Anxiety disorders are the most common psychiatric disorders in children and adolescents and are associated with social and academic problems, school dropout, suicidal attempts, and other psychiatric illnesses at a later age (de Lijster et al., Reference de Lijster, Dieleman, Utens, Dierckx, Wierenga, Verhulst and Legerstee2018; Woodward & Fergusson, Reference Woodward and Fergusson2001). Remarkably, many children with anxiety disorders do not receive treatment (Chavira, Stein, Bailey, & Stein, Reference Chavira, Stein, Bailey and Stein2004), and 40% of children who receive treatment do not recover (James, James, Cowdrey, Soler, & Choke, Reference James, James, Cowdrey, Soler and Choke2015; Weisz et al., Reference Weisz, Kuppens, Ng, Eckshtain, Ugueto, Vaugh-Coaxum and Fordwood2017). Research has shown that children and adolescents with anxiety disorders show an attention bias (AB), that is, differential attention towards threat compared to neutral stimuli (Abend, de Voogd et al., Reference Abend, de Voogd, Salemink, Wiers, Pérez-Edgar, Fitzgerald and Bar-Haim2018; Dudeney, Sharpe, & Hunt, Reference Dudeney, Sharpe and Hunt2015). AB has been related to both the onset and maintenance of anxiety symptomatology (Waters & Craske, Reference Waters and Craske2016). A promising new treatment that has received much interest is Attention Bias Modification (ABM) for children and adolescents with anxiety disorders (Bar-Haim, Reference Bar-Haim2010). ABM focuses on directing attention away from threat and towards neutral stimuli instead. For adults with anxiety disorders, ABM has been found to be particularly effective when it exerts a significant change in baseline AB (Hakamata et al., Reference Hakamata, Lissek, Bar-Haim, Britton, Fox, Leibenluft, Ernst and Pine2010; Macleod & Grafton, Reference Macleod and Grafton2016; Price et al., Reference Price, Wallace, Kuckertz, Amir, Graur, Cummings and Bar-Haim2016). As a result, studies have investigated its effect for children and adolescents with anxiety disorders as well.
Several studies have examined the efficacy of ABM for the treatment of anxiety disorders in children and adolescents. A systematic review by Lowther and Newman (Reference Lowther and Newman2014) described ABM as a promising novel treatment for child and adolescent anxiety. However, the results of previous studies have been fairly inconsistent. The first randomised controlled trial (RCT) by Eldar and colleagues (Reference Eldar, Apter, Lotan, Edgar, Naim, Fox and Bar-Haim2012) showed ABM to be superior compared to its placebo condition (i.e., Attention Control Condition [ACC]) with large effect sizes. In contrast, four successive RCT studies found equal efficacy for ABM and ACC (Britton et al., Reference Britton, Bar-Haim, Clementi, Sankin, Chen, Shechner and Pine2013; Ollendick et al., Reference Ollendick, White, Richey, Kim-Spoon, Ryan, Wieckowski and Smith2019; Pergamin-Hight, Pine, Fox, & Bar-Haim, Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016; Shechner et al., Reference Shechner, Rimon-Chakir, Britton, Lotan, Apter, Bliese, Pine and Bar-Haim2014). Likewise, subsequent meta-analyses and review studies have not been conclusive about the effects of ABM compared to ACC for children and adolescents with anxiety disorders (Cristea, Mogoase, David, & Cuijpers, Reference Cristea, Mogoase, David and Cuijpers2015; Mogg, Waters, & Bradley, Reference Mogg, Waters and Bradley2017; Pennant et al., Reference Pennant, Loucas, Whittington, Creswell, Fonagy, Fuggle and Kendall2015). Several methodological factors have been reported that may explain contrasting results of ABM in alleviating anxiety in children and adolescents. These factors include the setting in which ABM is delivered (Price et al., Reference Price, Wallace, Kuckertz, Amir, Graur, Cummings and Bar-Haim2016), the type of stimuli used (Pergamin-Hight, Naim, Bakermans-Kranenburg, & Bar-Haim, Reference Pergamin-Hight, Naim, Bakermans-Kranenburg, van and Bar-Haim2015), and moderators of treatment efficacy such as the direction and extent of baseline AB and age of the participants (Cristea et al., Reference Cristea, Mogoase, David and Cuijpers2015; Van Bockstaele et al., Reference Van Bockstaele, Verschuere, Tibboel, De Houwer, Crombez and Koster2014).
The majority of studies have examined the efficacy of ABM for children and adolescents with anxiety disorders in a laboratory setting and have utilised facial stimuli for ABM. First, ABM has the potential to reduce treatment barriers of accessibility and cost-effectiveness for online, at-home training. Second, although negative facial expressions seem particularly ecological valid to represent threat for children with social phobia (SOP), faces have also been used for a range of other anxiety disorder subtypes. AB is more consistently observed when the stimuli used are anxiety disorder congruent (In-Albon, Kossowsky, & Schneider, Reference In-Albon, Kossowsky and Schneider2010; Pergamin-Hight et al., Reference Pergamin-Hight, Naim, Bakermans-Kranenburg, van and Bar-Haim2015; Waters, Lipp, & Spence, Reference Waters, Lipp and Spence2004). Therefore, adopting stimuli that are congruent with the targeted anxiety disorder subtypes may enhance the efficacy of ABM. Only one study has examined the effect of ABM delivered partly at home and with the use of general threat words instead of face stimuli. This study, by Chang and colleagues (Reference Chang, Kuckertz, Bose, Carmona, Piacentini and Amir2018), found relatively more children who received ABM to be treatment responders compared to ACC. However, for children and adolescents with anxiety disorders, words may have less ecological value compared to pictorial stimuli. Furthermore, given the high rate of comorbidity between anxiety disorder subtypes (Wittchen, Lecrubier, Beesdo, & Nocon, Reference Wittchen, Lecrubier, Beesdo, Nocon, Nutt and Ballenger2007), using different types of stimuli that correspond to the anxiety disorders that are targeted could be promising (Abend, de Voogd et al., Reference Abend, de Voogd, Salemink, Wiers, Pérez-Edgar, Fitzgerald and Bar-Haim2018).
