Abstract
Background
In the UK, two treatment options are used for acute epileptic seizures in the community—rectal diazepam and unlicensed buccal midazolam. In practice, the former is rarely used, with unlicensed buccal midazolam being widely recommended and prescribed by physicians. In September 2011, Buccolam® (licensed midazolam oromucosal solution) became the first medicine to receive a Paediatric-Use Marketing Authorization (PUMA) and it is indicated for the treatment of prolonged, acute, convulsive seizures by caregivers in the community for children (aged 6 months to <18 years) diagnosed with epilepsy. The approval process for a PUMA product differs from other marketing authorization processes and may be based upon small population subsets and may not, in some cases, require new safety or efficacy data to be generated; a similar situation to that seen for orphan drugs. This can lead to challenges when conducting economic evaluations.
Objective
The aim of this study was to assess the cost effectiveness of Buccolam® for children with a diagnosis of epilepsy suffering prolonged, acute, convulsive seizures occurring in the UK community setting.
Design and Perspective
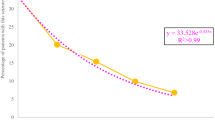
A hybrid model was developed according to a UK payer perspective. The model included a time-to-event simulation for the frequency and location of occurrence of seizures, along with a decision-tree model that assessed the treatment pathway when a seizure occured. The model compared treatment with Buccolam® with standard care in the community (95 % unlicensed buccal midazolam and 5 % rectal diazepam) or either treatment alone. The model was informed by data from a variety of sources, including clinical effectiveness estimates, and costs based on published UK data, using 2012–13 prices, where possible. To determine current practice and real-world effectiveness, a Delphi panel and a survey of parents of children with epilepsy were conducted.
Results
Buccolam® showed a reduction in costs of £2,939 compared with standard care, £14,269 compared with rectal diazepam alone and £886 compared with unlicensed buccal midazolam alone. Increases of 0.025, 0.082 and 0.013 quality-adjusted life-years, respectively, were also seen. Buccolam® remained dominant across a range of scenario analyses.
Conclusion
This model demonstrates the possibility of constructing a thorough economic case when trial or real-world data are not available. The results of the model show Buccolam® to be cost saving compared with rectal diazepam due to a reduction in the need for ambulance callouts and hospital stays, and compared with unlicensed buccal midazolam, through reduced drug costs and wastage.




Similar content being viewed by others
References
European Medicines Agency. Buccolam® 2.5 mg oromucosal solution: summary of product characteristics [online]. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002267/WC500112310.pdf. Accessed 30 Aug 2012.
Chin RF, Neville BG, Peckham C, Bedford H, Wade A, Scott RC. Incidence, cause, and short-term outcome of convulsive status epilepticus in childhood: prospective population-based study. Lancet. 2006;368(9531):222–9.
Raspall-Chaure M, Chin RF, Neville BGR, Scott RC. Outcome of paediatric convulsive status epilepticus: a systematic review. Lancet Neurol. 2006;5(9):769–79.
Forsgren L, Beghi E, Oun A, Sillanpaa M. The epidemiology of epilepsy in Europe: a systematic review. Eur J Neurol. 2005;12(4):245–53.
SEIN, WHO Collaborating Centre for Research, Training and Treatment in Epilepsy, WHO headquarters, ILAE/IBE/WHO Global Campaign Against Epilepsy. Epilepsy in the WHO European region: fostering epilepsy care in Europe [online]. http://www.ibe-epilepsy.org/downloads/EUROReport160510.pdf. Accessed 30 Aug 2012.
World Health Organization. Epilepsy fact sheet No 999 (01/2009) [online]. http://www.who.int/mediacentre/factsheets/fs999/en/index.html. Accessed 15 Aug 2012.
Joint Epilepsy Council. Epilepsy prevalence, incidence and other statistics [online]. http://www.epilepsyscotland.org.uk/pdf/Joint_Epilepsy_Council_Prevalence_and_Incidence_September_11_(3).pdf (2011). Accessed 30 Aug 2012.
Pellock JM. Overview: definitions and classifications of seizure emergencies. J Child Neurol. 2007;22(5 suppl):9S–13S.
Klimach VJ; Epic Clinical Network. The community use of rescue medication for prolonged epileptic seizures in children. Seizure. 2009;18(5):343–6.
Scott RC, Besag MF, Neville BG. Buccal midazolam and rectal diazepam for treatment of prolonged seizures in childhood and adolescence: a randomised trial. Lancet. 1999;353(9153):623–6.
Camfield CS, Camfield PR, Smith E, Dooley JM. Home use of rectal diazepam to prevent status epilepticus in children with convulsive disorders. J Child Neurol. 1989;4(2):125–6.
O’Dell C, Shinnar S, Ballaban-Gil KR, et al. Rectal diazepam gel in the home management of seizures in children. Pediatr Neurol. 2005;33(3):166–72.
