Abstract
Background
Efficiency refers the use of resources in ways that optimise desired outcomes. Health system efficiency is a priority concern for policy makers globally as countries aim to achieve universal health coverage, and face the additional challenge of an aging population. Efficiency analysis in the health sector has typically focused on the efficiency of healthcare facilities (hospitals, primary healthcare facilities), with few studies focusing on system level (national or sub-national) efficiency. We carried out a thematic review of literature that assessed the efficiency of health systems at the national and sub-national level.
Methods
We conducted a systematic search of PubMed and Google scholar between 2000 and 2021 and a manual search of relevant papers selected from their reference lists. A total of 131 papers were included. We analysed and synthesised evidence from the selected papers using a thematic approach (selecting, sorting, coding and charting collected data according to identified key issues and themes).
Findings
There were more publications from high- and upper middle-income countries (53%) than from low-income and lower middle-income countries. There were also more publications focusing on national level (60%) compared to sub-national health systems’ efficiency. Only 6% of studies used either qualitative methods or mixed methods while 94% used quantitative approaches. Data envelopment analysis, a non-parametric method, was the most common methodological approach used, followed by stochastic frontier analysis, a parametric method. A range of regression methods were used to identify the determinants of health system efficiency. While studies used a range of inputs, these generally considered the building blocks of health systems, health risk factors, and social determinants of health. Outputs used in efficiency analysis could be classified as either intermediate health service outputs (e.g., number of health facility visits), single health outcomes (e.g., infant mortality rate) or composite indices of either intermediate outputs of health outcomes (e.g., Health Adjusted Life Expectancy). Factors that were found to affect health system efficiency include demographic and socio-economic characteristics of the population, macro-economic characteristics of the national and sub-national regions, population health and wellbeing, the governance and political characteristics of these regions, and health system characteristics.
Conclusion
This review highlights the limited evidence on health system efficiency, especially in low- and middle-income countries. It also reveals the dearth of efficiency studies that use mixed methods approaches by incorporating qualitative inquiry. The review offers insights on the drivers of the efficiency of national and sub-national health systems, and highlights potential targets for reforms to improve health system efficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Most papers used quantitative methods that focused on quantifying the level of efficiency and its determinants. Few papers used a qualitative approach and provided more information about how certain factors might affect health system efficiency, and also identified determinants of efficiency that are not easily quantifiable. |
System level efficiency is affected by factors both outside the health system and within the health system; these include demographic and socio-economic characteristics of the population, macro-economic characteristics of the national and sub-national regions, population health and wellbeing, the governance and political characteristics of these regions, and health system characteristics. |
1 Introduction
Health system efficiency is a priority concern for policy makers globally in the face of mounting health system expenditures [1,2,3]. Attainment of efficiency demonstrates good stewardship through good use of available resources and elimination of wastage [1, 4]. It also inspires the willingness of governments and citizens to contribute resources towards Universal Health Coverage (UHC) [4]. Improved efficiency is recognised as a desirable goal of the health system [5] and an intermediate objective of health-financing policies that contributes towards the attainment of health system goals [6]. It is also a major criterion for priority setting by decision makers [7]. Given the scarcity of healthcare resources, it is imperative that health systems, in both high income (HIC) and low- and middle-income countries (LMICs), orient their operations towards using their resources efficiently to optimise the achievement of stated health system goals and promote financial sustainability in the long-term towards UHC [3, 4].
Efficiency refers to the extent to which system objectives are met given the resources invested in the system [1]. Two types of efficiency, technical and allocative efficiency, have been distinguished [8]. Technical efficiency (TE) is achieved when resources are allocated such that outputs are maximised for a given level of inputs, or inputs are minimised for a given level of outputs [9]. Allocative efficiency (AE) is achieved when resources are allocated such that outputs are maximised for a given level of input cost, or input costs are minimised for a given level of outputs [9]. Allocative and technical efficiency together make the 'overall' efficiency of a system. Productivity, a concept related but different from efficiency, refers to the ratio of outputs to inputs in a production system [10]. This paper focuses on the efficiency of health systems rather than productivity.