In addition to these methodological factors, some previous studies have examined characteristics of participants that moderate the efficacy of ABM. First, the direction and extent of baseline AB may be related to the effect of ABM, as it is generally aimed to induce an attention away from threat. However, results have been fairly inconsistent with regard to the effect of baseline AB on ABM success (Eldar et al., Reference Eldar, Apter, Lotan, Edgar, Naim, Fox and Bar-Haim2012; Ollendick et al., Reference Ollendick, White, Richey, Kim-Spoon, Ryan, Wieckowski and Smith2019; Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016). Furthermore, Mogg et al. (Reference Mogg, Waters and Bradley2017) highlight that for most ABM studies, participants often do not show AB towards threat. Another factor that has been reported as a moderator is the age of participants. Larger reductions in anxiety after ABM have been shown for older children (Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016).
ABM has been suggested to improve treatment efficacy rates of CBT for children and adolescents with anxiety disorders (Bar-Haim, Reference Bar-Haim2010). The combination of ABM with CBT has been proposed to be beneficial as CBT involves more ‘top-down’ processes whereas ABM involves ‘bottom-up’ processes of information (Cisler & Koster, Reference Cisler and Koster2010). However, relatively few studies have examined the combined effect of ABM with CBT. Three previous studies have examined the efficacy of ABM-enhanced CBT, and one study reported significantly more reductions (White et al., Reference White, Sequeira, Britton, Brotman, Gold, Berman and Pine2017), while two other studies did not find an additive effect of ABM on CBT (Britton et al., Reference Britton, Bar-Haim, Clementi, Sankin, Chen, Shechner and Pine2013; Shechner et al., Reference Shechner, Rimon-Chakir, Britton, Lotan, Apter, Bliese, Pine and Bar-Haim2014). Thus, more research is needed to elucidate whether ABM has augmenting effects on CBT (Lowther et al., Reference Lowther and Newman2014). In these three studies, ABM was delivered in the laboratory before weekly CBT sessions, and stimuli of the ABM procedure consisted of faces.
The aim of the current study is to examine the efficacy of online ABM combined with CBT compared to online ACC with CBT for children and adolescents with anxiety disorders in a randomised, double-blind, placebo-controlled clinical trial. ABM has the potential to become a more accessible treatment when its efficacy can be shown outside the clinic or research centre. Therefore, the current study examined online ABM combined with face-to-face CBT for children and adolescents with anxiety disorders. Building further upon previous research, we utilised a combination of anxiety disorder-congruent stimuli for ABM and ACC. Another aim is to examine baseline AB and age as moderators of treatment success. We hypothesised that children with baseline AB towards threat benefit more from ABM with CBT (and less from ACC with CBT) compared to children with a baseline AB away from threat or no bias. Also, we hypothesised that older children benefit more from ABM (and not ACC) than younger children, as larger AB has been found in adolescents with anxiety disorders (Dudeney et al., Reference Dudeney, Sharpe and Hunt2015). Finally, as only two previous studies reported on follow-up effects at 3 months (Ollendick et al., Reference Ollendick, White, Richey, Kim-Spoon, Ryan, Wieckowski and Smith2019; Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016), we examined long-term effects of treatment at 6-month follow-up.
Methods
Participants
Eligible for participation in this randomised, double-blind, placebo-controlled, clinical trial were children aged between 8 and 16 years consecutively referred to the outpatient clinic of the Erasmus Medical Center, Sophia Children's Hospital or Lucertis Center for Child and Adolescent Psychiatry between September 2013 and July 2016, along with a primary diagnosis of separation anxiety disorder (SAD), social phobia (SOP), specific phobia (SP), or generalised anxiety disorder (GAD), according to the Anxiety Disorders Interview Schedule for DSM-IV Child and Parent Version (ADIS-IV-C). In total, 66 children fulfilled criteria for participation, of whom informed consent was obtained from 55 children and their parents (response rate 83.3%). Children were randomised via a computerised sequence to either online ABM + CBT (n = 28; M age = 11.62 years, SD = 2.52, 53.6% male) or online ACC + CBT (n = 27; M age = 10.67 years, SD = 1.91, 44.4% male). Participating children did not differ regarding gender, age, or severity score of primary anxiety diagnosis compared to eligible children who did not participate (ps > .10).
Exclusion criteria
Exclusion criteria were a full scale IQ of 85 or less (Wechsler Intelligence Scale for Children-III: Wechsler, Reference Wechsler1991), poor command of the Dutch language, serious physical disease, psychosis, substance abuse, autism spectrum disorders, obsessive-compulsive disorder, posttraumatic stress disorder, acute stress disorder, panic disorder, agoraphobia, major depression disorder, current anxiety medication, and psychotherapy in the past 6 months.
For all participating children, socioeconomic status (SES) was based on the residential area of their families by deriving SES-status z scores (Knol, Boelhouwer, &Veldheer, Reference Knol, Boelhouwer and Veldheer2012). This study was approved by the Medical Ethics Committee of the Erasmus Medical Center in Rotterdam (MEC-2013-375) and registered with ClinicalTrials.gov, number NCT03764644.
Sample size and interim futility analysis
We aimed to include 128 children to find a medium effect with 90% statistical power for our primary outcomes, based on the effect of ABM as monotherapy in adult clinical samples (Hakamata et al., Reference Hakamata, Lissek, Bar-Haim, Britton, Fox, Leibenluft, Ernst and Pine2010). Because of our unsatisfactory inclusion rate over time, the subsidy partner requested an interim futility analysis by an independent researcher when 48 participants were included. As the futility analysis showed a very low conditional power (P = −3.81, p < .0001) with a futility index above 0.9, the chance of finding different results if we reached our target sample size was futile (Jennison & Turnbull, Reference Jennison and Turnbull1999). Therefore, we independently decided to stop the recruitment of participants before the target sample size was reached. Seven participants who already participated in the study or agreed to participate completed their participation, resulting in a final sample size of 55 children.
