin G (2012) Variation in use of the 2-week referral pathway for suspected cancer: a cross-sectional analysis. Br J Gen Pract 62: e590–e597.
Neal RD, Din NU, Hamilton W, Ukoumunne OC, Carter B, Stapley S, Rubin G (2014) Comparison of cancer diagnostic intervals before and after implementation of NICE guidelines: analysis of data from the UK General Practice Research Database. Br J Cancer 110: 584–592.
Neal RD, Tharmanathan P, France B, Din NU, Cotton S, Fallon-Ferguson J, Hamilton W, Hendry A, Hendry M, Lewis R, Macleod U, Mitchell ED, Pickett M, Rai T, Shaw K, Stuart N, Tørring ML, Wilkinson C, Williams B, Williams N, Emery J (2015) Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systemic Review. Br J Cancer 112(Suppl 1):S92–S107.
Norman G, Barraclough K, Dolovich L, Price D (2009) Iterative diagnosis. BMJ 339: b3490.
Nylenna M (1986) Diagnosing cancer in general practice: from suspicion to certainty. Br Med J (Clin Res Ed) 293: 314–317.
Olesen F, Hansen RP, Vedsted P (2009) Delay in diagnosis: the experience in Denmark. Br J Cancer 101 (Suppl 2): S5–S8.
Prades J, Espinàs JA, Font R, Argimon JM, Borràs JM (2011) Implementing a cancer fast-track programme between primary and specialised care in Catalonia (Spain): a mixed methods study. Br J Cancer 105: 753–759.
Probst HB, Hussain ZB, Andersen O (2012) Cancer patient pathways in Denmark as a joint effort between bureaucrats, health professionals and politicians—a national Danish project. Health Policy 105: 65–70.
Redaniel MT, Martin RM, Blazeby JM, Wade J, Jeffreys M (2014) The association of time between diagnosis and major resection with poorer colorectal cancer survival: a retrospective cohort study. BMC Cancer 14: 642.
Richards MA (2009) The national awareness and early diagnosis initiative in England: assembling the evidence. Br J Cancer 101 (Suppl 2): S1–S4.
Shapley M, Mansell G, Jordan JL, Jordan KP (2010) Positive predictive values of ⩾5% in primary care for cancer: systematic review. Br J Gen Pract 60: e366–e377.
Storm HH, Kejs AM, Engholm G, Tryggvadóttir L, Klint A, Bray F, Hakulinen T (2010) Trends in the overall survival of cancer patients diagnosed 1964-2003 in the Nordic countries followed up to the end of 2006: the importance of case-mix. Acta Oncol 49: 713–724.
Svendsen RP, Støvring H, Hansen BL, Kragstrup J, Søndergaard J, Jarbøl DE (2010) Prevalence of cancer alarm symptoms: a population-based cross-sectional study. Scand J Prim Health Care. 28: 132–137.
Toftegaard B, Bro F, Vedsted P (2014) A geographical cluster randomised stepped wedge study of continuing medical education and cancer diagnosis in general practice. Implement Sci 9 (1): 159.
Tørring ML, Frydenberg M, Hamilton W, Hansen RP, Lautrup MD, Vedsted P (2012) Diagnostic interval and mortality in colorectal cancer: U-shaped association demonstrated for three different datasets. J Clin Epidemiol 65: 669–678.
Tørring ML, Frydenberg M, Hansen RP, Olesen F, Hamilton W, Vedsted P (2011) Time to diagnosis and mortality in colorectal cancer: a cohort study in primary care. Br J Cancer 104: 934–940.
Tørring ML, Frydenberg M, Hansen RP, Olesen F, Vedsted P (2013) Evidence of increasing mortality with longer diagnostic intervals for five common cancers: a cohort study in primary care. Eur J Cancer 249: 2187–2198.
