Introduction
Exposure to potentially traumatic events, post-migration challenges and other psychological stressors can place conflict-affected populations at an increased risk of common mental disorders, such as depression, anxiety and post-traumatic stress disorder (PTSD) (Fazel et al., Reference Fazel, Wheeler and Danesh2005; Turrini et al., Reference Turrini, Purgato, Ballette, Nosè, Ostuzzi and Barbui2017; Giacco et al., Reference Giacco, Laxhman and Priebe2018; Kien et al., Reference Kien, Sommer, Faustmann, Gibson, Schneider, Krczal, Jank, Klerings, Szelag, Kerschner, Brattström and Gartlehner2019). Among displaced and conflict-affected populations, the World Health Organization (WHO) estimates the age-standardised prevalence of depression to be 10.8%, anxiety disorders (including PTSD) 21.7% and PTSD alone 15.3% (Charlson et al., Reference Charlson, Van Ommeren, Flaxman, Cornett, Whiteford and Saxena2019). These estimates are considerably higher than WHO estimates for common mental disorders among the general global population, at 4.4% for depression and 3.6% for anxiety disorders (including PTSD) (World Health Organization, 2017).
Included among those at risk are persons affected by the war in Syria, with an estimated 13.1 million requiring humanitarian assistance within Syria itself, and a further 5.6 million displaced across Europe and neighbouring countries (United Nations High Commissioner for Refugees, 2019). Evidence from these settings signals elevated levels of common mental disorders among displaced Syrian refugees. The majority of the available evidence comes from adult populations, with prevalence estimates ranging from 14% to 44% for depression (Naja et al., Reference Naja, Aoun, El Khoury, Abdallah and Haddad2016; Tinghög et al., Reference Tinghög, Malm, Arwidson, Sigvardsdotter, Lundin and Saboonchi2017; Acarturk et al., Reference Acarturk, Cetinkaya, Senay, Gulen, Aker and Hinton2018; Georgiadou et al., Reference Georgiadou, Zbidat, Schmitt and Erim2018; Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019), 13% to 36% for anxiety (Tinghög et al., Reference Tinghög, Malm, Arwidson, Sigvardsdotter, Lundin and Saboonchi2017; Georgiadou et al., Reference Georgiadou, Zbidat, Schmitt and Erim2018; Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019) and 11% to 83% for PTSD (Alpak et al., Reference Alpak, Unal, Bulbul, Sagaltici, Bez, Altindag, Dalkilic and Savas2015; Tinghög et al., Reference Tinghög, Malm, Arwidson, Sigvardsdotter, Lundin and Saboonchi2017; Acarturk et al., Reference Acarturk, Cetinkaya, Senay, Gulen, Aker and Hinton2018; Chung et al., Reference Chung, Alqarni, Almazrouei, Al Muhairi, Shakra, Mitchell, Al Mazrouei and Al Hashimi2018; Georgiadou et al., Reference Georgiadou, Zbidat, Schmitt and Erim2018; Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019). Evidence among Syrian children is more limited, although findings consistently demonstrate symptoms of common mental disorders (Hamdan-Mansour et al., Reference Hamdan-Mansour, Abdel Razeq, Abdulhaq, Arabiat and Khalil2017; Yayan et al., Reference Yayan, Düken, Özdemir and Çelebioğlu2020). The majority of these studies focus on PTSD, with prevalence estimates ranging from 33% to 50% (Ozer et al., Reference Ozer, Sirin and Oppedal2013; Soykoek et al., Reference Soykoek, Mall, Nehring, Henningsen and Aberl2017; Eruyar et al., Reference Eruyar, Maltby and Vostanis2018).
An estimated 3.6 million displaced Syrians live in Turkey, of whom almost half are children and adolescents under the age of 18 (United Nations High Commissioner for Refugees, 2020). One study, conducted in Islahiye camp near the Syria border, found that exposure to traumatic events and common mental disorders was high among Syrian children (Ozer et al., Reference Ozer, Sirin and Oppedal2013). The majority (74%) had experienced a family member dying, and 58% had experienced a stressful life event in which they believed their life was in danger. Nearly half of children in this study were found to have symptoms of PTSD, and 20% were identified as having a depressive disorder (Ozer et al., Reference Ozer, Sirin and Oppedal2013). Of these, significantly more girls than boys reported symptoms of depression.