Primary Outcomes
Anxiety disorder status
The Anxiety Disorders Interview Schedule for DSM-IV Child and Parent Version The ADIS-IV-C (Siebelink & Treffers, Reference Siebelink and Treffers2001; Silverman & Albano, Reference Silverman and Albano1996) was used to measure anxiety disorder status and the number of anxiety disorders. The ADIS-IV-C is a semi-structured interview and consists of a separate child and parent interview. Both parents and children were asked to rate the severity of symptom interference (0 = not at all; 8 = very much) when a sufficient amount of symptoms were endorsed. Administration of baseline (T1) anxiety disorder status with the ADIS-IV-C by experienced clinicians was part of the regular clinical procedure and hence not videotaped. For the interviews at T2, T3 and T4, administration by the first author (JdL) or a supervised research assistant were video-taped if parents gave their consent (91%). Clinician severity rating (CSR) was based on separate child and parent interviews. For CRS ≥ 4 an anxiety disorder was classified. Training on the ADIS-IV-C consisted of a workshop, practice interview and supervision by the last author (JL), who is a mental health psychologist. Twenty-six percent of the video-taped administrations were also scored by trained research assistants who were blind to randomisation and outcomes throughout the study for interrater agreement. Because of the dichotomisation of CRS scores for our analyses, interrater agreement was calculated based on anxiety disorder status instead of CRS scores. Interrater agreement across assessments after ABM or ACC (T2), after CBT (T3), and at follow-up (T4) was excellent (Κ = 0.94). The ADIS-IV-C has a good validity (Wood, Piacentini, Bergman, McCracken, & Barrios, Reference Wood, Piacentini, Bergman, McCracken and Barrios2002) and good to excellent test-retest reliability for the classification of the DSM-IV diagnoses of SAD, SOP, SP, and GAD (Silverman, Saavedra, & Pina, Reference Silverman, Saavedra and Pina2001).
Secondary Outcomes
Anxiety symptoms
The Dutch revised version of the Screen for Child Anxiety Related Emotional Disorders (SCARED-R; Birmaher et al., Reference Birmaher, Khetarpal, Brent, Cully, Balach, Kaufman and Neer1997; Muris, Steerneman, & Brinkman, Reference Muris, Steerneman and Brinkman2000) child, mother, and father report was used to assess anxiety symptoms. Questionnaires consisted of 69 items and a composite score was created by the sum of total scores of all informants divided by the number of informants. The SCARED-R has good internal consistency and moderate child-parent agreements, and excellent convergent validity and good test–retest reliability (Birmaher et al., Reference Birmaher, Brent, Chiappetta, Bridge, Monga and Baugher1999; Muris et al., Reference Muris, Merckelbach, Mayer, van Brakel, Thissen, Moulaert and Gadet1998). In the current study, internal consistency varied between .92 and .96 across informants and assessments. Correlations for the total score reports between children, mothers, and fathers ranged between r = .34 and r = .79 (ps < .05).
Depression symptoms
Child depression symptoms were assessed using the Child Depression Inventory (CDI; Kovacs, Reference Kovacs1992; Timbremont & Braet, Reference Timbremont and Braet2002), a 27-item questionnaire with good reliability (Finch, Saylor, Edwards, & McIntosh, Reference Finch, Saylor, Edwards and McIntosh1987) and validity (Timbremont, Braet, & Dreessen, Reference Timbremont, Braet and Dreessen2004). The CDI total score is the sum of all items, with higher scores representing more depressive symptoms. In the current study, internal consistency varied between .75 and .85 across assessments.
Attention Bias Measurement and Modification
Dot-probe task
AB in children was measured with the dot-probe detection task. This task was programmed using E-prime v2.0 (Psychology Software Tools, Inc.) and presented on a Fujitsu Lifebook computer in a quiet room with minimal visual and auditory distractions. In this task, a cross appeared in the middle of the screen for 500 ms followed by two pictures shown simultaneously (left and right) for 500 ms for each trial. Picture pairs were either threatening-neutral (128 trials) or neutral-neutral (32 trials) and followed by a probe in the spatial location previously occupied by one of the pictures. Probes consisted of two dots that were either placed next to each other (. .) or above each other (:) and were shown until one of the corresponding labelled keys were pressed. Participants were instructed to respond as accurately and quickly as possible. After ten practice trials, four blocks consisting of 40 trials each (160 trials in total) were performed. For threatening-neutral pairs, probes appeared in half of the trials at the same spatial location as the threatening picture (congruent trials) and in half of the trials at the opposite location of the threatening picture (incongruent trials).
Stimuli reflected all included anxiety disorders, with 40 stimuli pairs per subtype (SAD, SOP, SP, and GAD). For SAD, pictures that showed either separation (threatening) or reuniting (neutral) social scenarios of adults and children were used (In-Albon, Dubi, Rapee, & Schneider, Reference In-Albon, Dubi, Rapee and Schneider2009). Pictures of faces expressing anger or disgust (threatening), or neutral faces from a set of Japanese and Caucasian facial expressions of emotions (JACFEE; Biehl, et al., Reference Biehl, Matsumoto, Ekman, Hearn, Heider, Kudoh and Ton1997; Matsumoto & Ekman, Reference Matsumoto and Ekman1988) were used to reflect SOP. For SP, pictures were selected from the International Affective Picture System (IAPS; Lang, Bradley, & Cuthbert, Reference Lang, Bradley and Cuthbert1997) of animals (e.g., a barking dog), blood, and threatening phenomena in nature, along with neutral pictures. Four additional pictures of a tunnel and elevator were taken to ensure full coverage of different phobias. The first three blocks showed the SAD, SOP, and SP stimuli per participant in a randomised order. In the final block, threat-related and neutral words were selected from the Dutch Affective Words List for GAD (Moors et al., Reference Moors, De Houwer, Hermans, Wanmaker, van Schie, Van Harmelen and Brysbaert2013). Both the location and type of the probes, number of (in)congruent trials, and type of stimuli (for the first three blocks) were counterbalanced across trials. In this study, we calculated both disorder-congruent AB and average AB across anxiety disorder stimuli subtype as all children were presented with the same, mixed stimuli set.
