Abstract
Objective
Health utility decrements associated with diabetes mellitus complications are essential for calculating quality-adjusted life-years (QALYs) in patients for use in economic evaluation of diabetes interventions. Previous studies mostly focused on assessing the impact of complications on health utility at event year based on cross-sectional data. This study aimed to separately estimate health utility decrements associated with current and previous diabetes complications.
Research Design and Methods
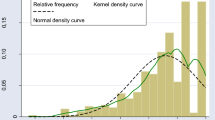
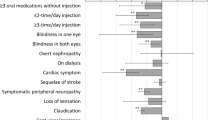
The Health Utilities Index Mark 3 (HUI-3) was used to measure heath utility in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial (N = 8713). Five macrovascular complications (myocardial infarction [MI], congestive heart failure [CHF], stroke, angina, and revascularization surgery [RS]) and three microvascular complications (nephropathy [renal failure], retinopathy [severe vision loss], and neuropathy [severe pressure sensation loss]) were included in a set of alternative modelling approaches including the ordinary least squares (OLS) model, fixed effects model, and random effects model to estimate the complication-related health utility decrements.
Results
All macrovascular complications were associated with decrements of HUI-3 scores: MI (event year: − 0.042, successive years: − 0.011), CHF (event year: − 0.089, successive years: − 0.041), stroke (event year: − 0.204, successive years: − 0.101), angina (event year: − 0.010, successive years: − 0.032), and revascularization (event year: − 0.038, successive years: − 0.016) (all p < 0.05). For microvascular complications, severe vision loss (− 0.057), and severe pressure sensation loss (− 0.066) were significantly associated with decrements of HUI-3 scores (both p < 0.05). Hypoglycemia (both severe and symptomatic) was found to be associated with a 0.036 decrement of health utility at event year, and a 0.033 decrement of health utility at successive years. Results from an OLS model are preferred for supporting a microsimulation model while a fixed effects model is preferred to describe direct health impacts from complications.
Conclusions
Macrovascular and microvascular complications caused QALY decrements in patients with type 2 diabetes. While only part of the total impaired QALY is experienced during the event year, further QALY decrements for successive years were quite substantial.
Similar content being viewed by others
References
Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96:5–21.
Fanshel S, Bush JW. A health-status index and its application to health-services outcomes. Oper Res. 1970;18:1021–66.
Torrance GW, Thomas WH, Sackett DL. A utility maximization model for evaluation of health care programs. Health Serv Res. 1972;7:118.
Weinstein MC, Stason WB. Foundations of cost-effectiveness analysis for health and medical practices. N Engl J Med. 1977;296:716–21.
Rawlins MD, Culyer AJ. National Institute for Clinical Excellence and its value judgments. BMJ 2004;329:224.
Gold MR. Cost-effectiveness in health and medicine. Oxford: Oxford University Press; 1996.
Sassi F. Calculating QALYs, comparing QALY and DALY calculations. Health policy and planning. 2006;21:402–8.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Hoch JS, Dewa CS. An introduction to economic evaluation: what’s in a name? Can J Psychiatry. 2005;50:159–66.
Karnon J. Heath state utility values for cost-effectiveness models. PharmacoEconomics. 2017;35:1–3.
Weinstein MC, Torrance G, McGuire A. QALYs: the basics. Value Health. 2009;12:S5–9.
Nord E, Daniels N, Kamlet M. QALYs: some challenges. Value Health. 2009;12:S10–5.
Kind P, Lafata JE, Matuszewski K, Raisch D. The use of QALYs in clinical and patient decision-making: issues and prospects. Value Health. 2009;12:S27–30.
Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–108.
Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S, Denton M, Boyle M. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40:113–28.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–92.
DeWalt DA, Rothrock N, Yount S, Stone AA. Evaluation of item candidates: the PROMIS qualitative item review. Med Care. 2007;45:S12.
Ara R, Brazier J. Estimating health state utility values for comorbidities. PharmacoEconomics. 2017;35:89–94.
Coffey JT, Brandle M, Zhou H, Marriott D, Burke R, Tabaei BP, Engelgau MM, Kaplan RM, Herman WH. Valuing health-related quality of life in diabetes. Diabetes Care. 2002;25:2238–43.
Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Mak. 2002;22:340–9.
Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–63.
Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ. 2005;14:217–30.
Glasziou P, Alexander J, Beller E, Clarke P. Which health-related quality of life score? A comparison of alternative utility measures in patients with Type 2 diabetes in the ADVANCE trial. Health Qual Life Outcomes. 2007;5:21.
Zhang P, Brown MB, Bilik D, Ackermann RT, Li R, Herman WH. Health utility scores for people with type 2 diabetes in US managed care health plans. Diabetes Care. 2012;35:2250–6.
Lung TW, Hayes AJ, Hayen A, Farmer A, Clarke PM. A meta-analysis of health state valuations for people with diabetes: explaining the variation across methods and implications for economic evaluation. Qual Life Res. 2011;20:1669–78.
