Abstract
Purpose
Although some studies have been conducted to examine general psychosocial impairment in Iran, there is no research to date on clinical impairment secondary to disordered eating in Iranian adolescents. The purpose of this study was to evaluate the Farsi version of the Clinical Impairment Assessment (F-CIA) among Iranian adolescents.
Methods
A total of 1112 adolescents (ageM [SD] = 15.55 [1.59], body mass index [zBMI] M [SD] = – 0.00 [1.0]; 54.6% girls) were recruited from four cities (Tehran [Capital], Tabriz [North-Western], Kurdistan [West], and Rasht [North]) in Iran. After translation and back-translation procedures, the F-CIA, Eating Disorder Examination Questionnaire (EDE-Q), and Beck Depression Inventory-Second Edition (BDI-II) were administered to adolescents. We used confirmatory factor analysis (CFA), measurement invariance, independent samples t tests, Pearson correlation, chi-square tests, and internal consistency to test validity and reliability.
Results
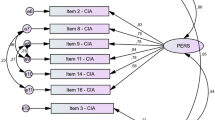
CFA indicated that F-CIA demonstrated good fit to the data and supported a three-factor model. The scale was invariant across gender and zBMI. The F-CIA had good internal consistency (αs = 0.76–0.93) and positive associations (rs = 0.13–0.62; p < 0.001) with zBMI, disordered eating symptoms, and binge/purge symptoms. We found no gender differences across mean scores on the F-CIA, but adolescents with higher zBMI reported higher scores on the F-CIA relative to those with lower zBMIs. Finally, adolescents scoring above CIA cutoffs reported higher zBMI, disordered eating outcomes, and depression.
Conclusion
Findings suggested that the F-CIA is a reliable and valid measure of clinical eating disorder-related impairment in Iranian adolescents.
Level of evidence
III; Evidence obtained from well-designed observational study, including case–control design for relevant aspects of the study.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the first author.
References
Nasser M, Katzman M, Gordon R (2001) Eating disorders and cultures in transition. Routledge
Pike KM, Hoek HW, Dunne PE (2014) Cultural trends and eating disorders. Curr Opin Psychiatry 27(6):436–442. https://doi.org/10.1097/YCO.0000000000000100
Smink FR, van Hoeken D, Hoek HW (2012) Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep 14(4):406–414. https://doi.org/10.1007/s11920-012-0282-y
Nobakht M, Dezhkam M (2000) An epidemiological study of eating disorders in Iran. Int J Eat Disord 28(3):265–271. https://doi.org/10.1002/1098-108x(200011)28:3%3c265::aid-eat3%3e3.0.co;2-l
Mohammadi MR, Mostafavi S-A, Hooshyari Z, Khaleghi A, Ahmadi N, Molavi P et al (2020) Prevalence, correlates and comorbidities of feeding and eating disorders in a nationally representative sample of Iranian children and adolescents. Int J Eat Disord 53(3):349–361. https://doi.org/10.1002/eat.23197
Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR (2011) Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry 68(7):714–723. https://doi.org/10.1001/archgenpsychiatry.2011.22
Sahlan RN, Saunders JF, Mond JM, Fitzsimmons-Craft EE (2021) Eating disorder symptoms among adolescent boys and girls in Iran. Int J Eat Disord 54(1):19–23. https://doi.org/10.1002/eat.23420
Sahlan RN, Taravatrooy F, Quick V, Mond JM (2020) Eating-disordered behavior among male and female college students in Iran. Eat Behav 37:101378. https://doi.org/10.1016/j.eatbeh.2020.101378
Sahlan RN, Saunders JF, Perez M, Blomquist KK, Fitzsimmons-Craft EE, Bodell LP (2021) The validation of a Farsi version of the Loss of Control over Eating Scale (F-LOCES) among Iranian adolescent boys and girls. Eat Behav 29(41):101502. https://doi.org/10.1016/j.eatbeh.2021.101502
