Abstract
Objectives
Assessments of health-related quality of life outcomes associated with preterm birth provide valuable complementary data to the objective biomedical assessments that have traditionally been reported. The objective of this study was to perform a systematic review and meta-analysis of health utility values associated with preterm birth generated using preference-based approaches to health-related quality of life measurement.
Methods
Systematic searches of MEDLINE, Web of Science, EconLit, EMBASE, CINAHL, PsycINFO, the Cochrane Library and SCOPUS were performed, covering the literature from inception of the search engines to 26 June 2018. Studies reporting health utility values estimated using either direct or indirect utility elicitation methods and published in the English language were included. Central descriptive statistics and measures of variability surrounding health utility values for each study and control group, and differences between comparator groups, are reported for each included article. The effect of preterm birth on health utility values was estimated using a hierarchical linear model in a linear mixed-effects meta-regression.
Results
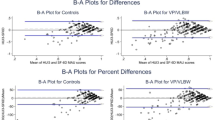
Of 2139 unique articles retrieved, 20 articles met the inclusion criteria. All but one study used the Health Utilities Index (HUI) Mark 2 (HUI2) or Mark 3 (HUI3) measures as their primary health utility assessment method. All studies reporting health utility values for individuals born preterm or at low birthweight and a control group of individuals born at full term or normal birthweight reported lower utility values in the study groups, regardless of age at assessment, respondent type or valuation method. The meta-regression revealed that preterm birth was associated with a mean utility decrement of 0.066 (95% confidence interval [CI] 0.035–0.098; p < 0.001) after controlling for valuation method, respondent type, administration mode, year of publication, geographical region of study, study setting and age at assessment.
Conclusion
Evidence identified by this review can act as data inputs into future economic evaluations of preventive or treatment interventions for preterm birth. Future research should focus particularly on estimating health utility values during the various stages of adulthood, and incorporating the effects of preterm birth on the preference-based health-related quality of life outcomes of parents and other family members.



Similar content being viewed by others
Data Availability Statement
The data generated or analysed during the current study are available from the corresponding author on reasonable request.
References
Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016;21(2):74–9. https://doi.org/10.1016/j.siny.2015.12.007.
Larroque B, Ancel PY, Marret S, Marchand L, Andre M, Arnaud C, et al. Neurodevelopmental disabilities and special care of 5-year-old children born before 33 weeks of gestation (the EPIPAGE study): a longitudinal cohort study. Lancet. 2008;371(9615):813–20. https://doi.org/10.1016/S0140-6736(08)60380-3.
Moore T, Hennessy EM, Myles J, Johnson SJ, Draper ES, Costeloe KL, et al. Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ. 2012;345:e7961. https://doi.org/10.1136/bmj.e7961.
Serenius F, Kallen K, Blennow M, Ewald U, Fellman V, Holmstrom G, et al. Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA. 2013;309(17):1810–20. https://doi.org/10.1001/jama.2013.3786.
Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR. Neurologic and developmental disability after extremely preterm birth. EPICure Study Group. N Engl J Med. 2000;343(6):378–84. https://doi.org/10.1056/NEJM200008103430601.
Johnson S, Wolke D. Behavioural outcomes and psychopathology during adolescence. Early Hum Dev. 2013;89(4):199–207. https://doi.org/10.1016/j.earlhumdev.2013.01.014.
Petrou S, Yiu HH, Kwon J. Economic consequences of preterm birth: a systematic review of the recent literature (2009–2017). Arch Dis Child. 2019;104(5):456–65. https://doi.org/10.1136/archdischild-2018-315778.
Horvath H, Brindis CD, Reyes EM, Yamey G, Franck L, Knowledge T, et al. Preterm birth: the role of knowledge transfer and exchange. Health Res Policy Syst. 2017;15(1):78. https://doi.org/10.1186/s12961-017-0238-0.
Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371(9608):261–9. https://doi.org/10.1016/S0140-6736(08)60136-1.