Venkataraman K, Wee H, Leow M, Tai E, Lee J, Lim S, Tavintharan S, Wong T, Ma S, Heng D. Associations between complications and health-related quality of life in individuals with diabetes. Clin Endocrinol. 2013;78:865–73.
Alva M, Gray A, Mihaylova B, Clarke P. The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ. 2014;23:487–500.
Hayes A, Arima H, Woodward M, Chalmers J, Poulter N, Hamet P, Clarke P. Changes in quality of life associated with complications of diabetes: results from the ADVANCE study. Value Health. 2016;19:36–41.
Zhang P, Brown MB, Bilik D, Ackermann RT, Li R, Herman WH. Health utility scores for people with type 2 diabetes in US managed care health plans: results from Translating Research Into Action for Diabetes (TRIAD). Diabetes Care. 2012;35:2250–6.
Pesantes MA, Brandt LR, Ipince A, Miranda JJ, Diez-Canseco F. An exploration into caring for a stroke-survivor in Lima, Peru: emotional impact, stress factors, coping mechanisms and unmet needs of informal caregivers. eNeurologicalSci. 2017;6:33–50.
Lewis EF, Li Y, Pfeffer MA, Solomon SD, Weinfurt KP, Velazquez EJ, Califf RM, Rouleau J-L, Kober L, White HD. Impact of cardiovascular events on change in quality of life and utilities in patients after myocardial infarction: a VALIANT study (valsartan in acute myocardial infarction). JACC: Heart Fail. 2014;2:159–165.
Buse JB, Group AS. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol. 2007;99:S21–33.
Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH, Hamilton BP, Hoogwerf B, Karl D, Katz L, Krikorian A, O’Connor P, Pop-Busui R, Schubart U, Simmons D, Taylor H, Thomas A, Weiss D, Hramiak I. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376:419–30.
Kingry C, Bastien A, Booth G, Geraci TS, Kirpach BR, Lovato LC, Margolis KL, Rosenberg Y, Sperl-Hillen JM, Vargo L. Recruitment strategies in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007;99:S68–79.
Baser OH, Li L, Wang L. Obese patients in the veteran population in the united states: a health care cost and utilization analysis. Value Health. 2013;16(3):A110.
Sullivan MD, Anderson RT, Aron D, Atkinson HH, Bastien A, Chen GJ, Feeney P, Gafni A, Hwang W, Katz LA, Venkat Narayan KM, Nwachuku C, O’Connor PJ, Zhang P. Health-related quality of life and cost-effectiveness components of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Trial: rationale and design. Am J Cardiol. 2007;99:S90–102.
Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:54.
Palmer AJ, Roze S, Valentine WJ, Minshall ME, Foos V, Lurati FM, Lammert M, Spinas GA. The CORE Diabetes Model: projecting long-term clinical outcomes, costs and costeffectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20:S5–26.
RTI Press. Validation of the CDC-RTI diabetes cost-effectiveness model [article online]. 2009. Available from https://www.rti.org/. Accessed 15 May 2018.
Shi L, Shao H, Zhao Y, Thomas NA. Is hypoglycemia fear independently associated with health-related quality of life? Health Qual Life Outcomes. 2014;12:167.
Luo N, Johnson JA, Shaw JW, Feeny D, Coons SJ. Self-reported health status of the general adult U.S. population as assessed by the EQ-5D and Health Utilities Index. Med Care. 2005;43:1078–86.
Johnson JA, Coons SJ, Ergo A, Szava-Kovats G. Valuation of EuroQOL (EQ-5D) health states in an adult US sample. Pharmacoeconomics. 1998;13:421–33.
Johnson JA, Luo N, Shaw JW, Kind P, Coons SJ. Valuations of EQ-5D health states: are the United States and United Kingdom different? Med Care. 2005;43:221–8.
Action to Control Cardiovascular Risk in Diabetes (ACCORD) data [article online]. Available from https://biolincc.nhlbi.nih.gov/studies/accord/. Accessed 15 Ma 2018.
Acknowledgements
Hui Shao researched the data and wrote the first draft of the manuscript. Shuang Yang analyzed the data. Vivian Fonseca provided knowledge from the physician’s perspective. Charles Stoecker helped with interpreting the statistical results. Lizheng Shi designed the study and managed the project flow. All authors contributed to the discussion and reviewed/edited the manuscript. Dr. Hui Shao is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
All authors, including Hui Shao, Shuang Yang, Vivian Fonseca, Charles Stoecker, and Lizheng Shi disclosed no conflict of interests.
Data availability statement
The datasets used for this study are publicly available and can be accessed through the National Heart, Lung, and Blood Institute [44].
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shao, H., Yang, S., Fonseca, V. et al. Estimating Quality of Life Decrements Due to Diabetes Complications in the United States: The Health Utility Index (HUI) Diabetes Complication Equation. PharmacoEconomics 37, 921–929 (2019). https://doi.org/10.1007/s40273-019-00775-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-019-00775-8