Sahlan RN, Williams BM, Forrest LN, Saunders JF, Fitzsimmons-Craft EE, Levinson CA (2021) Disordered eating, self-esteem, and depression symptoms in Iranian adolescents and young adults: A network analysis. Int J Eat Disord 54(2):132–147. https://doi.org/10.1002/eat.23365
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Author, Washington, DC
Bohn K, Doll HA, Cooper Z, O’Connor M, Palmer RL, Fairburn CG (2008) The measurement of impairment due to eating disorder psychopathology. Behav Res Ther 46(10):1105–1110. https://doi.org/10.1016/j.brat.2008.06.012
Udo T, Grilo CM (2018) Prevalence and correlates of DSM-5-defined eating disorders in a nationally representative sample of U.S. adults. Biol Psychiatry 84(5):345–354. https://doi.org/10.1016/j.biopsych.2018.03.014
Bodell LP, Cheng Y, Wildes JE (2019) Psychological impairment as a predictor of suicide ideation in individuals with anorexia nervosa. Suicide Life Threat Behav 49(2):520–528. https://doi.org/10.1111/sltb.12459
Fairburn CG (2008) Cognitive behavior therapy and eating disorders. Guilford Press, New York
Spoor ST, Stice E, Burton E, Bohon C (2007) Relations of bulimic symptom frequency and intensity to psychosocial impairment and health care utilization: results from a community-recruited sample. Int J Eat Disord 40(6):505–514. https://doi.org/10.1002/eat.20410
Jalali-Farahani S, Chin YS, Mohd Nasir MT, Amiri P (2015) Disordered eating and its association with overweight and health-related quality of life among adolescents in selected high schools of Tehran. Child Psychiatry Hum Dev 46(3):485–492. https://doi.org/10.1007/s10578-014-0489-8
Tehrani M, Pourabbasi A (2020) Eating behaviors vs. BMI: which is more related with health-related quality of life? A cross-sectional study on Iranian female adolescents. Int J Sch Health 7(1):1–5. https://doi.org/10.30476/intjsh.2020.83598.1019
Ravens-Sieberer U, Erhart M, Rajmil L, Herdman M, Auquier P, Bruil J et al (2010) Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Qual Life Res 19(10):1487–1500. https://doi.org/10.1007/s11136-010-9706-5
Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: Reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39(8):800–812. https://doi.org/10.1097/00005650-200108000-00006
Vannucci A, Kass AE, Sinton MM, Aspen V, Weisman H, Bailey JO et al (2012) An examination of the Clinical Impairment Assessment among women at high risk for eating disorder onset. Behav Res Ther 50(6):407–414. https://doi.org/10.1016/j.brat.2012.02.009
Becker AE, Thomas JJ, Bainivualiku A, Richards L, Navara K, Roberts AL et al (2010) Adaptation and evaluation of the Clinical Impairment Assessment to assess disordered eating related distress in an adolescent female ethnic Fijian population. Int J Eat Disord 43(2):179–186. https://doi.org/10.1002/eat.20665
Horie T, Hiraide M, Takakura S, Hata T, Sudo N, Yoshiuchi K (2020) Development of a new Japanese version of the Clinical Impairment Assessment Questionnaire. Biopsychosoc Med 14(1):1–6. https://doi.org/10.1186/s13030-020-00194-8
Calugi S, Sartirana M, Milanese C, El Ghoch M, Riolfi F, Dalle Grave R (2018) The Clinical Impairment Assessment Questionnaire: validation in Italian patients with eating disorders. Eat Weight Disord 23(5):685–694. https://doi.org/10.1007/s40519-018-0477-2
Reas DL, Ro O, Kapstad H, Lask B (2010) Psychometric properties of the Clinical Impairment Assessment: norms for young adult women. Int J Eat Disord 43(1):72–76. https://doi.org/10.1002/eat.20653
