Abstract
Purpose
The aim of this narrative review of the literature was to evaluate and summarize the current literature regarding the effect of lipedema on health-related quality of life (HRQOL) and psychological status.
Methods
The authors collected articles through a search into Medline, Embase, Scopus, Web of Science, Physiotherapy Evidence Database (PEDro), and the Cochrane Review. Search terms used included “Lipoedema,” “Lipedema,” “psychological status,” “Quality of life,” “Health related quality of life,” and “HRQOL.”
Results
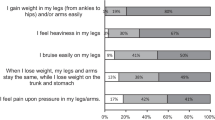
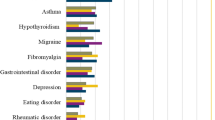
A total of four observational studies were evaluated. The included studies were moderate-quality according to the Newcastle–Ottawa Scale. Three of the included studies demonstrated deterioration of HRQOL and psychological status in patients with lipedema. These studies also identify that pain and tenderness are a more common and dominant characteristic.
Conclusion
Future studies should establish a specific approach to treat and manage lipedema symptoms. Based on this narrative review of the literature findings, we recommended for the health care provider to pay more attention to HRQOL and psychological status. Moreover, validated and adapted measures of HRQOL and psychological status for patients with lipedema are required.
Level of evidence
Level V, narrative review.
Similar content being viewed by others

References
Fonder MA, Loveless JW, Lazarus GS (2007) Lipedema, a frequently unrecognized problem. J Am Acad Dermatol 57:S1–S3. https://doi.org/10.1016/j.jaad.2006.09.023
Forner-Cordero I, Szolnoky G, Forner-Cordero A, Kemény L (2012) Lipedema: an overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome—systematic review. Clin obes 2:86–95. https://doi.org/10.1111/j.1758-8111.2012.00045.x
Schmeller W, Meier-Vollrath I (2005) Lipödem: Ein update. LymphForsch 9:10–20
Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS (2010) Lipedema: an inherited condition. Am J Med Genet A 152:970–976. https://doi.org/10.1002/ajmg.a.33313
De Lorenzo A, Soldati L, Sarlo F, Calvani M, Di Lorenzo N, Di Renzo L (2016) New obesity classification criteria as a tool for bariatric surgery indication. World J Gastroenterol 22:681. https://doi.org/10.3748/wjg.v22.i2.681
De Lorenzo A, Nardi A, Iacopino L, Domino E, Murdolo G, Gavrila C, Minella D, Scapagnini G, Di Renzo L (2014) A new predictive equation for evaluating women body fat percentage and obesity-related cardiovascular disease risk. J Endocrinol Investig 37:511–524. https://doi.org/10.1007/s40618-017-0806-8
Fife CE, Maus EA, Carter MJ (2010) Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care 23:81–92. https://doi.org/10.1097/01.ASW.0000363503.92360.91
Mayes JS, Watson GH (2004) Direct effects of sex steroid hormones on adipose tissues and obesity. Obes Rev 5:197–216. https://doi.org/10.1111/j.1467-789X.2004.00152.x
Gavin KM, Cooper EE, Hickner RC (2013) Estrogen receptor protein content is different in abdominal than gluteal subcutaneous adipose tissue of overweight-to-obese premenopausal women. Metabolism 62:1180–1188. https://doi.org/10.1016/j.metabol.2013.02.010
Schingale FJ (2003) Lymphoedema lipoedema. Schlütersche GmbH, Hannover, pp 20–21
Fife CE, Maus EA, Carter MJ (2010) Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv Skin Wound Care 23:81–92. https://doi.org/10.1097/01.ASW.0000363503.92360.91
Herbst KL (2012) Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacol Sin 33:155. https://doi.org/10.1038/aps.2011.153
Langendoen SI, Habbema L, Nijsten TEC, Neumann HAM (2009) Lipoedema: from clinical presentation to therapy. A review of the literature. Br J Dermatol 161:980–986. https://doi.org/10.1111/j.1365-2133.2009.09413.x