The majority of Syrians (96%) in Turkey do not live in refugee camps, but rather live among the host population. This includes 550 000 Syrians currently living in Istanbul (Ministry of Interior: Directorate General of Migration Management, 2019). A survey among adult Syrian refugees living in Sultanbeyli district of Istanbul, conducted in 2018, found a high prevalence of depression (34.7%), anxiety (36.1%) and PTSD (19.6%), with the majority screening positive for these conditions not seeking care of any kind. However, data were not collected for children (Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019). To the best of our knowledge, just one study has previously been conducted with Syrian children living among the host population in Istanbul, with common mental disorders found to be common (Eruyar et al., Reference Eruyar, Maltby and Vostanis2018). Half of the children surveyed scored above the clinical cut-off for PTSD, with 24% judged to have ‘very high’ general mental health problems. However, this was a school-based study and community-based surveys are lacking.
Epidemiological data, identifying prevalence and factors associated with increased risk of common mental disorders, are important for informing the development of public mental health policy, special education and psychosocial support initiatives, and programming for Syrian children living among the host population in Turkey.
The objectives of the current study are to: (1) estimate the prevalence of symptoms of common mental disorders (depression, anxiety and PTSD) among Syrian refugee children living in Sultanbeyli district of Istanbul; and (2) identify associations between symptoms of common mental disorders and socio-demographic characteristics.
Methods
Study design and sampling
This cross-sectional study was conducted between August and October 2019 in Sultanbeyli District, Istanbul, as part of an all-age population-based survey of disability among Syrian refugees, aged 2+ years. This paper reports specifically on mental health data collected among children and adolescents aged 8–17 years.
Based on evidence from similar populations, the prevalence of common mental disorders among children and adolescents aged 8–17 years was estimated to be 15%. Incorporating precision of 20% around the estimates, 95% confidence, 20% non-response and a design effect of 1.7, we required a sample size of 1073 participants aged 8–17 years. The total sample size calculated for the all-age survey of disability was 4000.
The local municipality's database of registered Syrian refugees provided the sampling frame, from which we selected the study population using a two-stage sampling technique. First, we randomly selected 80 clusters, of 50 participants each (a total all-age sample of 4000), using probability proportionate to size sampling. A cluster was defined as a single street within Sultanbeyli District. Within each cluster, we randomly selected households until at least 50 participants were included. When a single street (‘cluster’) did not contain 50 participants, we randomly selected additional households from randomly selected connecting and adjacent streets, until the target number was reached.
Across all 80 clusters, enumerators visited households door-to-door, tallying participants until at least 50 people were included. For this survey, all Syrians within selected households were included in the survey, regardless of their legal ‘Temporary Protection’ status. To maximise the response rate, enumerators telephoned households in advance, where possible, to inform them of the survey purpose and arrange a suitable time to visit. If unavailable, enumerators attempted to revisit the household at another time, including evenings and weekends.
Survey questionnaires
Upon consent from the head of each household, enumerators completed a household roster, gathering socio-demographic information.
Symptoms of common mental disorders were subsequently assessed in each child aged 8–17 years using direct self-report questionnaires. Depression was assessed using the Center for Epidemiologic Studies Depression Scale for Children (CES-DC), anxiety using the Screen for Child Anxiety Related Disorders (SCARED) and PTSD using the Child Revised Impact of Event Scale (CRIES-8). Each of these tools has been previously used in research with refugee populations (Eruyar et al., Reference Eruyar, Maltby and Vostanis2018; Kandemir et al., Reference Kandemir, Karataş, Çeri, Solmaz, Kandemir and Solmaz2018; Perkins et al., Reference Perkins, Ajeeb, Fadel and Saleh2018). To limit the response burden, we used abbreviated versions of the CES-DC and SCARED, validated for use with Syrian refugee children living in Lebanon (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020).
Each of these screening tools results in a total score, indicating high or low symptomology. These tools are designed to screen symptomology, not to provide a diagnosis, which is typically done through a clinical interview with a trained mental health specialist. Screening tools of this kind have typically been validated against clinical interviews and the cut-off scores indicate the level at which a child is likely to receive a diagnosis.