Vaz AR, Conceicao E, Pinto-Bastos A, Silva D, Machado PPP (2019) Validation of the Portuguese version of the Clinical Impairment Assessment (CIA) in eating disorders’ patients. Eat Weight Disord. https://doi.org/10.1007/s40519-019-00661-4
Ng KW, Kuek A, Lee HY (2018) Eating psychopathology and psychosocial impairment in patients treated at a Singapore eating disorders treatment programme. Singap Med J 59(1):33–38. https://doi.org/10.11622/smedj.2017042
Martin J, Padierna A, Unzurrunzaga A, Gonzalez N, Berjano B, Quintana JM (2015) Adaptation and validation of the Spanish version of the Clinical Impairment Assessment Questionnaire. Appetite 91:20–27. https://doi.org/10.1016/j.appet.2015.03.031
Welch E, Birgegard A, Parling T, Ghaderi A (2011) Eating Disorder Examination Questionnaire and Clinical Impairment Assessment Questionnaire: general population and clinical norms for young adult women in Sweden. Behav Res Ther 49(2):85–91. https://doi.org/10.1016/j.brat.2010.10.010
Jenkins PE (2013) Psychometric validation of the Clinical Impairment Assessment in a UK eating disorder service. Eat Behav 14(2):241–243. https://doi.org/10.1016/j.eatbeh.2012.12.001
Raykos B, Erceg-Hurn D, McEvoy P, Byrne SM (2019) Evidence that the Clinical Impairment Assessment (CIA) subscales should not be scored: Bifactor modelling, reliability, and validity in clinical and community samples. Assessment 26(7):1260–1269. https://doi.org/10.1177/1073191117733546
Mahmoodi M, Moloodi R, Ghaderi A, Babai Z, Saleh Z, Alasti H et al (2016) The Persian version of Eating Disorder Examination Questionnaire and Clinical Impairment Assessment: Norms and psychometric properties for undergraduate women. Iran J Psychiatry 11(2):67–74 (PMID: 27437002; PMCID: PMC4947222)
Jalali-Farahani S, Alamdari S, Karimi M, Amiri P (2016) Is overweight associated with health-related quality of life (HRQoL) among Tehranian school children? Springerplus 5:313. https://doi.org/10.1186/s40064-016-1930-1
World Health Organization (2007) Growth reference 5–19 years: BMI-for-age (5–19 years). Peжим дocтyпy: http://www.whoint/growthref/who2007_bmi_for_age/en. Accessed 10 Jan 2021
Fairburn CG, Beglin SJ (2008) Eating Disorder Examination Questionnaire (EDE-Q 6.0). In: Fairburn CG (ed) Cognitive behavior therapy and eating disorders. Guilford Press, New York
Carter JC, Stewart DA, Fairburn CG (2001) Eating Disorder Examination Questionnaire: norms for young adolescent girls. Behav Res Ther 9(5):625–632. https://doi.org/10.1016/s0005-7967(00)00033-4
Mond J, Hall A, Bentley C, Harrison C, Gratwick-Sarll K, Lewis V (2014) Eating-disordered behavior in adolescent boys: Eating Disorder Examination Questionnaire norms. Int J Eat Disord 47(4):335–341. https://doi.org/10.1002/eat.22237
White HJ, Haycraft E, Goodwin H, Meyer C (2014) Eating Disorder Examination Qestionnaire: Factor structure for adolescent girls and boys. Int J Eat Disord 47(1):99–104. https://doi.org/10.1002/eat.22199
Beck AT, Steer R (1987) Manual for the revised Beck Depression Inventory. Psychological Corporation, San Antonio
Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N (2005) Psychometric properties of a Persian-language version of the Beck Depression Inventory—second edition: BDI-II-Persian. Depress Anxiety 21(4):185–192. https://doi.org/10.1002/da.20070
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J 6(1):1–55. https://doi.org/10.1080/10705519909540118
Kline RB (2015) Principles and practice of structural equation modeling. Guilford Publications, New York
van de Schoot R, Lugtig P, Hox J (2012) A checklist for testing measurement invariance. Eur J Dev Psychol 9(4):486–492. https://doi.org/10.1080/17405629.2012.686740