Zwicker JG, Harris SR. Quality of life of formerly preterm and very low birth weight infants from preschool age to adulthood: a systematic review. Pediatrics. 2008;121(2):e366–76. https://doi.org/10.1542/peds.2007-0169.
Torrance GW, Feeny D. Utilities and quality-adjusted life years. Int J Technol Assess Health Care. 1989;5(4):559–75.
Arnold D, Girling A, Stevens A, Lilford R. Comparison of direct and indirect methods of estimating health state utilities for resource allocation: review and empirical analysis. BMJ. 2009;339:b2688. https://doi.org/10.1136/bmj.b2688.
Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53–72. https://doi.org/10.1016/0168-8510(96)00822-6.
Feeny D, Furlong W, Boyle M, Torrance GW. Multi-attribute health status classification systems. Health Utilities Index. Pharmacoecon. 1995;7(6):490–502.
Brazier J, Ratcliffe J, Salomon J, Tsuchiya A. Measuring and valuing health benefits for economic evaluation. Oxford: Oxford University Press; 2007.
National Institute for Health and Care Excellence (NICE). Guide to the methods of technology appraisal 2013. London: NICE; 2013.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
Papaioannou D, Brazier J, Paisley S. Systematic searching and selection of health state utility values from the literature. Value Health. 2013;16(4):686–95. https://doi.org/10.1016/j.jval.2013.02.017.
Petrou S, Kwon J, Madan J. A practical guide to conducting a systematic review and meta-analysis of health state utility values. Pharmacoeconomics. 2018;36(9):1043–61. https://doi.org/10.1007/s40273-018-0670-1.
Canadian Agency for Drugs and Technologies in Health (CADTH). Guidelines for the economic evaluation of health technologies. 4th ed. Ottawa: CADTH; 2017.
Baumann N, Bartmann P, Wolke D. Health-related quality of life into adulthood after very preterm birth. Pediatrics. 2016;137:4. https://doi.org/10.1542/peds.2015-3148.
Feeny D, Furlong W, Saigal S, Sun J. Comparing directly measured standard gamble scores to HUI2 and HUI3 utility scores: group- and individual-level comparisons. Soc Sci Med. 2004;58(4):799–809.
Gray R, Petrou S, Hockley C, Gardner F. Self-reported health status and health-related quality of life of teenagers who were born before 29 weeks’ gestational age. Pediatrics. 2007;120(1):e86–93. https://doi.org/10.1542/peds.2006-2034.
Hille ET, Weisglas-Kuperus N, van Goudoever JB, Jacobusse GW, Ens-Dokkum MH, de Groot L, et al. Functional outcomes and participation in young adulthood for very preterm and very low birth weight infants: the Dutch Project on Preterm and Small for Gestational Age Infants at 19 years of age. Pediatrics. 2007;120(3):e587–95. https://doi.org/10.1542/peds.2006-2407.
James JD. Health status and psychological adjustment in low birth weight and normal birth weight Jamaican preadolescents. Evanston: Northwestern University; 2003.
Petrou S, Abangma G, Johnson S, Wolke D, Marlow N. Costs and health utilities associated with extremely preterm birth: evidence from the EPICure study. Value Health. 2009;12(8):1124–34. https://doi.org/10.1111/j.1524-4733.2009.00580.x.
Quinn GE, Dobson V, Saigal S, Phelps DL, Hardy RJ, Tung B, et al. Health-related quality of life at age 10 years in very low-birth-weight children with and without threshold retinopathy of prematurity. Arch Ophthalmol. 2004;122(11):1659–66. https://doi.org/10.1001/archopht.122.11.1659.
Rautava L, Hakkinen U, Korvenranta E, Andersson S, Gissler M, Hallman M, et al. Health-related quality of life in 5-year-old very low birth weight infants. J Pediatr. 2009;155(3):338–43 e1–3. https://doi.org/10.1016/j.jpeds.2009.03.061.