Center for Epidemiologic Studies Depression Scale for Children (CES-DC)
The CES-DC measures the frequency and duration of symptoms associated with depression in children and adolescents (Faulstich et al., Reference Faulstich, Carey, Ruggiero, Enyart and Gresham1986). This measure has been adapted to an abbreviated 10-item version (CES-DC-10Sy) by Queen Mary University and their research partners, for use with Syrian children in Lebanon (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020). The 10-item version showed good internal consistency (Cronbach's α = 0.89) and was used in this study after consultation with the research team at Queen Mary University. This abbreviated version asks children to respond to statements (‘items’) across a four-point Likert scale, identifying to what extent they experienced a given feeling in the past month: (0) not at all; (1) a little; (2) some; (3) a lot. The validated cut-off score among Syrian children of 10, from a total of 30, indicates symptomatic depression and those children at risk of clinical diagnosis (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020).
Screen for Child Anxiety Related Disorders (SCARED)
The SCARED screens children and adolescents for anxiety disorders, including general anxiety disorder, panic disorder and separation anxiety disorder (Birmaher et al., Reference Birmaher, Khetarpal, Brent, Cully, Balach, Kaufman and Neer1997). We used the abbreviated version developed by Queen Mary University (SCARED-18Sy), previously validated for use with Syrian children in Lebanon, and found to have good internal consistency (Cronbach's α = 0.84) (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020). The abbreviated measure used in this study scored the 18 items across a three-point scale: (0) not true or hardly ever true; (1) somewhat true or sometimes true; (2) very true or often true. The validated cut-off of 12, from a maximum score of 36, indicates symptomatic anxiety (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020).
Child Revised Impact of Event Scale (CRIES-8)
The CRIES tool is designed to assess symptoms of PTSD (Perrin et al., Reference Perrin, Meiser-Stedman and Smith2005). The eight-item version (hence CRIES-8) demonstrates good psychometric properties among conflict-affected populations and has been previously used with Syrian refugee children in Turkey (Ozer et al., Reference Ozer, Sirin and Oppedal2013; Eruyar et al., Reference Eruyar, Maltby and Vostanis2018). Among refugee minors in Sweden (including Arabic speakers), internal consistency was found to be acceptable (Cronbach's α = 0.75) (Salari et al., Reference Salari, Malekian, Linck, Kristiansson and Sarkadi2017). The tool is designed to measure the intrusion and avoidance of unwanted thoughts, feelings and memories, and items are scored on a four-point scale: (0) not at all; (1) rarely; (3) sometimes; (5) often. Items ask children to report how frequently comments were true for them in the past 7 days, when thinking about a stressful life event. From a maximum score of 40, the cut-off of 17 indicates symptomatic PTSD.
Child Youth and Resilience Measure (CYRM)
In addition to an assessment of symptoms of common mental disorders, we also assessed resilience in children aged 12–17 years, using a modified 12-item version of the CYRM, which has been validated for use with Syrian adolescents (Panter-Brick et al., Reference Panter-Brick, Hadfield, Dajani, Eggerman, Ager and Ungar2018). Internal consistency was found acceptable (Cronbach's α = 0.75) in this validation study. Using this tool, children are asked to rate the extent to which a statement is relevant to them, on a four-point scale: (1) not at all; (2) a little; (3) somewhat; (4) quite a bit. Higher scores indicate a higher level of personal resilience as a protective factor against the onset of mental distress, with a maximum score of 48.
Existing Arabic versions of each tool were independently back-translated into English, assessing accuracy, conceptual equivalence and cultural acceptance. These tools were subsequently piloted with members of the target population by technical experts (each a native Syrian Arabic speaker), who shared recommendations of minor amendments for use with this population.
Data collection
Enumerators administered each of the self-report questionnaires directly with a child, within their home. If requested (by child or caregiver), a parent/guardian/caregiver remained present throughout the interview. Enumerators conducted the interview in Arabic. Visual aids (an example of which is seen in Appendix 1) were used to help children understand the questionnaire responses. Each of the enumerators had completed a 10-day training, covering the aims of the survey, interview techniques, mental health and disability sensitisation, data entry procedures and ethical responsibilities.
Data were collected on android tablets using the London School of Hygiene & Tropical Medicine's Open Data Kit software. Collected data were encrypted and uploaded to a secure cloud-based server at the end of each day.
Data analysis
Data were analysed using STATA version 14.0. Prevalence estimates (with 95% CI) were calculated from those children scoring at or above the cut-off on each measurement tool. These estimates were stratified by age, sex and socio-economic status. The ‘svv’ command in STATA was used to account for the cluster sampling methods.
Principal components analysis was used to derive a socio-economic index from household level indicators such as household asset ownership, type of residence and source of heating. The resulting socio-economic score was divided into quartiles, from the poorest to least poor. The first principal component accounted for 14.96% of the variation in the original data.