Toustrup K, Lambertsen K, Birke-Sørensen H, Ulhøi B, Sørensen L, Grau C (2011) Reduction in waiting time for diagnosis and treatment of head and neck cancer—a fast track study. Acta Oncol 50: 636–641.
Valentín-López B, Ferrándiz-Santos J, Blasco-Amaro JA, Morillas-Sáinz JD, Ruiz-López P (2012) Assessment of a rapid referral pathway for suspected colorectal cancer in Madrid. Fam Pract 29: 182–188.
Vallverdú-Cartié H, Comajuncosas-Camp J, Orbeal-Sáenz RA, López-Negre JL, Gris Garriga PJ, Jimeno-Fraile J, Hermoso-Bosch J, Sánchez-Pradell C, Torra-Alsina S, Urgellés-Bosch J, Parés D (2011) Results of implementation of a fast track pathway for diagnosis of colorectal cancer. Rev Esp Enferm Dig 103: 402–407.
Vedsted P, Olesen F (2009) Early diagnosis of cancer—the role of general practice. Scand J Prim Health Care 27: 193–194.
Vedsted P, Olesen F (2011) Are the serious problems in cancer survival partly rooted in gatekeeper principles? An ecologic study. Br J Gen Pract 61: e508–e512.
Walters S, Maringe C, Coleman MP, Peake MD, Butler J, Young N, Bergström S, Hanna L, Jakobsen E, Kölbeck K, Sundstrøm S, Engholm G, Gavin A, Gjerstorff ML, Hatcher J, Johannesen TB, Linklater KM, McGahan CE, Steward J, Tracey E, Turner D, Richards MA, Rachet B ICBP Module 1 Working Group (2013a) Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the United Kingdom: a population-based study, 2004-2007. Thorax 0: 1–14.
Walters S, Maringe C, Butler J, Rachet B, Barrett-Lee BJ, Boyages J, Christiansen P, Lee M, Wärnberg AC, Engholm G, Fornander T, Gjerstorff ML, Johannesen TB, Lawrence G, McGahan CE, Middleton R, Steward J, Tracey E, Turner D, Richards MA, Coleman MP the ICBP Module 1 Working Group (2013b) Breast cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK, 2000-2007: a population-based study. Br J Cancer 108: 1195–1208.
Wang J, Wang J, Mahasittiwat P, Wong KK, Quint LE, Kong FM (2012) Natural growth and disease progression of non-small cell lung cancer evaluated with 18F-fluorodeoxyglucose PET/CT. Lung Cancer 78: 51–56.
Acknowledgements
We thank our research team for making this work possible and all the people who continously inspire us. PV is funded by The Danish Cancer Society and the Novo Nordisk foundation. FO is funded through The Research Unit for General Practice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
FO is the chairman of the Danish Cancer Society (2015). PV declares no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Vedsted, P., Olesen, F. A differentiated approach to referrals from general practice to support early cancer diagnosis – the Danish three-legged strategy. Br J Cancer 112 (Suppl 1), S65–S69 (2015). https://doi.org/10.1038/bjc.2015.44
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.44
Keywords
This article is cited by
-
Associations between smoking status and involvement of personal and professional relations among individuals reporting symptoms related to a diagnosis of lung cancer: a population-based study
BMC Public Health (2022)
-
Prospective Observational Study on the Prevalence and Diagnostic Value of General Practitioners’ Gut Feelings for Cancer and Serious Diseases
Journal of General Internal Medicine (2022)
-
Symptoms and signs of colorectal cancer, with differences between proximal and distal colon cancer: a prospective cohort study of diagnostic accuracy in primary care
BMC Family Practice (2021)
-
Setting up a rapid diagnostic clinic for patients with vague symptoms of cancer: a mixed method process evaluation study
BMC Health Services Research (2021)
-
The effectiveness of the Guy’s Rapid Diagnostic Clinic (RDC) in detecting cancer and serious conditions in vague symptom patients
British Journal of Cancer (2021)