Schaefer LM, Smith KE, Leonard R, Wetterneck C, Smith B, Farrell N et al (2018) Identifying a male clinical cutoff on the Eating Disorder Examination-Questionnaire (EDE-Q). Int J Eat Disord 51(12):1357–1360. https://doi.org/10.1002/eat.22972
Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJ (2004) Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther 42(5):551–567. https://doi.org/10.1016/s0005-7967(03)00161-x
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. L. Erlbaum Associates, Mahwah, New Jersey
Lavender JM, De Young KP, Anderson DA (2010) Eating Disorder Examination Questionnaire (EDE-Q): Norms for undergraduate men. Eat Behav 11(2):119–121. https://doi.org/10.1016/j.eatbeh.2009.09.005
Mond JM, Hay PJ, Rodgers B, Owen C (2006) Eating Disorder Examination Questionnaire (EDE-Q): Norms for young adult women. Behav Res Ther 44(1):53–62. https://doi.org/10.1016/j.brat.2004.12.003
Quick VM, Byrd-Bredbenner C (2013) Eating Disorders Examination Questionnaire (EDE-Q): norms for US college students. Eat Weight Disord 18(1):29–35. https://doi.org/10.1007/s40519-013-0015-1
Kraemer HC, Kupfer DJ (2006) Size of treatment effects and their importance to clinical research and practice. Biol Psychiatry 59(11):990–996. https://doi.org/10.1016/j.biopsych.2005.09.014
Cheung GW, Rensvold RB (2002) Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model Multidiscip J 9(2):233–255. https://doi.org/10.1207/S15328007SEM0902_5
George D, Mallery P (2003) SPSS for Windows step by step: A simple guide and reference, 11.0 update. Allyn and Bacon, Boston
Milfont TL, Fischer R (2010) Testing measurement invariance across groups: applications in cross-cultural research. Int J Psychol Res 3(1):111–130. https://doi.org/10.21500/20112084.857
Dahlgren CL, Stedal K, Ro O (2017) Eating Disorder Examination Questionnaire (EDE-Q) and Clinical Impairment Assessment (CIA): Clinical norms and functional impairment in male and female adults with eating disorders. Nord J Psychiatry 71(4):256–261. https://doi.org/10.1080/08039488.2016.1271452
Sahlan RN, Saunders JF, Fitzsimmons-Craft EE (2021) Body-, eating-, and exercise-related social comparison behavior and disordered eating in college women in the U.S. and Iran: a cross-cultural comparison. Eat Behav 40:101451. https://doi.org/10.1016/j.eatbeh.2020.101451
Acknowledgements
We thank the adolescents who participated in the study, the teachers and principals of the schools.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study attained Institutional Review Board approval and complied with all ethical guidelines by the Iran University of Medical Sciences.
Human and animal rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participant included in the study.
What is already known on this subject?
Few measures of generic (non-ED specific) quality of life measures have been officially validated in Iran to this end. The Farsi translation and validation of the CIA in the current study enable researchers and clinicians in Iran to assess clinical impairment secondary to EDs.
What this study adds?
The F-CIA was supported in the original 3-factor structure with 16 items among adolescents. Additionally, F-CIA was invariant across gender and zBMI status, suggesting that the scale would be compared across those groups. Furthermore, concurrent and discriminant validity, as well as internal consistency reliability of the F-CIA were supported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sahlan, R.N., Saunders, J.F., Perez, M. et al. The validation of a Farsi version of the Clinical Impairment Assessment (F-CIA) among Iranian adolescent boys and girls. Eat Weight Disord 27, 665–674 (2022). https://doi.org/10.1007/s40519-021-01204-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-021-01204-6