Multivariate regression analyses were undertaken to assess the relationship between each common mental disorder and individual (age, sex, years since displacement, education and resilience), household level (household size, household head and socio-economic status) and socio-demographic characteristics.
Ethical approval
Ethical approval was granted by Istanbul Sehir University, Republic of Turkey Ministry of Interior: Directorate General of Migration Management and the London School of Hygiene & Tropical Medicine.
Informed written consent was sought from the self-identified head of each household prior to completion of the household roster and collection of demographic information. Informed consent was subsequently sought from parents and caregivers for children and adolescents aged 8–17 years. Verbal assent was also sought from the children and adolescents.
Results
Study population
Of 1080 eligible participants aged 8–17 years, 852 took part in the survey (response rate of 79%), 157 were unavailable (15%) and 71 (7%) refused. The sample characteristics of these participants are provided in Table 1.
Table 1. Sample characteristics (n = 852)

a Data missing.
Of the study sample, 439 (51%) were female and 413 (49%) male. Compared to participants, non-participants were, on average, slightly older (participants: 11.9 years, 95% CI 11.7–12.9 years; non-participants: 12.9 years, 95% CI 12.5–13.2, p < 0.01) and more likely to be male (participants: 49%; non-participants: 59%). Overall, the sample age distribution was largely comparable to the registration database used for the sampling frame, with slight under-representation of older children.
On average, participants in the study had been displaced from Syria approximately 4 years prior to the study. The vast majority of children lived in a flat/apartment (81%) or house (16%). In terms of the highest education level attained, 73% had attended primary school, 20% had attended secondary school and 6% had never attended formal education (given the age distribution of the sample, it is important to note that not all children were eligible to have attended secondary school).
Prevalence of common mental disorders
The estimated prevalence of symptomatic depression, anxiety and PTSD were 12.5% (95% CI 9.8–15.6), 9.2% (95% CI 6.8–12.1) and 11.5% (95% CI 9.1–14.4), respectively (Table 2). Overall, 23.7% (95% CI 19.9–27.2) had symptoms of one or more of these common mental disorders.
Table 2. Prevalence of common mental disorders, by age and sex
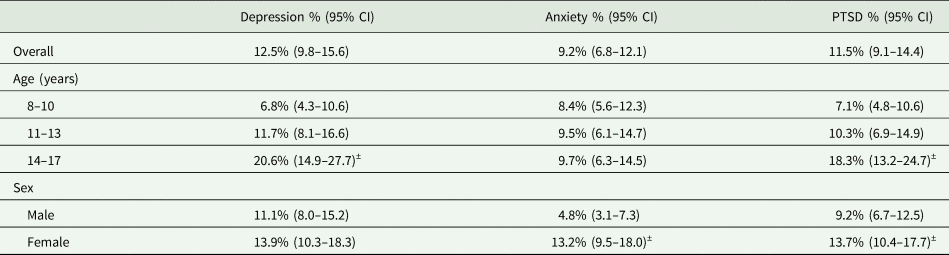
± Significant at p < 0.05.
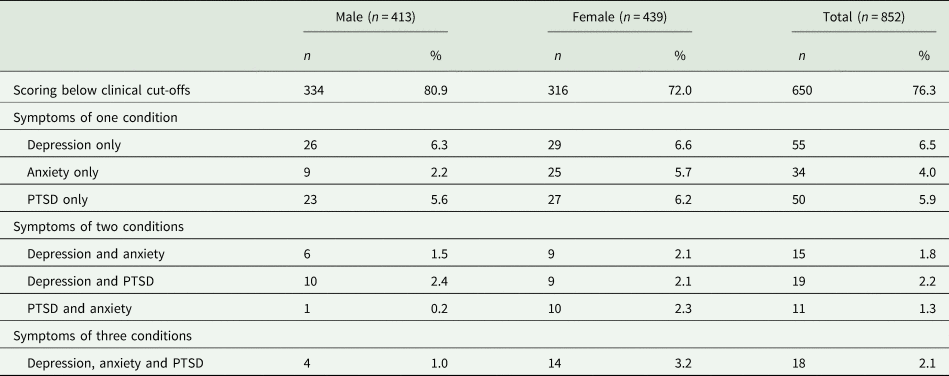
As seen in Table 3, 16.4% screened positive for symptoms of just one condition only, 5.3% showed symptoms across two conditions and 2.1% were found to have symptoms of all three common mental disorders.