Reaction times (RTs) were excluded from trials with errors, and if RTs were <200 ms, >1500 ms, and when >2.5 SD above the participant's mean RT. The average amount of missing trials was 15.1% (T1). In line with previous studies, AB scores were calculated by subtracting the average RT on congruent trials from the average RT on incongruent trials (Roy et al., Reference Roy, Vasa, Bruck, Mogg, Bardley and Sweeney2008). Positive values represent greater attention towards threatening compared to neutral stimuli, whereas negative values reflect attention away from the threatening relative to neutral stimuli.
Online ABM and ACC
Online ABM or ACC comprised a browser-based (Google Chrome or Firefox), nine-session program children followed over a period of three weeks. Online ABM and ACC consisted of the same stimuli, presentation time, and number of trials, as used in the dot-probe task. Probes always appeared in the spatial location of the neutral picture in the ABM, whereas the spatial location was counterbalanced in the ACC. Online ABM or ACC was monitored by the first author (JdL) by verifying the completion of the scheduled sessions in the remote online system. Parents were contacted to reschedule the session if children had not completed the session on a previously agreed day (online ABM and ACC adherence = 99.8%). For one participant, one of the nine sessions could not be rescheduled and was missed. Both groups had similar accuracy rates, as the average number of errors did not differ between the ABM group, M = 7.14, SD = 4.97 and ACC group, M = 7.42, SD = 3.87, t(53) = −0.24, p > .8. Also, mean reaction time (RT) was the same for the ABM group, M = 1039.21, SD = 359.67, and ACC group, M = 1040.74, SD = 315.83, t(53) = −0.02, p = 1.0.
Cognitive Behavioural Therapy (CBT)
Children followed individual CBT with the Dutch translation of the FRIENDS for Life program for children and adolescents (Barrett, Reference Barrett2014; Utens, de Nijs, & Ferdinand, Reference Utens, de Nijs and Ferdinand2001). This treatment comprises psychoeducation, relaxation and breathing exercises, exposure, problem-solving, social support training, and cognitive restructuring. The individual application of the FRIENDS program for children and adolescents with clinical anxiety includes ten weekly sessions and two booster sessions. CBT was given by licensed mental health psychologists or supervised master-level psychologists in training. CBT adherence was coded via a standardised protocol by trained research assistants, and analysis of a random selection of videotaped sessions showed that therapists adhered sufficiently (M CBT adherence = 2.45, SD = 0.48, scale range 0 = not at all to 3 = excellent) to the CBT protocol.
Procedure
Figure 1 displays the flow of participants throughout the study. The ADIS-IV-C, SCARED-R, and CDI were completed before participation in the study as part of the regular clinical procedures. At baseline assessment (T1), children completed the AB task and were randomly assigned to the ABM or ACC group. Children, parents, therapists and researchers were blind to the training condition. On the same day, children and parents were instructed about the online training. One week after online ABM or ACC, the second assessment (T2, total n = 55) took place. After CBT, children, and parents participated in the T3 assessment. Children and parents who were in the study at T3 were invited to participate 6 months after T3 for follow-up measurement (T4: M follow-up time in months = 5.93, SD = 0.62). Information about additional treatment (e.g., separate parent sessions, medication) was gathered at T4.
Figure 1. Flow of participants. Note: One participant from the ABM group needed more intensive treatment because of school-refusal and was not assigned to CBT. During CBT, six participants dropped out of the study equally divided over the ABM and ACC group (T3, total n = 48). Reasons for drop-out were unwillingness to continue CBT (n = 3) and worsening of symptoms (n = 3). At follow-up, 46 children participated with one drop-out (due to the perceived burden of the assessment) in each condition.
Statistical Analyses
To test for group differences in demographic and clinical characteristics at baseline we conducted chi-square tests and t tests. One-sample t tests were used to assess whether threat biases were significantly different from zero at baseline in both groups separately.
All time-related analyses were conducted with generalised estimating equations (GEE; Zeger & Liang, Reference Zeger and Liang1986; Zeger, Liang, & Albert, Reference Zeger, Liang and Albert1988). GEE allows for correlated observations (i.e., repeated measurements), accounts for missing data under the missing-at-random assumption, and accommodates outcomes that are normal, categorical, or count variables. For all analyses, we used an unstructured correlation matrix. Data were included from all participants who were randomised and completed at least one assessment (i.e., intention-to-treat analysis).
We used GEE for our primary and secondary outcomes. For the dichotomous outcome anxiety disorder status (primary outcome) we selected a binomial distribution and logit link function. For the count outcome number of anxiety disorders, a Poisson distribution with an identity link function was selected. For the continuous outcomes of anxiety symptoms, depression symptoms, and AB score a normal distribution with an identity link function was selected. For each outcome, we conducted two separate analyses. First, we examined the time interval including T1, T2, and T3. Second, we examined the interval from T3 to T4. In each analysis, we investigated the effect of group (ABM + CBT vs. ACC + CBT), time, and the interaction between group and time. The group-by-time interaction tested the treatment effect hypothesis of better primary and secondary outcomes over time for the ABM + CBT relative to the ACC + CBT group. Long-term treatment effects from T3 to T4 at follow-up were modelled with separate GEE analyses for all outcome measures because of the possibility that children received additional psychological treatment after CBT. Therefore, additional treatment (yes or no) was added to correct the analyses of long-term treatment effects. In addition, separate analyses for moderators of treatment effects (i.e., three-way interactions with the interaction between group and time and the moderators) from T1 to T3 and from T3 to T4 were conducted with age and baseline AB as continuous, centred variables. Statistical significance was determined using α = .05. All analyses were performed with SPSS version 24.