It has been estimated that 20–40% of health system spending globally is wasted through inefficiency [11]. Such inefficiencies haemorrhage resources within the health sector and impede progress towards UHC [11]. While generating additional resources for health is crucial, improving the use of available resources in the health sector is argued by some as one of the a promising strategies towards expanding the fiscal space for health [11,12,13]. This is important both for LMICs that face constrained fiscal space as the support from donors reduces, and HICs as an aging population increases resource requirements in the health sector.
Efficiency measurement is therefore a key dimension of health system performance assessment. It requires the identification of the boundaries of the entity under scrutiny ranging from micro (provider-patient level) to meso (organisational) to macro (national or global) levels of the health system [4, 14]. The chosen level of analysis should reflect an entity that will take accountability for the level of performance identified by the analysis [4]. Efficiency is increasingly assessed in healthcare, but most of these studies analyse efficiency at the meso-level of the health system involving healthcare organisations (such as hospitals and health centres) [4, 10, 15], with fewer examining the national or subnational level [10].
Understanding efficiency within the health system and the associated inputs, outputs/outcomes and determinants of efficiency can influence policy formulation and managerial decision-making [4]. This literature review aims to synthesise existing empirical evidence on efficiency at the health system level (national and sub-national rather than health facility level) to increase the understanding of the conceptualisation and determinants of health system efficiency.
2 Methods
2.1 Literature Search Strategy
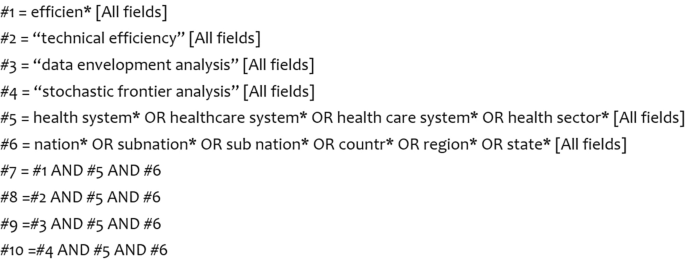
We followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [16] in the reporting of this literature review. We searched two electronic databases: PubMed and Google scholar for published and grey literature using specific subject headings and free text terms. We ran the searches separately for these databases. Search terms included ‘efficiency’, ‘technical efficiency’, ‘data envelopment analysis’, ‘stochastic frontier analysis’, ‘health system’, ‘health sector’, ‘nation’, ‘sub nation’, ‘country’, ‘region’ and ‘state’. These search terms were used as key words in google scholar. We developed a Boolean algorithm to search PubMed was developed (Fig. 1). The last literature search was done in December 2021.
2.2 Article Selection
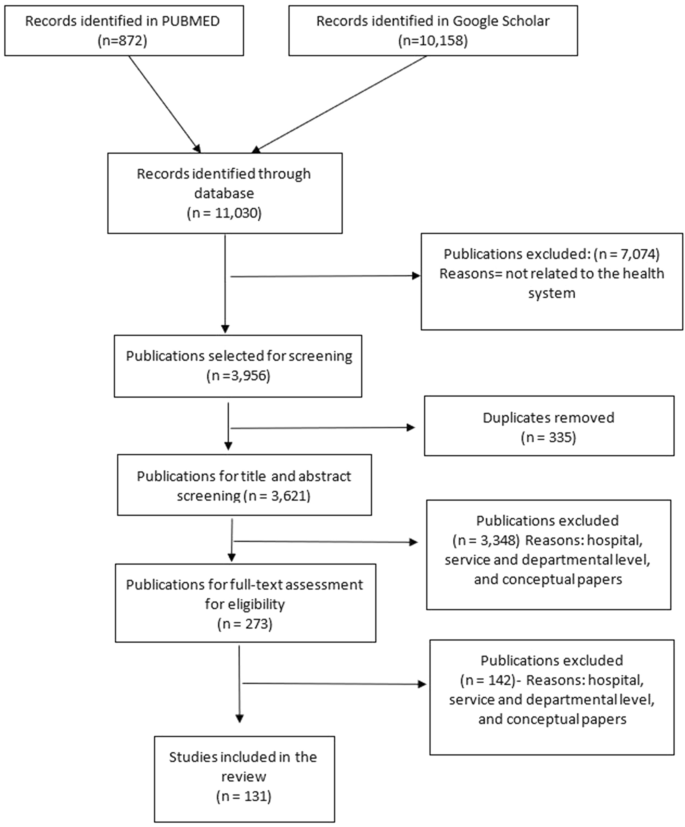
The electronic literature search identified 11,030 publications. Of these, 10,899 were rejected based on our eligibility criteria (Table 1). We retained 131 articles that met our inclusion criteria. We only included publications that met the inclusion criteria. We included publications that reported on empirical research on efficiency of health systems above the meso-level of the health system. We defined these levels to include jurisdictions such as sub national, national, regional and international health systems. We included publications that were published in English due to time and resource constraints that would otherwise be required for the translation of non-English publications. We did not use any restrictions on publication year, publication status, country income classification or study design. The publications that met the inclusion criteria were imported into EndNote X8. The article selection process is summarised in a search flow diagram in Fig. 2. A total of 131 publications were retrieved and reviewed.