Table 3. Distribution of symptomology, by common mental disorder
Association with resilience
Children with symptoms of depression demonstrated significantly lower mean resilience scores (59.0, 95% CI 55.0–63.1) compared to children without symptomatic depression (71.2, 95% CI 69.5–72.9), as shown in Table 4. There was no association observed between resilience score and symptoms of anxiety or PTSD.
Table 4. Association between common mental disorders and resilience
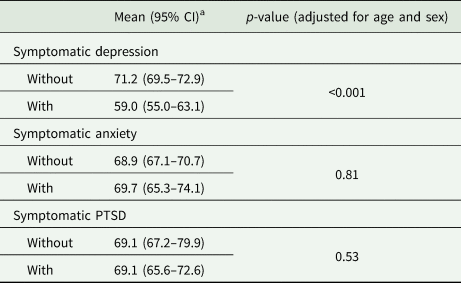
a Higher score indicates a greater level of resilience.
Association with socio-demographic variables
Table 5 presents the association between each common mental disorder and socio-demographic variables, adjusted for age and sex. Older children (14–17 years) were three times more likely to experience symptomatic depression (adjusted odds ratio (aOR): 3.6, 95% CI 2.1–6.8) and PTSD (aOR: 3.0, 95% CI 1.7–5.2) compared to younger (8–10 years) children, although this association was not observed for anxiety. Symptomatic anxiety (aOR: 2.9, 95% CI 1.8–4.9) and PTSD (aOR: 1.6, 95% CI 1.1–2.4) were more common among girls, with no association observed for depression. Demonstrating symptoms of these common mental disorders was not significantly associated with the number of years since leaving Syria. Symptomatic depression was more common in children who had received no education (aOR: 2.3, 95% CI 1.0–5.2), although no association was seen for PTSD or anxiety. Symptomatic PTSD was found to be significantly less likely to occur in children living in a household with 8+ members (aOR: 0.5, 95% CI 0.3–0.9), compared to those living in households of 2–4. Household size was not associated with symptomology of depression or anxiety, and the sex of the head of the household was not associated with any common mental disorder. Symptomatic depression was slightly more common among children who lived in the poorest households, although this was of borderline significance (aOR: 2.0, 95% CI 1.0–3.5). Socio-economic status was not associated with either PTSD or anxiety.
Table 5. Association between common mental disorders and socio-demographic variables
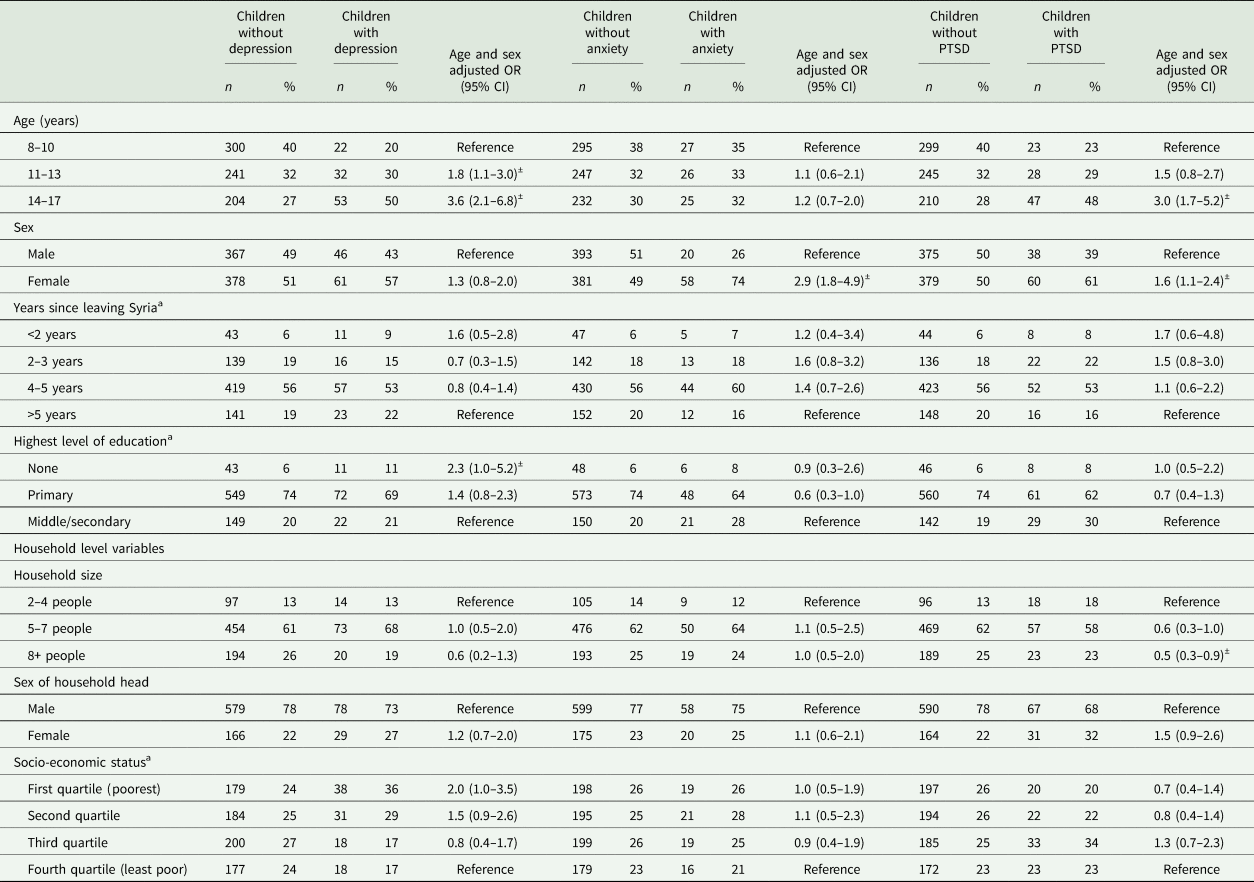
± Significant at p < 0.05.
a Data missing.
Discussion
This study reports on the prevalence and socio-demographic predictors of common mental disorders among Syrian children living in Istanbul. Nearly a quarter (23.7%) of children screened positive for symptoms of at least one common mental disorder. By condition, 12.5% screened positive for symptomatic depression, 9.2% for anxiety and 11.5% PTSD. Older children were more likely to screen positive for symptomatic depression and PTSD, with girls more likely to screen positive for anxiety and PTSD. Depression was more common among children who had received no education and were from the poorest households.