Results
Baseline Measures
No differences were found between groups regarding demographic and clinical characteristics (see Table 1). Average baseline AB scores were normally distributed and similar across groups. AB in the ABM group was not significantly different from zero (t = 0.42, p = .68), whereas the ACC group showed a bias towards threat (t = 2.19, p = .037). In the combined ABM and ACC sample, anxiety disorder-congruent AB was not significantly different from zero for children and adolescents with SAD (n = 15, M = 24.42, SD = 62.16, t = 1.52, p = .15), SOP (n = 19, M = −19.09, SD = 69.84, t = −1.19, p = .25), SP (n = 25, M = −19.39, SD = 100.99, t = −0.84, p = .41), and GAD (n = 29, M = 12.42, SD = 95.06, t = 0.70, p = .49). Therefore, further analyses with AB concern average AB and not anxiety disorder-congruent AB. The number of children that received additional treatment after CBT was the same for the ABM (n = 4, 17.4%) and ACC (n = 6, 26.1%) groups, χ2 (1) = 0.51, p = .48.
Table 1. Descriptive and Diagnostic Characteristics for Children in the Attention Bias Modification (ABM) + Cognitive Behavioural Therapy (CBT) Group and Attention Control Condition (ACC) + CBT Group at Baseline (T1)
Note: aSocioeconomic status represents a continuous (status) z score; bClinical severity rating (CRS) for the Anxiety Disorders Interview Schedule for DSM-IV Child and Parent Version (ADIS-IV-C); cSCARED-R = Screen for Child Anxiety Related Emotional Disorders; CDI = Child Depression Inventory.
Treatment Effects
Primary outcomes
Figure 2 and Table 2 show anxiety disorder status of children in the ABM and ACC group at T2, T3, and T4. Analyses indicated a significant change over time from T1 to T3 (Wald = 23.02, b = −0.17, SE = 0.05, p < .001) and from T3 to T4 (Wald = 11.04, b = −0.08, SE = 0.04, p = .046). However, no significant main effect of group or interaction effect between group and time was found. After 3-week online ABM and online ACC, 18.2% of the children no longer met the criteria for anxiety disorder status. After CBT, this percentage increased to 47.9%. At T4, 76.1% of the children were anxiety-disorder free.
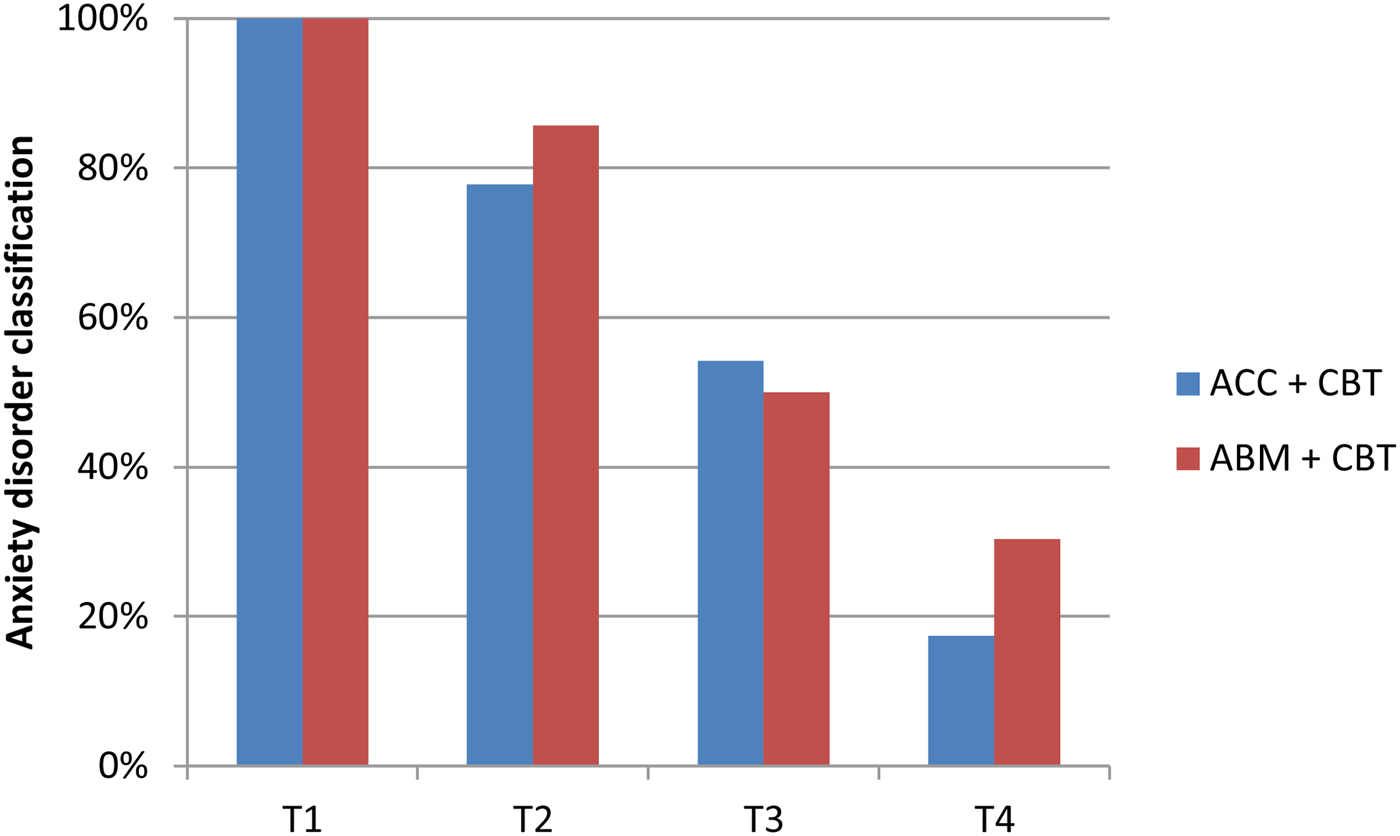
Figure 2. Changes in Anxiety Disorder Classification (ADIS-IV-C) throughout the study for the Attention Bias Modification (ABM) + Cognitive Behavioural Therapy (CBT) groups and the Attention Control Condition (ACC) and CBT groups.