2.3 Quality Appraisal
We used the critical appraisal skills programme (CASP) tool to assess the quality of the identified publications [17]. CASP tool uses a checklist approach to assess the adequacy, trustworthiness and relevance of the evidence reported in the publications [18, 19]. The CASP tool helps to reflect the character of the studies included in the review [17]. The results of the quality appraisal are indicated in Table 2. All the publications were of sufficient quality to be included in the review.
2.4 Data Extraction
Two authors (RM and EB) performed data extraction of the retrieved publications using a thematic analysis approach. Specifically, RM and EB first extracted data from a subset of selected papers (25/131). The data extracted by the two authors was compared to establish concurrence on the extraction approach. RB thereafter concluded data extraction of the remaining papers. Thematic analysis is an analytic process that involves a systematic process of sifting, sorting, coding and charting collected data according to key issues and themes [20]. The first step in this analysis process involved familiarisation with the publications through reading and re-reading. This formed the beginning of the abstraction process. We used a data extraction form structured (Additional File 2) in line with the review question and efficiency concepts. This form was used as a data registry and a guide for the identification of inputs, outputs and determinants of efficiency within the health system. Second, after familiarisation, we applied codes, developed inductively and deductively, to data that we interpreted as important and relevant. We then grouped similar codes into categories or themes drawing upon: (a) a priori issues (those informed by the original research aims and researchers’ knowledge in the subject area), (b) emergent categories identified by the authors in the retrieved literature, and lastly, (3) analytical themes arising from similarities across the identified codes. We then charted the data into a framework matrix using Microsoft Excel. This allowed us to: (1) summarise the data by category, (2) identify patterns and linkages in our data, that is, findings that were similar and recurrent across selected papers, and (3) make comparisons across the papers, to identified both converging and diverging findings and seek explanations for this.
3 Results
3.1 Characteristics of Selected Publications
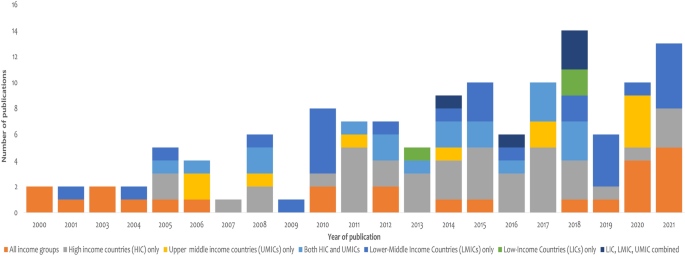
The list of the selected publications is provided in Online Supplementary Material, File 1. Empirical literature on health system efficiency has expanded noticeably over the years with the highest number of the retrieved literature published in 2018 (Fig. 3). However, most of these studies (53%) presented findings of health system efficiency in upper middle-income and high-income countries, while 25% of the studies focused exclusively on lower middle-income countries and low-income countries, and another 19% focused on countries across all income groups (Table 3).