These estimates fall at the lower end of prevalence figures identified in a recent systematic review of studies among young refugees (under 18 years) displaced across Europe, in which estimates ranged from 10.3–32.8% for depression, 19–52.7% for PTSD and 8.7–31.6% for anxiety (Kien et al., Reference Kien, Sommer, Faustmann, Gibson, Schneider, Krczal, Jank, Klerings, Szelag, Kerschner, Brattström and Gartlehner2019). Our findings on PTSD do, however, align with evidence from an umbrella review conducted by Turrini et al., which identified five surveys of 260 refugee children that generated an estimate of 11% for PTSD, similar to that in our study (Turrini et al., Reference Turrini, Purgato, Ballette, Nosè, Ostuzzi and Barbui2017). The wide variation in these estimates may reflect the varying study and sampling methodologies, and the different screening tools, as well as the different characteristics of the refugee groups and host communities.
Overall, our study indicates a substantial burden of common mental disorders among Syrian children in Istanbul, with nearly a quarter of children demonstrating symptoms of at least one common mental disorder. Our estimates are considerably higher than estimates from the WHO for the general population and are congruent with the evidence of a substantial burden of common mental disorders among Syrian refugees (Ozer et al., Reference Ozer, Sirin and Oppedal2013; World Health Organization, 2017; Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019).
Eruyar et al.'s study among Syrian school children in Istanbul estimated the prevalence of PTSD to be 50% using CRIES-8, the same screening tool used in our study (Eruyar et al., Reference Eruyar, Maltby and Vostanis2018). This estimate is considerably higher than that identified in our study, although their sample was recruited from two Syrian schools only, limiting the comparison to our community-based survey. Similarly, the prevalence of PTSD was estimated to be higher among children living in Islahiye camp, in South-Eastern Turkey (Ozer et al., Reference Ozer, Sirin and Oppedal2013). This study also utilised the CRIES-8, with 45% of children reaching the cut-off for symptomatic PTSD. Further, 44% screened positive for depression, of whom 20% reached the clinical cut-off, albeit via a different screening tool to that used in our study. Comparison between these estimates and ours may reflect a greater risk of common mental disorders among those refugees living in a camp setting, compared to those living in an urban setting among the host population, as with our sample. Additionally, the study in Islahiye camp was conducted in 2012, just one year after the start of the war in Syria, and the study in Syrian schools was conducted in 2015. In contrast, 75% of children in our 2019 study had been away from Syria for at least 4 years, and the difference in PTSD estimates may indicate that children with more recent exposure to the war and associated trauma are at a higher risk of symptoms of PTSD.