Seo CA (2014) You mean it's not my fault learning about lipedema a fat disorder. Narrat Inq Bioeth 4:E6–E9. https://doi.org/10.1353/nib.2014.0045
Bosman J (2011) Lipoedema poor knowledge neglect or disinterest? J Lymphoedema 6:109–111
Skevington SM, Lotfy M, O'Connell K (2004) The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual Life Res 13:299–310. https://doi.org/10.1023/B:QURE.0000018486.91360.00
Dadras M, Mallinger PJ, Corterier CC, Theodosiadi S, Ghods M (2017) Liposuction in the treatment of lipedema a longitudinal study. Arch Plast Surg 44:324. https://doi.org/10.5999/aps.2017.44.4.324
Schmeller W, Meier-Vollrath I (2006) Tumescent liposuction a new and successful therapy for lipedema. J Cutan Med Surg 10:7–10. https://doi.org/10.1007/7140.2006.00006
Schneider R (2018) Low-frequency vibrotherapy considerably improves the effectiveness of manual lymphatic drainage (MLD) in patients with lipedema: a two-armed randomized controlled pragmatic trial. Physiother Theory Pract. https://doi.org/10.1080/09593985.2018.1479474
Rapprich S, Dingler A, Podda M (2011) Liposuction: is an effective treatment for lipedema—results of a study with 25 patients. J Dtsch Dermatol Ges 9:33–40. https://doi.org/10.1111/j.1610-0387.2010.07504.x
Wells G (2004) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. https://www.ohri.ca/programs/clinical_epidemiology.oxford.htm. Accessed 6 Mar 2019
Dudek JE, Białaszek W, Ostaszewski P (2016) Quality of life in women with lipoedema: a contextual behavioral approach. Qual Life Res 25:401–408. https://doi.org/10.1007/s11136-015-1080-x
Romeijn JR, de Rooij MJ, Janssen L, Martens H (2018) Exploration of patient characteristics and quality of life in patients with lipoedema using a survey. Dermatol Ther 1:1–9. https://doi.org/10.1007/s13555-018-0241-6
Dudek JE, Białaszek W, Ostaszewski P, Smidt T (2018) Depression and appearance-related distress in functioning with lipedema. Psychol Health Med 23:846–853. https://doi.org/10.1080/13548506.2018.1459750
Blome C, Augustin M, Heyer K, Knöfel J, Cornelsen H, Purwins S, Herberger K (2014) Evaluation of patient-relevant outcomes of lymphedema and lipedema treatment: development and validation of a new benefit tool. Eur J Vasc Endovasc Surg 47:100–107. https://doi.org/10.1016/j.ejvs.2013.10.009
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33:350–357. https://doi.org/10.3109/07853890109002089
Hays RD, Morales LS (2001) The RAND-36 measure of health-related quality of life. Ann Med 33:350–357
GroupTE (1990) EuroQol—a new facility for the measurement of health-related quality of life. Health Policy 16:199–208. https://doi.org/10.1016/0168-8510(90)90421-9
Whoqol Group (1995) The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med 41:1403–1409. https://doi.org/10.1016/0277-9536(95)00112-K
Abdallah CG, Geha P (2017) Chronic pain and chronic stress: two sides of the same coin? Chronic Stress. https://doi.org/10.1177/2470547017704763
Petroni ML, Villanova N, Avagnina S, Fusco MA, Fatati G, Compare A, QUOVADIS Study Group (2007) Psychological distress in morbid obesity in relation to weight history. Obes Surg 17:391–399. https://doi.org/10.1007/s11695-007-9069-3
Nath R (2019) The injustice of fat stigma. Bioethics. https://doi.org/10.1111/bioe.12560
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alwardat, N., Di Renzo, L., Alwardat, M. et al. The effect of lipedema on health-related quality of life and psychological status: a narrative review of the literature. Eat Weight Disord 25, 851–856 (2020). https://doi.org/10.1007/s40519-019-00703-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00703-x