Delphi survey of the current clinical practice in Wales for the treatment of prolonged acute convulsive seizures in children and adolescents. Brussels: ViroPharma SPRL-BVBA; 2011 (Data on File).
Wilson MT, Macleod S, O’Regan ME. Nasal/buccal midazolam use in the community. Arch Dis Child. 2004;89(1):50–1.
Chattopadhyay A, Morris B, Blackburn L, et al. Buccal midazolam and rectal diazepam for epilepsy. Lancet. 1999;353(9166):1798.
Pharmaceutical Services Negotiating Committee. Unlicensed specials and imports FAQs [online]. http://www.psnc.org.uk/publications_detail.php/285/unlicensed_specials_and_imports_guidance (2011). Accessed 30 Aug 2012.
General Medical Council. Good Practice in Prescribing Medicines [online]. Available from URL: http://www.gmc-uk.org/guidance/ethical_guidance/prescriptions_faqs.asp (2008). Accessed 30 Aug 2012.
Scottish Medicines Consortium. Midazolam, 5 mg/mL oromucosal solution (Buccolam®) SMC No. (757/12): ViroPharma Ltd [online]. http://www.scottishmedicines.org.uk/SMC_Advice/Advice/757_12_midazolam_Buccolam_oromucosal_solution/midazolam_Buccolam_oromucosal_solution (2012). Accessed 24 Jan 2013.
All Wales Medicine Strategy Group (2012). Final Appraisal Recommendation Advice No: 0912. Midazolam (BUCCOLAM®). Submission by ViroPharma Ltd [online]. http://www.wales.nhs.uk/sites3/Documents/371/midazolam%20(Buccolam)%20FAR%20(W).pdf (2012). Accessed 30 Aug 2012.
McIntyre J, Robertson S, Norris E, et al. Safety and efficacy of buccal midazolam versus rectal diazepam for emergency treatment of seizures in children: a randomised controlled trial. Lancet. 2005;366(9481):205–10.
Mpimbaza A, Ndeezi G, Staedke S, et al. Comparison of buccal midazolam with rectal diazepam in the treatment of prolonged seizures in Ugandan children: a randomized clinical trial. Pediatrics. 2008;121(1):e58–64.
McMullan J, Sasson C, Pancioli A, Silbergleit R. Midazolam versus diazepam for the treatment of status epilepticus in children and young adults: a meta-analysis. Acad Emerg Med. 2010;17(6):575–82.
Patient Survey Wales: Epilepsy rescue medication and your child. ViroPharma SPRL-BVBA; 2011 (Data on File).
Chin RF, Neville BG, Peckham C, et al. Treatment of community-onset, childhood convulsive status epilepticus: a prospective, population-based study. Lancet Neurol. 2008;7(3):696–703.
NHS Business Services Authority. Electronic drug tariff [online]. http://www.ppa.org.uk/edt/January_2013/mindex.htm. Accessed 24 Jan 2013.
Joint Formulary Committee. British National Formulary 64 [online]. http://www.medicinescomplete.com/mc/bnf/current/ (2011). Accessed 24 Jan 2013.
Department of Health. NHS Reference Costs 2011–2012 [online]. http://www.dh.gov.uk/health/2012/11/2011-12-reference-costs/. Accessed 24 Jan 2013.
Strzelczyk A, Nickolay T, Bauer S, Haag A, Knake S, Oertel WH et al. Evaluation of health-care utilization among adult patients with epilepsy in Germany. Epilepsy Behav. 2012;23(4):451–7.
Acknowledgments
This study was funded by ViroPharma SPRL-BVBA. ViroPharma is the manufacturer of Buccolam® (midazolam oromucosal solution). The authors independently conducted all analyses and wrote the manuscript. The decision to submit the manuscript for publication was made by the authors. Dawn Lee, Daniel Gladwell, Anthony Batty and Nic Brereton are employees of BresMed. Elaine Tate was an employee of Hayward Medical Communications when the study was carried out. The study was designed by Dawn Lee, Anthony Batty, Nic Brereton and Elaine Tate. The methods were implemented by Dawn Lee, Daniel Gladwell and Anthony Batty. Dawn Lee, Daniel Gladwell, Anthony Batty, Nic Brereton and Elaine Tate participated in the review and interpretation of the data analysis. The manuscript was written by Dawn Lee and Daniel Gladwell, and reviewed by Anthony Batty, Nic Brereton and Elaine Tate. Dawn Lee is the guarantor for the overall content of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, D., Gladwell, D., Batty, A.J. et al. The Cost Effectiveness of Licensed Oromucosal Midazolam (Buccolam®) for the Treatment of Children Experiencing Acute Epileptic Seizures: An Approach When Trial Evidence is Limited. Pediatr Drugs 15, 151–162 (2013). https://doi.org/10.1007/s40272-013-0009-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-013-0009-5