Roberts G, Anderson PJ, Cheong J, Doyle LW, Victorian Infant Collaborative Study Group. Parent-reported health in extremely preterm and extremely low-birthweight children at age 8 years compared with comparison children born at term. Dev Med Child Neurol. 2011;53(10):927–32. https://doi.org/10.1111/j.1469-8749.2011.04025.x.
Roberts G, Burnett AC, Lee KJ, Cheong J, Wood SJ, Anderson PJ, et al. Quality of life at age 18 years after extremely preterm birth in the post-surfactant era. J Pediatr. 2013;163(4):1008–1013e1. https://doi.org/10.1016/j.jpeds.2013.05.048.
Saigal S, Feeny D, Furlong W, Rosenbaum P, Burrows E, Torrance G. Comparison of the health-related quality of life of extremely low birth weight children and a reference group of children at age eight years. J Pediatr. 1994;125(3):418–25.
Saigal S, Feeny D, Rosenbaum P, Furlong W, Burrows E, Stoskopf B. Self-perceived health status and health-related quality of life of extremely low-birth-weight infants at adolescence. JAMA. 1996;276(6):453–9.
Saigal S, Ferro MA, Van Lieshout RJ, Schmidt LA, Morrison KM, Boyle MH. Health-related quality of life trajectories of extremely low birth weight survivors into adulthood. J Pediatr. 2016;179(68–73):e1. https://doi.org/10.1016/j.jpeds.2016.08.018.
Saigal S, Rosenbaum PL, Feeny D, Burrows E, Furlong W, Stoskopf BL, et al. Parental perspectives of the health status and health-related quality of life of teen-aged children who were extremely low birth weight and term controls. Pediatrics. 2000;105(3 Pt 1):569–74.
Saigal S, Stoskopf B, Pinelli J, Streiner D, Hoult L, Paneth N, et al. Self-perceived health-related quality of life of former extremely low birth weight infants at young adulthood. Pediatrics. 2006;118(3):1140–8. https://doi.org/10.1542/peds.2006-0119.
van Dommelen P, van der Pal SM, Bennebroek Gravenhorst J, Walther FJ, Wit JM, van der Pal de Bruin KM. The effect of early catch-up growth on health and well-being in young adults. Ann Nutr Metab. 2014;65(2–3):220–6. https://doi.org/10.1159/000364884.
van Lunenburg A, van der Pal SM, van Dommelen P, van der Pal-de Bruin KM, Bennebroek Gravenhorst J, Verrips GH. Changes in quality of life into adulthood after very preterm birth and/or very low birth weight in the Netherlands. Health Qual Life Outcomes. 2013;11:51. https://doi.org/10.1186/1477-7525-11-51.
Verrips E, Vogels T, Saigal S, Wolke D, Meyer R, Hoult L, et al. Health-related quality of life for extremely low birth weight adolescents in Canada, Germany, and the Netherlands. Pediatrics. 2008;122(3):556–61. https://doi.org/10.1542/peds.2007-1043.
Verrips G, Brouwer L, Vogels T, Taal E, Drossaert C, Feeny D, et al. Long term follow-up of health-related quality of life in young adults born very preterm or with a very low birth weight. Health Qual Life Outcomes. 2012;10:49. https://doi.org/10.1186/1477-7525-10-49.
Wolke D, Chernova J, Eryigit-Madzwamuse S, Samara M, Zwierzynska K, Petrou S. Self and parent perspectives on health-related quality of life of adolescents born very preterm. J Pediatr. 2013;163(4):1020. https://doi.org/10.1016/j.jpeds.2013.04.030.
McCormick MC, Litt JS. The outcomes of very preterm infants: is it time to ask different questions? Pediatrics. 2017;139(1):e20161694. https://doi.org/10.1542/peds.2016-1694.
Vieira ME, Linhares MB. Quality of life of individuals born preterm: a systematic review of assessment approaches. Qual Life Res. 2016;25(9):2123–39. https://doi.org/10.1007/s11136-016-1259-9.
Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med. 2001;33(5):344–9.