Sixty percent of all the retrieved publications examined efficiency at the national/country level. These included studies that examined a single country health system or several country health systems such as OECD countries [21], World Health Organization member states [22], Eastern European countries [23], Asian countries [24, 25], Latin America and Caribbean countries [26] and Sub Saharan Africa [27]. Forty percent of the publications examined efficiency at sub national levels such as: (1) provinces in China [28, 29] and South Africa [30]; regions in Saudi Arabia [31] and Switzerland [32]; municipalities in Brazil [33] and Finland [34]; and districts in India [35], Zambia [36] and Mozambique [37].
3.2 Conceptualisation of Efficiency at Health System Level in the Retrieved Literature
Following existing production literature described by Farrell [8], the majority of the authors of the retrieved literature explicitly defined efficiency as the extent to which desired health system goals were achieved given existing resources [38,39,40,41]. The literature conceptualised a health system as a production system that transformed inputs into desired outputs [42]. In most of the studies, this production system was considered as a single unit. In two studies, however, the health system was perceived to be composed of two subunits—a public health system (non-health facility-based health promotion and prevention services) and a medical care system (i.e., healthcare facilities) that offered population-based and individual-based care, respectively [43, 44]. Both subunits contributed towards the efficiency of the overall health system [43]. In addition to inputs and outputs, the efficiency of the health system as a production “unit” was thought to be affected by contextual factors from within and outside of the health sector. These factors had different labels, including exogenous factors, explanatory factors, and determinants of efficiency.
3.3 Methods Used to Analyse Efficiency
Of the selected papers, 123 (94%) used purely quantitative approaches, five (4%) used purely qualitative approaches, and another three (2%) used mixed methods approaches. Quantitative approaches were used to measure the level and determinants of efficiency. Qualitative approaches were used to examine study participants’ perceptions about the objectives of the health system [41, 45] and existence and nature of health system inefficiency and its determinants [41, 45,46,47,48]. Beyond identification, qualitative approaches provided explanations of the relationship between identified determinants and health system efficiency [36, 48, 49]. Seventy-two (57%) of the publications that used pure quantitative approaches or mixed methods used cross-sectional quantitative data to estimate the level of efficiency in the health system. The remaining 54 (43%) of these papers used panel data with authors such as [27, 50, 51] indicating that panel data offer more accurate estimations of efficiency because of the richness of the data and consideration of the effect of time [52] precludes the need to impose assumptions on the error terms likely to be correlated with time. Of the papers that used panel data, 36 (67%) used the Malmquist productivity index (MPI) approach to measure efficiency changes over time, while 18 (33%) included time as a covariate in a regression analysis. Five publications (4%) employed qualitative approaches [36, 46, 53,54,55], while two studies (2%) used a mixed methods approach by combining both qualitative and quantitative methods [47, 49].
Efficiency measurement in the retrieved literature was done using non-parametric (data envelopment analysis-DEA and Free disposal hull technique) and parametric methods (stochastic frontier analysis-SFA). DEA was the most used technique for measuring efficiency. DEA is a non-parametric linear programming method that assess the relative efficiency of production units by obtaining the ratio of a weighted sum of the outputs of a productive unit to a weighted sum of its inputs [56]. The DEA technique is relevant in the health sector given the complex nature of health systems where multiple inputs are utilised to produce multiple outputs. A key limitation of DEA is that its results may be influenced by measurement error or statistical noise given that DEA is non-stochastic. DEA ascribes deviations from the frontier entirely to inefficiency, even though these may be due to measurement errors. DEA was exclusively used in 95 (76%) of the selected papers and used in combination and compared with free disposal hull (FDH) or SFA in two (2%) papers respectively. SFA was the second most common approach, used exclusively in 23 (18%) papers and in combination and compared to FDH in one (1%) paper. SFA is a parametric method that uses regression analysis to estimate the production frontier, measuring the efficiency of a unit using the residuals from the estimated equation [57]. Its key advantage over DEA is that SFA explicitly accounts for measurement error. The DEA model decomposes the error term in a stochastic error component and an additional error term that represents systematic inefficiency. SFA is used because it accounts for random disturbances in the data [58]. Qualitative data were analysed using thematic analysis [36].