Table 2. Descriptive Statistics of the Outcome Measures Throughout the Study for the Attention Bias Modification (ABM) + Cognitive Behavioural Therapy (CBT) Group and Attention Control Condition (ACC) + CBT Group
Note: aAverage attention bias score significantly different from zero; bCases with too few trials removed at T2 (one participant of the ABM + CBT and one participant of the ACC + CBT). ADIS-IV-C = Anxiety Disorders Interview Schedule for Children; SCARED-R = Screen for Child Anxiety Related Emotional Disorders; CDI = Child Depression Inventory.
Figure 3a and Table 2 show the change in the number of anxiety disorders across treatment and at follow-up. Although the decrease in the number of anxiety disorders was significant from T1 to T3 (Wald = 17.59, b = −0.06, SE = 0.02, p < .001) and from T3 to T4 (Wald = 11.00, b = −0.06, SE = 0.02, p < .001), no significant interaction effect between group and time or main effect of group was detected. From T3 to T4 a main effect for additional treatment was found (Wald = 4.11, b = 0.83, SE = 0.41, p = .043). Thus, for children who received additional treatment, the further decline in number of anxiety disorders from T3 to T4 was less evident. No significant interaction effect between group and time or main effect of group was found from T3 to T4.
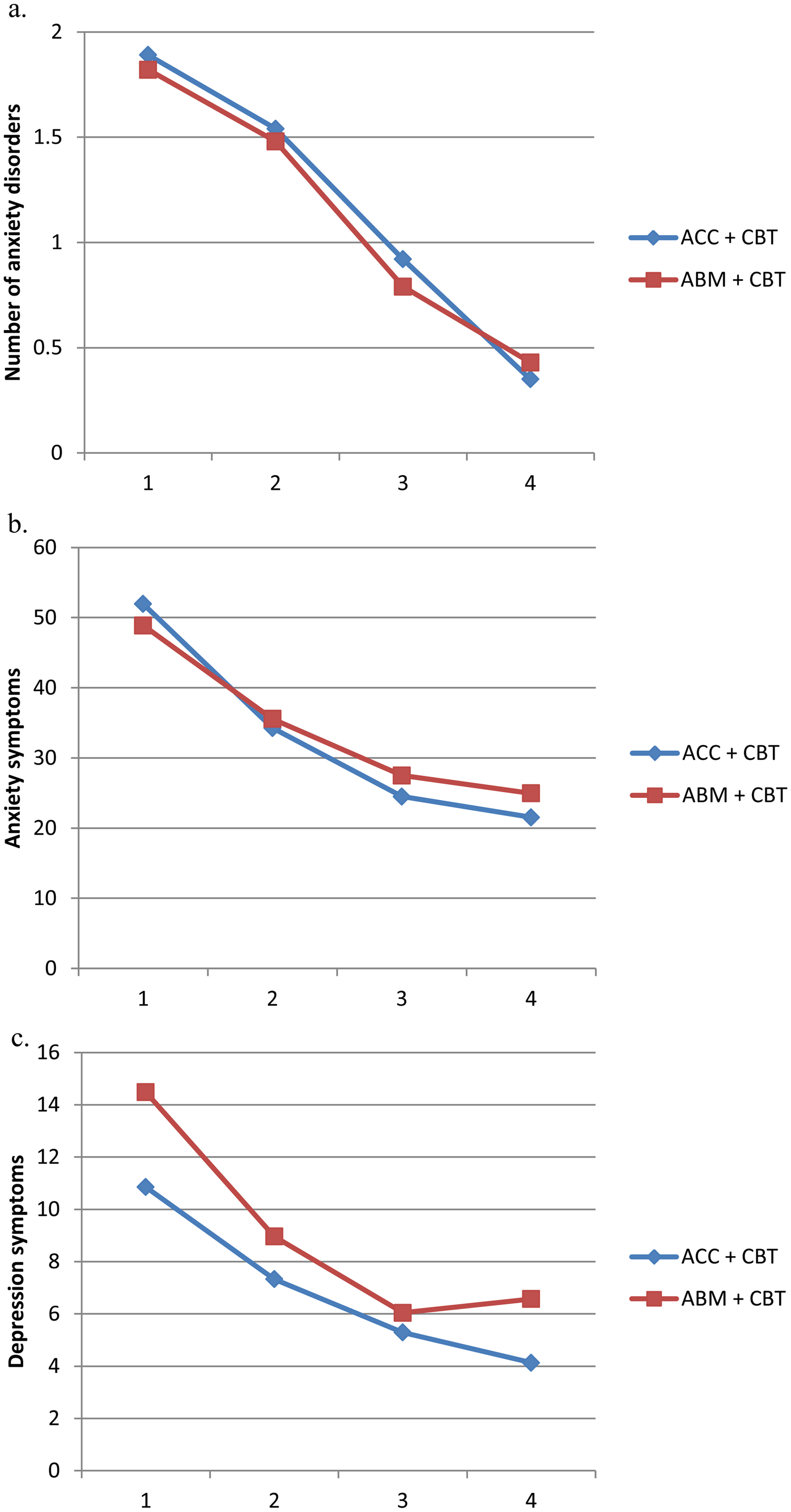
Figure 3. Change in the number of anxiety disorders (a), anxiety symptoms (b), and depression symptoms (c) after Attention Bias Modification (ABM) and the Attention Control Condition (ACC; T2), cognitive behavioural therapy (CBT; T3) and at 6-month follow-up (T4).