Marra CA, Woolcott JC, Kopec JA, Shojania K, Offer R, Brazier JE, et al. A comparison of generic, indirect utility measures (the HUI2, HUI3, SF-6D, and the EQ-5D) and disease-specific instruments (the RAQoL and the HAQ) in rheumatoid arthritis. Soc Sci Med. 2005;60(7):1571–82. https://doi.org/10.1016/j.socscimed.2004.08.034.
Kwon J, Kim SW, Ungar WJ, Tsiplova K, Madan J, Petrou S. A systematic review and meta-analysis of childhood health utilities. Med Decis Making. 2018;38(3):277–305. https://doi.org/10.1177/0272989X17732990.
Eiser C, Morse R. Quality-of-life measures in chronic diseases of childhood. Health Technol Assess. 2001;5(4):1–157.
McCabe C, Stevens K, Roberts J, Brazier J. Health state values for the HUI 2 descriptive system: results from a UK survey. Health Econ. 2005;14(3):231–44. https://doi.org/10.1002/hec.925.
Lakshmanan A, Agni M, Lieu T, Fleegler E, Kipke M, Friedlich PS, et al. The impact of preterm birth < 37 weeks on parents and families: a cross-sectional study in the 2 years after discharge from the neonatal intensive care unit. Health Qual Life Outcomes. 2017;15(1):38. https://doi.org/10.1186/s12955-017-0602-3.
Wolke D, Baumann N, Busch B, Bartmann P. Very preterm birth and parents’ quality of life 27 years later. Pediatrics. 2017;140(3):e20171263. https://doi.org/10.1542/peds.2017-1263.
Honest H, Forbes CA, Duree KH, Norman G, Duffy SB, Tsourapas A, et al. Screening to prevent spontaneous preterm birth: systematic reviews of accuracy and effectiveness literature with economic modelling. Health Technol Assess. 2009;13(43):1–627. https://doi.org/10.3310/hta13430.
McCurdy RJ, Baxter JK. Universal cervical length screening with a cervicometer to prevent preterm birth < 34 weeks: a decision and economic analysis. J Matern Fetal Neonatal Med. Epub. 2019. https://doi.org/10.1080/14767058.2019.1583202.
Werner EF, Hamel MS, Orzechowski K, Berghella V, Thung SF. Cost-effectiveness of transvaginal ultrasound cervical length screening in singletons without a prior preterm birth: an update. Am J Obstet Gynecol. 2015;213(4):554.e1–6. https://doi.org/10.1016/j.ajog.2015.06.020.
Moya MP, Goldberg RN. Cost-effectiveness of prophylactic indomethacin in very-low-birth-weight infants. Ann Pharmacother. 2002;36(2):218–24. https://doi.org/10.1345/aph.10347.
Acknowledgements
We would like to thank Samantha Johnson for her assistance with the development and piloting of the literature search strategies. We would also like to thank colleagues at the University of Warwick for comments on earlier drafts of the paper.
Funding
SP receives support as an NIHR (National Institute for Health Research) Senior Investigator (NF-SI-0616-10103). SP also receives funding from the European Union’s 2020 research and innovation programme, Research on European Children and Adults born Preterm (RECAP), under grant agreement number 733280. The views contained within this paper are those of the authors and not necessarily of the funders.
Author information
Authors and Affiliations
Contributions
SP designed the study, extracted and reviewed the evidence from all contributing studies, wrote the article and acts as guarantor. NK and KK performed the literature searches and screened all titles and abstracts and full-text articles. NK also extracted data from all full-text articles. All authors read and approved the final version of the article. SP is the guarantor of the overall content.
Corresponding author
Ethics declarations
Conflict of interest
SP, NK and KK have no conflicts of interest.
Ethics approval
Ethics approval was not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Petrou, S., Krabuanrat, N. & Khan, K. Preference-Based Health-Related Quality of Life Outcomes Associated with Preterm Birth: A Systematic Review and Meta-analysis. PharmacoEconomics 38, 357–373 (2020). https://doi.org/10.1007/s40273-019-00865-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-019-00865-7