Abstract
Introduction
Capturing the patient experience during treatment is important to both regulatory authorities and to patients starting treatment. We identified the symptoms and side effects experienced by patients with advanced non-small-cell lung cancer during osimertinib treatment, to understand treatment expectations, satisfaction, and the level of difficulty coping with the side effects experienced during treatment.
Methods
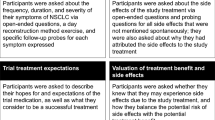
Qualitative interviews (approximately 4–6 weeks after treatment initiation and again after approximately 4 months of treatment) were conducted during the phase I/II AURA clinical trial of osimertinib, a tyrosine kinase inhibitor of epidermal growth factor receptor-sensitizing and T790M resistance mutations.
Results
During the first interview (23 patients), the most commonly reported symptoms/side effects were coughing, itching, tiredness (each reported by 56.5% of patients), and rash (43.5%). During the second interview (21 patients), compared with the first interview, shortness of breath and diarrhea were reported by more patients (57.1 and 38.1%, respectively; both increased from 34.8%); tiredness remained predominant (42.9%); and itching (38.1%), coughing (38.1%), and rash (14.3%) were reported by fewer patients. At both interviews, the most frequently reported symptoms/side effects were also those most often rated by patients for bothersomeness and severity, and generally received mean scores in the low-to-moderate range. However, several rarely expressed symptoms/side effects (e.g., abdominal pain, frequent day time urination) received high bothersomeness ratings. At the second interview, patients were highly satisfied with osimertinib and had a low level of difficulty in coping with side effects during treatment.
Conclusions
These data enhance our understanding of patients’ experiences of symptoms/side effects, which could increase the accuracy of the osimertinib benefit–risk assessment, guide management of adverse events, and improve the information given to patients receiving the drug.

Similar content being viewed by others
References
Basch E, Reeve BB, Mitchell SA, Clauser SB, Minasian LM, Dueck AC, et al. Development of the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). J Natl Cancer Inst. 2014;106(9).
Basch E. The missing voice of patients in drug-safety reporting. N Engl J Med. 2010;362(10):865–9.
Fromme EK, Eilers KM, Mori M, Hsieh YC, Beer TM. How accurate is clinician reporting of chemotherapy adverse effects? A comparison with patient-reported symptoms from the Quality-of-Life Questionnaire C30. J Clin Oncol. 2004;22(17):3485–90.
Pakhomov SV, Jacobsen SJ, Chute CG, Roger VL. Agreement between patient-reported symptoms and their documentation in the medical record. Am J Manag Care. 2008;14(8):530–9.
FDA. Patient-reported outcome measures: use in medical product development to support labeling claims; 2009. http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM193282.pdf.
EMA. Reflection paper on the regulatory guidance for the use of health-related Quality of life (HRQL) measures in the evaluation of medicinal products; 2005. http://www.ispor.org/workpaper/emea-hrql-guidance.pdf.
EMA. Reflection paper on the use of patient reported outcome (PRO) measures in oncology studies; 2014. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/06/WC500168852.pdf.
Janne PA, Yang JC, Kim DW, Planchard D, Ohe Y, Ramalingam SS, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–99.
Ballard P, Yates JW, Yang Z, Kim DW, Yang JC, Cantarini M, et al. Preclinical comparison of osimertinib with other EGFR-TKIs in EGFR-mutant NSCLC brain metastases models, and early evidence of clinical brain metastases activity. Clin Cancer Res. 2016;22(20):5130–40.
Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–8.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46.
Kuiper JL, Heideman DA, Thunnissen E, Paul MA, van Wijk AW, Postmus PE, et al. Incidence of T790M mutation in (sequential) rebiopsies in EGFR-mutated NSCLC-patients. Lung Cancer. 2014;85(1):19–24.
Li W, Ren S, Li J, Li A, Fan L, Li X, et al. T790M mutation is associated with better efficacy of treatment beyond progression with EGFR-TKI in advanced NSCLC patients. Lung Cancer. 2014;84(3):295–300.
Yu HA, Arcila ME, Rekhtman N, Sima CS, Zakowski MF, Pao W, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–7.
FDA. FDA approves new pill to treat certain patients with non-small cell lung cancer; 2015. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm472525.htm.
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N Engl J Med. 2016;376:629–40.
Patrick DL, Burke LB, Gwaltney CJ, Leidy NK, Martin ML, Molsen E, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2—assessing respondent understanding. Value Health. 2011;14(8):978–88.
FDA. The voice of the patient; 2013 Public Meeting: June 28, 2013. Report Date: December 2013.
Remon J, Planchard D. AZD9291 in EGFR-mutant advanced non-small-cell lung cancer patients. Future Oncol. 2015;11(22):3069–81.
Acknowledgements
Anna Rydén took a lead in designing the study and in collecting, analyzing, and interpreting the data. Fiona Blackhall, Hye Ryun Kim, Rathi N. Pillai, Lauren Braam, Mona L. Martin, and Andrew Walding all had major roles in designing the study, and in collecting, analyzing, and interpreting the data. All authors have critically reviewed manuscript drafts and approved the final manuscript for publication.
Medical writing support (assistance in writing the manuscript under the direction of the authors from the study report) was provided by Dr. Nesta Hughes from Oxford PharmaGenesis, Oxford, UK, and was funded by AstraZeneca Gothenburg, Mölndal, Sweden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by AstraZeneca Gothenburg, Mölndal, Sweden.
Conflict of interest
The authors declare the following conflicts of interest: Anna Rydén and Andrew Walding are employees of AstraZeneca and hold shares in AstraZeneca. Lauren Braam and Mona L. Martin are employees of Health Research Associates, Inc., which has received funding from AstraZeneca to conduct the study. Fiona Blackhall has received grants from AstraZeneca, Pfizer, Boehringer-Ingelheim, Medivation, Novartis, MSD, and BMS, and has received consulting fees or honorarium from AstraZeneca, Pfizer, Boehringer-Ingelheim, Medivation, Novartis, MSD, and BMS. Hye Ryun Kim and Rathi N. Pillai have no conflicts to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Rights and permissions
About this article
Cite this article
Rydén, A., Blackhall, F., Kim, H.R. et al. Patient Experience of Symptoms and Side Effects when Treated with Osimertinib for Advanced Non-Small-Cell Lung Cancer: A Qualitative Interview Substudy. Patient 10, 593–603 (2017). https://doi.org/10.1007/s40271-017-0229-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-017-0229-9