Our study identified a number of risk and protective factors associated with common mental disorders among Syrian children in Istanbul. Children with symptomatic depression in our sample were more likely to come from poorer households, consistent with evidence on the social determinants of mental health among the general and refugee populations (Porter and Haslam, Reference Porter and Haslam2005; Allen et al., Reference Allen, Balfour, Bell and Marmot2014; Hynie, Reference Hynie2018).
Symptoms of depression were also more common in children who had not attended school. School is crucial to a child's integration and acculturation in the host community, providing children with a place in which to develop relationships and a sense of belonging. Evidence indicates that the social support structures provided by a school offer protection against common mental disorders (Fazel and Stein, Reference Fazel and Stein2002), although the mechanism of this among Syrian children in Istanbul merits further investigation.
Similar structures may explain our finding that children from households with a larger number of household members were significantly less likely to demonstrate symptoms of PTSD. Social support is a strong protective factor for common mental disorders (Marley and Mauki, Reference Marley and Mauki2018), and children from larger households may receive more stable social support, shielding them against symptoms of PTSD. This is consistent with the ‘Intervention Pyramid’ proposed in the Inter-Agency Standing Committee Guidelines on Mental Health and Psychosocial Support in Emergency Settings, which highlights the need for strengthened community and family supports for those affected by situations of emergency, displacement and conflict (Inter-Agency Standing Committee, 2007).
As was expected, symptomatic depression was inversely associated with resilience scores, consistent with Panter-Brick et al.'s study among Syrian youth (Panter-Brick et al., Reference Panter-Brick, Hadfield, Dajani, Eggerman, Ager and Ungar2018). This association was not, however, observed for symptoms of anxiety or PTSD, despite support from the literature on the role of resilience as a protective factor against the onset of these disorders (Charney, Reference Charney2003). Further exploration is required in the interaction of resilience with social factors among Syrian children living in Istanbul.
Important to consider among our findings is the higher prevalence of common mental disorders in girls (27.7%) compared to boys (18.8%). This is consistent with research from across refugee and general populations, in which girls are reported to have a higher prevalence of depression and suicidal ideation/attempts than boys (Afifi, Reference Afifi2007; Mohwinkel et al., Reference Mohwinkel, Nowak, Kasper and Razum2018). Gender differences in anxiety and PTSD are less well defined, but apparent in some studies (Van Droogenbroeck et al., Reference Van Droogenbroeck, Spruyt and Keppens2018). This includes our study, in which girls (13.2%) demonstrated a significantly higher prevalence of symptomatic anxiety compared to boys (4.8%).
Evidence suggests that girls are more likely to exhibit ‘internationalising’ behaviours (withdrawal, self-consciousness and hypersensitivity), as opposed to ‘externalising’ behaviours (aggression, non-compliance and impaired self-regulation) in boys, particularly in adolescence (Liu et al., Reference Liu, Chen and Lewis2011). Males and females also exhibit differences in help-seeking, coping strategies and preferences for treatment (Liddon et al., Reference Liddon, Kingerlee and Barry2018). These are important considerations for future prevention and intervention strategies for this population.
Limitations
This was the first population-based survey of common mental disorders in Syrian refugee children living among the host community in Istanbul. Survey teams visited participants in their households, which may have contributed to the higher response rate than a previous study of adult mental health in the same district (Fuhr et al., Reference Fuhr, Ataturk, Mcgrath, Ilkkursun, Woodward, Sondorp and Roberts2019).
However, there were some limitations. Firstly, the sample was selected from the Sultanbeyli municipality's refugee registration database, which does not include information of unregistered or undocumented refugees, who may have a higher prevalence of common mental disorders. We sought to address this to some extent by including all eligible Syrians within a household, regardless of legal refugee status, but this cannot account for those unregistered households who would have been missed during the first stages of sampling.
Second, the response rate was slightly lower than 80%, although age and sex distribution were largely congruent with the registration database.
Third, all efforts were made to interview participants in private, but this was not always possible, as interviews were conducted in the child's home and caregivers had the right to be present. This may have resulted in response bias, especially with the sensitive nature of questions on mental health. Arguably, considering the stigma often attached to mental health, this may have resulted in underestimates of common mental disorders. The number of participants interviewed in the presence of caregivers was not recorded, which would have aided further analysis.