Determinants of health systems efficiency were identified in 72 (55%) of the selected papers. Methods used for the quantitative identification of the determinants of efficiency include: Bayesian linear regression [59, 60], Tobit regression [60, 61], truncated regression model [62], and multiple regression analysis [63]. These methods were second stage analysis in DEA or SFA.
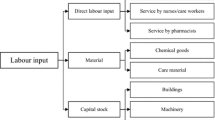
3.3.1 Inputs, Their Definition and Reasons Why They Were Chosen
Inputs were defined as resources required to facilitate the production function of the health system [21, 60]. These resources were considered to be within the control of the managers in the health system [33]. The list of inputs identified in the literature is provided in Table 4. While different studies used different inputs, the inputs could be classified into three broad categories: health system building blocks, social determinants of health, and health risk factors. Among the health system building blocks, finances were the most common input, with 68% of the studies using this variable in the production function. This was followed by human resources for health (66%) and medical equipment (54%). In some of the studies, the number of beds was used as a proxy for capital investment in health production [62, 64, 65] because direct measurement of capital in healthcare was found to be problematic [62]. The number of health facilities was only used in 22% of the studies. Education, a social determinant of health, was used as an input in 15% of the studies. Health risk factor characteristics used as inputs included tobacco and alcohol consumption (5%).
The choice of inputs used in assessing efficiency was informed by various reasons. These included evidence of use of the input variables in previous efficiency studies, availability of the data, positive relationship with the outputs, frequency of data reporting on the variable, direct involvement of the input in the production of health, input that would allow cross-country comparisons of efficiency or whether the input could be standardised across the system to allow comparison. It also included whether the input variable could be consistently measured across the units being assessed, whether the influence of the variable on efficiency was within the control of the health system, and based on economic theory and wider literature, and opinions of experts and stakeholders in the system.
3.3.2 Outputs and Outcomes, Their Definition and Reasons Why They Were Chosen
Outputs used in the reviewed literature fall into three categories: intermediate health service outputs, single health outcomes, or composite indices of either intermediate outputs or health outcomes. While several authors indicate that a general consensus in existing literature puts health status of the population [60] as the single most important output of the system [66], its measurement has, however, remained difficult [60]. As indicated by [23], the distinction between output and outcome is often blurred leading authors to use the two terms interchangeably.
The list of outputs and outcomes identified in the literature is provided in Table 5. Seventy percent of the publications included more than one output variable in their assessment of efficiency. Of the health outcome variable used, mortality rates and life expectancy were the most common (51%). Mortality rates were considered a good summary measure of overall population health [67] as well as the closest measurable indicator of the stated health system objectives [41]. Common intermediate health outputs used included outpatient and inpatient workload measures and maternal and child health services utilisation measures. Several studies used composite indices as output/outcome measures. For example Tandon et al. [68] used a weighted average of health system goals using disability adjusted life expectancy (DALE), health inequality, responsiveness level, responsiveness distribution and fair financing. Tandon et al. [69] created an outcome index by combining five indicators on immunisation coverage, skilled birth attendance, iodised salt content, catastrophic expenditure and life expectancy while Achoki et al. [70] use a composite metric for maternal and child health services made up of diphtheria, pertussis, tetanus vaccine-3 doses (DPT3) and measles immunisations, skilled birth attendance and malaria prevention.