Secondary outcomes
Figure 3b and 3c, and Table 2 show the change in patient-reported anxiety and depression symptoms across treatment and at follow-up. Anxiety symptomatology decreased continuously throughout treatment from T1 to T3 (Wald = 17.96, b = −0.52, SE = 0.16, p = .001), but no changes were apparent from T3 to T4 (Wald = 2.38, b = −0.20, SE = 0.13, p = .12). No significant main effect of group or interaction effects between group and time were found.
Child-reported depression symptoms decreased from T1 to T3 (Wald = 32.35, b = −0.46, SE = 0.11, p < .001), whereas no significant main or interaction effects were found. At T4, a significant interaction effect between group and time was found (Wald = 4.95, b = −0.16, SE = 0.07, p = .026), with a larger decrease of depression symptoms for children in the ACC + CBT group compared to the ABM + CBT group. Also, a main effect for additional treatment (Wald = 5.41, b = 4.60, SE = 1.98, p = .020) was found, but no main effect of group or time.
Changes in AB from T1 to T3 were not significant across time (Wald = 1.06, b = −0.77, SE = 0.66, p = .24), and no interaction effect between group and time or main effect of group was found. From T3 to T4, a main effect of group (Wald = 4.62, b = 39.58, SE = 18.41, p = .032) and an interaction effect between group and time was found for changes in AB (Wald = 3.87, b = −1.76, SE = 0.90, p = .049). Although the direction of AB change from T3 to T4 was different across groups, AB at both assessments for the ABM + CBT group and ACC + CBT group were not significantly different from zero (Table 2).
Moderators of treatment effects
For both primary or secondary outcomes, no significant, three-way interactions between group, time, and the moderators’ baseline AB and age were found from T1 to T3 and from T3 to T4. Therefore, moderators of treatment effects were examined without the effect of group in the model. Also, for these analyses of primary and secondary outcomes, no significant two-way interactions of time and the moderators were found.
Discussion
This randomised, double-blind, placebo-controlled clinical trial examined the efficacy of online ABM combined with CBT for children and adolescents with anxiety disorders. Building further upon current knowledge in the field of ABM, we utilised anxiety disorder-congruent stimuli with the four included anxiety disorder subtypes to improve the targeting of AB. Moreover, we examined baseline AB and age as moderators of ABM efficacy. Finally, we conducted a long-term follow-up of all children 6 months after they completed ABM combined with CBT or ACC combined with CBT.
Although online attention training (ABM and ACC) combined with CBT was effective in reducing both clinician-rated anxiety disorders and patient-reported anxiety and depression symptomatology, no differences were found between the ABM and ACC condition. The results indicate that when ABM is delivered online, with stimuli that match all anxiety disorders targeted and in combination with CBT, it is no more effective than ACC. Thus although the current study used a different methodological approach than previous studies, we did not find a superior effect of ABM. This finding is in line with four previous RCTs in children with anxiety disorders (Britton et al., Reference Britton, Bar-Haim, Clementi, Sankin, Chen, Shechner and Pine2013; Ollendick et al., Reference Ollendick, White, Richey, Kim-Spoon, Ryan, Wieckowski and Smith2019; Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016; Shechner et al., Reference Shechner, Rimon-Chakir, Britton, Lotan, Apter, Bliese, Pine and Bar-Haim2014). A significant augmented effect of ABM over ACC has only been reported by one study for clinician-rated symptoms, but not for anxiety disorder status (White et al., Reference White, Sequeira, Britton, Brotman, Gold, Berman and Pine2017). Therefore, results of the current and previous studies show that ABM as an adjunct to CBT does not have a superior effect on anxiety disorder status and that the findings for a beneficial effect of ABM over ACC for patient-reported outcomes are inconsistent and at most modest. Even if there are modest effects of ABM on patient-reported outcomes, these do not outperform the general effectiveness of CBT for anxiety disorders in children and adolescents (James et al., Reference James, James, Cowdrey, Soler and Choke2015).
Clinician-reported and patient-reported anxiety symptomatology decreased continuously for children in both the ABM and ACC conditions throughout the study. In line with previous studies, decreases in anxiety symptoms were not accompanied by changes in AB (Mogg, Waters, & Bradley, Reference Mogg, Waters and Bradley2017). Possibly other mechanisms are involved in the reduction of anxiety during attention training. Both ABM and ACC have been previously described to increase top-down cognitive control over processing threat stimuli irrelevant to the task performed, that is, attentional control. Top-down cognitive control is the deployment of attention that is based on voluntary goals and expectations (Itti & Koch, Reference Itti and Koch2001). Poor attentional control has previously been associated with AB in anxious individuals (Derryberry & Reed, Reference Derryberry and Reed2002). Therefore, an increase in top-down cognitive control might explain the decreases in anxiety symptoms in both training conditions (Cisler & Koster, Reference Cisler and Koster2010).
Reductions in anxiety symptoms in both attention training groups may also be due to exposure to threatening stimuli. This explanation is also proposed in the review of Mogg and colleagues (Reference Mogg, Waters and Bradley2017). Numerous studies have shown that exposure is a very effective strategy to diminish anxiety problems (Seligman & Ollendick, Reference Seligman and Ollendick2011; Weisz et al., Reference Weisz, Kuppens, Ng, Eckshtain, Ugueto, Vaugh-Coaxum and Fordwood2017). Future studies are needed to examine the influence of exposure on attention training effects; for example, by comparing ABM and ACC to an exposure control condition in which patients are only exposed to threatening stimuli. In addition, a placebo control condition with exposure to neutral stimuli should be incorporated to rule out that decreases in anxiety are attributable to retest effects that are commonly observed within clinical samples (Arrindell, Reference Arrindell2001).