Fourth, a clinical diagnostic interview would have resulted in more precise prevalence estimates, but this was not feasible within a population survey. Self-report mental health screening tools can result in overestimated prevalence figures, although this is an issue common to nearly all other studies (Thombs et al., Reference Thombs, Kwakkenbos, Levis and Benedetti2018).
Finally, we used abbreviated versions of tools used to assess symptoms of depression and anxiety. The tools and cut-offs for these abbreviated versions have been validated with Syrian children living in refugee camps in Lebanon, as opposed to children living among a host population, as is the case in Sultanbeyli (Mcewen et al., Reference Mcewen, Moghames, Bosqui, Kyrillos, Chehade, Saad, Abdul Rahman, Popham, Saab, Karam, Karam and Pluess2020). These validated cut-offs may be higher than needed for children in Sultanbeyli, as children living in camps may be more likely to endorse certain items, given more challenging living conditions. As such, our estimates for symptomatic depression and anxiety in children may represent an under-estimate. Similarly, the tool used to assess symptoms of PTSD has been validated among Arabic speaking and refugee populations, but not among Syrians specifically.
Conclusion
We have presented findings of the first population-based study to report on the estimated prevalence of symptomatic depression, anxiety and PTSD among Syrian children and adolescents living in Istanbul, Turkey. Nearly 25% of participants demonstrated symptoms of at least one common mental disorder. The estimates of this study are considerably higher than in the general population and represent a substantial burden of these common mental disorders in this population. With high estimates of common mental disorders among Syrian children in Istanbul, it is important to support mental health intervention and prevention policies and programmes for this group.
Data
For more information on the data supporting the findings of this study, please contact Nathaniel Scherer: nathaniel.scherer@lshtm.ac.uk
Acknowledgements
We would firstly like to thank the study participants who generously gave their time to take part in the study. We also thank researchers at Queen Mary University of London (QMUL), the Institute for Development, Research, Advocacy and Applied Care (IDRAAC), Balamand University Medical School, St George's University Medical Center, Médecins du Monde (France) in Lebanon (MdM), and the American University of Beirut (AUB) for supporting us to use the abbreviated mental health screening tools used in this study. Thank you also to the wider team at Mülteciler Derneği and Relief International who provided support to the team and project. Finally, we are grateful for the team of enumerators and volunteers for their work, commitment and dedication to this study: Abdul Hadi Nashed, Abdulrahman Mohamed Zain, Afaf Elhaggan, Ahed Mansour, Al Shayma Khaled Al Jaseem, Diana Rahima, Ibrahim Dello, Lena Haddadin, Maria Altabba, Maryam Alsaid, Mohamad Amer Al Atassi, Muhamad Adib Alhaj Ibrahim, Nawar Aljasem, Sara Albadr, Sara Ashraf Mohamed, Shahed Aljassem, Yaman Hamwi, Muhammet Eyad Sahloul, Mohamad Yahya, Rukayye Esved, Mohammed Jundi, Melisa Ozakman. Electronic data solutions were provided by LSHTM Open Research Kits (odk.lshtm.ac.uk).
Author contributions
NS, SP and SH were responsible for study design and conceptualisation, methodology and data collection. NS managed in-country data collection. CA, GD, AS, SV, AO, AP, IP and IA were instrumental in sourcing funding, study conceptualisation, methodology and data collection. SP analysed the data, with support from NS. NS wrote the first draft of the manuscript and all authors contributed to subsequent drafts and the final version.
Financial support
This research was funded by a grant from the United States Department of State to Relief International. The opinions, findings and conclusions stated herein are those of the author[s] and do not necessarily reflect those of the United States Department of State.
Conflict of interest
None declared.
Ethical standards
Ethics approval was obtained from the London School of Hygiene & Tropical Medicine Research Ethics Committee (Ref: 17623), Istanbul Sehir University (Ref: 26/2019) and Republic of Turkey Ministry of Interior: Directorate General of Migration Management (Ref: 72104824000/72304). All participants were under the age of 18, and parent or caregiver consent was obtained for each participant. Verbal assent was sought from the participant themselves using a simplified information sheet.
Appendix 1
Visual aid for use with SCARED measurement tool (the versions used in the study were in Arabic)