The most common criterion that informed the choice of outputs used in a study was evidence of common use of the variable in previous studies [44, 60, 65, 71,72,73]. This was indicated in 40% of the retrieved literature. Other criteria applied to select outputs included: (1) use of the variable by the ministry of health to monitor efficiency of the health system, for example, the hospital bed occupancy rate in Zambia [36]. (2) Relevance to millennium development goals related to reduction of maternal mortality and child mortality such as institutional delivery rate [74] or under-5-year-old mortality rates. (3) Relevance to the national government priorities such as primary healthcare agenda in India [74] or increased number of live births in Thailand [75] or access to quality and effective healthcare in Canada [41]. (4) Availability of data [52, 76]. (5) Robustness of the indicators [77,78,79]. (6) Objectivity of the variables [80]. Relevance of the variable to the context [81]. (7) Routine collection of the data and its ability to allow for cross-unit comparison [66, 82].
3.3.3 Exogenous or Environmental Variables, Their Definition and Reasons Why They Were Chosen
Exogenous variables refer to the factors that are not directly related to the resources in the sector in question but may have an effect on the relationship between the inputs and outputs of that sector [69]. These variables are recognised as the third variable for inclusion in efficiency measurement along with inputs and outputs [68]. Exogenous variables were thought to capture heterogeneity and explain some of the differences or dispersion in the efficiency levels of units under analysis [39]. Fifty-six percent of the retrieved publications considered the influence of exogenous variables on the efficiency of the units under consideration. However, only one author [53] provided a conceptual framework that shows the influence of environmental variables on a health system’s production function. The list of these variables is provided in Table 6.
Exogenous variables were chosen based on: (1) evidence of use in previous studies [15, 21, 59, 77]; this was the most common reason given by a third of all the authors who used exogenous variables in their analysis. (2) Completeness and consistency of reporting of the variable in question for the units under consideration [72]. And lastly, (3) evidence of their potential influence on efficiency [33, 62, 65]. Table 6 outlines the categories of exogenous variables used in the analysis. It will be evident that some factors are used either as inputs or as exogenous variables in different studies.
3.4 Efficiency of Health Systems
It is challenging to summarise and/or compare findings from the literature on the efficiency of health systems because of heterogeneity of methods. This includes differences in approach (qualitative and quantitative), selection of inputs, outputs, exogenous variables, and models. For instance, a sensitivity analysis of an efficiency analysis of 141 countries originally conducted by the World Health Organization (WHO) found that country rankings and efficiency scores were sensitive to the definition of efficiency and choice of model specification [63]. Qualitative papers focused on health system stakeholders’ views about the existence of inefficiency and sources of inefficiency in health systems. These are summarised in the next section. Quantitative approaches reported the level of health system efficiency as a proportion (with a range of 0–100) or an inefficiency score. For example, the most recent regional analysis of the efficiency the country health systems reported a mean efficiency of 80% (range 31–100%) for 45 African countries [27], 92% (range 81–91%) for 46 Asian countries [83], 93% (range 51–93%) for 27 Latin American countries, and 83% (range 54–94%) for 28 European countries [84]. The most recent global analysis of the efficiency of 140 country health systems reported a mean efficiency of 93% (range 71–100%), with the following regional means: African countries (86%), Asian countries (95%) South American countries (95%), and European countries (96%) [85]. An efficiency score of 100% denotes an efficient health system, while a score below 100% means that there is scope to improve efficiency by either producing more output or reducing inputs to achieve a score of 100%.