Our study is the first to examine the effect of ABM and ACC delivered fully online in a clinical sample of children and adolescents with anxiety disorders. In contrast to our findings, relatively more children were found to be treatment responders in the ACM group than the ACC group by Chang and colleagues (Reference Chang, Kuckertz, Bose, Carmona, Piacentini and Amir2018). However, children in the study by Chang et al. also completed an ABM or ACC session at the laboratory, besides performing the training at home for eight sessions. Other studies with full online delivery also did not find a beneficial effect of ABM compared to ACC for subclinical anxiety symptoms in adolescents (de Voogd et al., Reference de Voogd, Wiers, Prins, de Jong, Boendermaker, Zwitser and Salemink2016; Sportel, de Hullu, de Jong, & Nauta, Reference Sportel, de Hullu, de Jong and Nauta2013) and adults with SOP (Boettcher et al., Reference Boettcher, Leek, Matson, Holmes, Browning, MacLeod, Andersson and Carlbring2013; Enock, Hofmann, & McNally, Reference Enock, Hofmann and McNally2014; Neubauer et al., Reference Neubauer, von Auer, Murray, Petermann, Helbig-Lang and Gerlach2013). Although treatment adherence in our study was almost perfect (99.8%) and children made relatively few errors during attention training, mean RTs were rather large. Children may respond differently to ABM at home than in a research or hospital setting because of several reasons. Performing the training in an uncontrolled setting most likely brings along distractions, which was shown in the current study by relatively large RTs. Also, training in a research centre may be related to other non-specific effects such as treatment structure, motivation, and the participants’ outcome expectations, also described as a variant of the experimenter effect (Cristea, Kok, & Cuijpers, Reference Cristea, Kok and Cuijpers2015; Linetzky, Pergamin-Hight, Pine, & Bar-Haim, Reference Linetzky, Pergamin-Hight, Pine and Bar-Haim2015). When performed at home, more explicit learning could be achieved by introducing explicit goal-setting, feedback, and variation of training to increase engagement (Mogg & Bradley, Reference Mogg and Bradley2018). For example, a series of studies by Waters and colleagues (Waters, Pittaway, Mogg, Bradley & Pine, Reference Waters, Pittaway, Mogg, Bradley and Pine2013; Waters et al., Reference Waters, Zimmer-Gembeck, Craske, Pine, Bradley and Mogg2015, Reference Waters, Zimmer-Gembeck, Craske, Pine, Bradley and Mogg2016) found a novel online attention training, including techniques to consolidate the positive-search strategies, to be more effective than a control condition or wait-list control group for children with anxiety disorders.
In the current study, baseline AB and age neither moderated the effect of ABM, nor explained differences in symptom reduction throughout the study. A previous study found the efficacy of ABM relative to ACC for children with SOP above the age of 13 (Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016). The median age of our sample was lower (10 years), and this might explain why we did not find a moderating effect of age. Moreover, recent studies found a positive association between treatment gains and baseline AB for adults and not for children or adolescents (Abend, de Voogd et al., Reference Abend, de Voogd, Salemink, Wiers, Pérez-Edgar, Fitzgerald and Bar-Haim2018; Abend, Naim et al., Reference Abend, Naim, Pergamin-Hight, Fox, Pine and Bar-Haim2018). We also did not find baseline AB to be related to the efficacy of ABM, which is generally in line with previous studies (Ollendick et al., Reference Ollendick, White, Richey, Kim-Spoon, Ryan, Wieckowski and Smith2019; Pergamin-Hight et al., Reference Pergamin-Hight, Pine, Fox and Bar-Haim2016). It should also be noted that children in the ABM, whose attention was trained towards neutral, did not show a baseline bias, whereas children in the ACC group showed a bias towards threat. In contrast to our expectations, children and adolescents did not show an anxiety disorder-congruent AB at baseline. This could also explain why in our study ABM was not superior to ACC. Another explanation is low reliability and a paucity of research on the psychometric properties of the dot-probe task (Cisler, Bacon & Williams, Reference Cisler, Bacon and Williams2009; Roy, Dennis & Warner, Reference Roy, Dennis and Warner2015).
The current study has several strengths worth mentioning. By using online ABM and ACC, this is the first study to examine the efficacy of online ABM combined with CBT for children and adolescents with anxiety disorders. In addition, by combining stimuli that matched all included anxiety disorders, content-specificity of the training was attuned. Nevertheless, the current study should also be seen in the light of the following limitations. Our sample size was low, which may have hampered detecting significant effects. However, as futility analyses showed a very low chance of finding a significant effect when our target sample size was reached, lack of statistical power was limited to the moderation analyses. Although the training stimuli represented all included anxiety disorders, stimuli were not personalised. Also, the stimuli used to represent SAD consisted of more complex pictures (i.e., scenes of children separating or reuniting with a parent) than the other stimuli. Even though comorbidity in the current study was high and we specifically aimed to target this, the combination of stimuli that required more processing (SAD and GAD), with less complex stimuli (SOP and SP) may have also led to the measurement and training of different stages of AB. Finally, we did not include a CBT-only condition to contrast findings of the ABM and ACC group.
The findings of the current study have several implications for clinical practice and future research. As our study adds to the growing body of research that questions the efficacy of ABM for children and adolescents with anxiety disorders, implementing ABM into clinical practice is not advised. Although we used anxiety disorder-specific stimuli, this did not lead to improved efficacy of ABM. More research is needed that examines which elements of ABM explain decreases in anxiety symptoms, such as increases in top-down cognitive control during exposure of threatening stimuli regardless of bias modification. In addition, combining training attention control with more goal-oriented exercises may be more effective in addressing the complex circuit of cognitive control functions involved in anxiety (Mogg et al., Reference Mogg, Waters and Bradley2017).
Conclusion
We did not find a benefit of online ABM with anxiety disorder-congruent stimuli in combination with CBT for the treatment of children and adolescents with anxiety disorders in a randomised, double-blind, placebo-controlled trial. Although anxiety symptomatology decreased throughout the study and improvements remained at the 6-month follow-up, no differences between ABM and ACC were found. More research is needed to identify active elements of attention training for children and adolescents with anxiety disorders.
Author ORCIDs
Jasmijn M. de Lijster, 0000-0002-7322-7877.
Funding
This work was supported by the Sophia Children's Hospital Research Foundation (SSWO), Project S13-11 and the Coolsingel Foundation, Project 251.
Declaration of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.