3.5 Factors Affecting the Efficiency of Health Systems
3.5.1 Demographic Characteristics of the Population
Several population/demographic characteristics were found to determine health system technical efficiency. One of these was population density. Some studies found that a high population density of a country or sub-national unit (region/district etc) was associated with increased technical efficiency. For instance, a study of the primary healthcare system in Chile found that a high population of primary healthcare catchment areas increased the technical efficiency regional health systems [61]. Ahmed et al. assessed the technical efficiency of the health systems of 46 Asian countries and found that countries having more than 200 people per square kilometre were more technically efficient compared with the countries with ≤ 100 population per square kilometre. Higher population densities increased the technical efficiency of regional health systems by reducing distances to populations and making it easier for health systems to organise and utilise their services infrastructure, and by reducing per capita cost of healthcare [33]. However, some studies reported a negative association between population density and health system technical efficiency. For instance, a study of Finnish municipalities found that large populations reduced the technical efficiency of municipalities and speculated that this could be because other factors related to population size such as quality differences, bureaucratic inefficiency, or unmeasured outputs [34]. A study in Kenya found that the technical efficiency of county health system was negatively associated with population density, and speculated that this was likely because higher population densities were not matched with healthcare resources and hence compromising health outcomes [86]. Another factor that was explored was the rural/urban distribution of the population. There is a general finding that regions with low urbanisation rates are likely to be less technically efficient [34, 35, 87]. This was because, among others, lower urbanisation was associated with lower unemployment rates and lower income levels that affect healthcare utilisation [88]. Population age structure was also explored; high proportions of the very young (children) or the very old reduced the technical efficiency of health systems because these vulnerable populations increased the cost of healthcare [33, 61].
3.5.2 Socio-Economic Characteristics of the Population/Social Determinants of Health
Several socio-economic characteristics of the population were examined. Some studies reported that improved socio-economic status of the population is positively associated with health system technical efficiency. For instance, several studies found that increased per capita income of a country or regions population was associated with increased technical efficiency of the health system [89]. However, some studies reported a negative association between population income per capita and health system technical efficiency. This was thought to be because health systems whose catchment populations had higher income per capita were characterised by higher levels of overprovision and higher costs of care.
In addition to average income levels in a country, the distribution of incomes was also found to determine health system technical efficiency. High income inequality and poverty was associated with reduced technical efficiency. Bekarogu and Heffley found that increased poverty and income inequality affected the technical efficiency of health system by reducing the overall level of health system outcomes. A related socio-economic characteristic was employment status, where high unemployment rates were associated with reduced health system technical efficiency [34].
Several studies found that access to basic sanitation and clean water increased the technical efficiency of health systems. This was because improved sanitation improved health outcomes, which was linked to improved technical efficiency of the system. For example, Grigoli and Kapsoli [90] found that the percentage of the population with access to sanitation services was associated with an increase in technical efficiency, while Hassan et al. [91] found that the rate of access to drinking water decreased the incidence of water-related diseases such as cholera, fever and malaria, and was associated with increased technical efficiency.
Increased literacy was associated with increased technical efficiency of health systems [26, 38, 87, 92]. For example, Ahmed et al. found that Asian countries with higher literacy levels have higher health system technical efficiency. This was thought to be because educated people more easily transform health information and knowledge into health outcomes [87, 89].
3.5.3 Macro-Economic Characteristics
Findings on the effect of the size of a country’s economy on health system technical efficiency were mixed. Some studies found that higher country per capita gross domestic product (GDP) was associated with a more technically efficient delivery of healthcare [93,94,95,96]. This was thought to be because increased country wealth could translate to increased investments in the health sector as well as other sectors that impact on social determinants of health, with improved health and quality of life having a positive impact on overall health outcomes. For instance, some studies found that countries with good road infrastructure and good access to electricity were associated with increased technical efficiency of health systems [87]. However, other studies found that higher GDP per capita was associated with lower technical efficiency of health systems. This was thought to be because of the increased cost of healthcare because of overprovision [15, 61, 97] and higher relative prices of healthcare in richer countries [98].
3.5.4 Health and Wellbeing of the Population
Several aspects of the health and wellbeing of the population affected the technical efficiency of the health system. Generally, higher prevalence of chronic disease was associated with reduced health system technical efficiency. For instance, Novignon and Lawanson found that HIV/AIDS negatively affects technical efficiency of health systems in Africa, with a similar finding reported in Kenya [86]. Allin et al. found that an increase in the proportion of people with chronic conditions by 10% would decrease the technical efficiency score by between 10 and 18% in regional health systems in Canada. Further, health systems that serve populations with high levels of health risk factors such as smoking, alcohol consumption and obesity were likely to be less technically efficient [15, 21, 59, 99]. For example, Bekaroglu and Heffley found that a high consumption of alcohol increases inefficiency by causing premature ill health and death. A high prevalence of chronic disease and health risk factors reduced health system outcomes and increased healthcare costs with negative impacts on health system efficiency.
3.5.5 Health System Characteristics
Several characteristics of health system functions were found to determine the efficiency of health systems. First, how health systems are financed affected health system efficiency in several ways. The fragmentation of financing arrangements, and specifically the presence of multiple health insurance firms, was negatively associated with health system efficiency [53, 77]. The level of health expenditure also had an impact on health system efficiency. Total health expenditure as a share of GDP was positively associated with the technical efficiency of health systems [38, 42, 65, 100]. The role of availability of funds was also highlighted in Kenya [47, 48]. This was thought to be because greater healthcare spending was essential in improving health outcomes [65]. However, some studies found that higher levels of total health expenditure can be negatively associated with efficiency when the health system is characterised by unnecessary care and/or higher costs of care [14, 15, 40, 48]. The source of funding for the health sector was also shown to affect technical efficiency. The share of public spending on healthcare was positively associated with health system technical efficiency [14]. Further, Increased population coverage with a prepayment health-financing mechanism (such as health insurance) was associated with increased technical efficiency of health systems [101]. An assessment in China found that provinces with a high proportion of out-of-pocket payments had lower technical efficiency [102]. However, some studies on the efficiency of OECD (Organisation for Economic Co-operation and Development) countries [98, 101] have found that out of pocket payments in the form of co-payments were positively associated with health system efficiency in contexts that have adequate population coverage with prepayment mechanisms. This was because co-payments disincentivized unnecessary use of care. Public finance management arrangements also influenced health system efficiency. Enhanced capacity to execute budgets, flow of funds directly to providers, timeliness of funds disbursements to local authorities and health facilities, the flexibility of budgets, and the autonomy of local authorities and health facilities over resources enhanced efficiency [45, 47, 48].
With regard to the purchasing function of the health system, how healthcare providers were paid also affected health system efficiency. For instance, prospective payments such as capitation, rather than fee-for-service payments, were founds to be positively associated with health system efficiency in some studies because they disincentivised unnecessary care and provided purchasers with better control over costs [103]. In the Democratic republic of Congo, the introduction of a zero-margin policy for drug sales in the public sector reduced the incentive of healthcare providers to prescribe unnecessary medicines [53]. The design and implementation of benefit packages also affects health system efficiency. Chile, Mexico and Uruguay improved the efficiency of their health systems by prioritising health services that are cost-effective in their benefit packages [53].
The efficiency of health systems was also found to be affected by how users interacted with the health service providers. Health systems where patients exercised choice of health providers were associated with higher technical efficiency [59]. Gate keeping by primary-care providers, where a patient is required to have a referral from a general practitioner for non-emergency access to a specialist, enhanced health system efficiency by aligning the level of specialisation and cost of healthcare with healthcare needs, and reducing healthcare costs [103]. However, some studies found that gate keeping could reduce health system efficiency in settings where primary-care physicians had limited ability to coordinate the follow-up of patient care, or in settings where the health system’s capacity to provide secondary care was limited [77]. Inadequate health system capacity to provide specialised care resulted in long waiting times, and increased the utilisation of emergency departments and hospitalisations and hence resulting in inefficiency [77]. The effectiveness of gate keeping in enhancing health system efficiency was also dependent on whether it was accompanied by interventions to improve the availability and quality of secondary-care services [77]. Further, an interaction between price regulation and gate keeping has been reported. It has been observed that when healthcare prices are regulated, gate keeping may reduce efficiency by incentivising excessive specialisation of healthcare professionals to access higher fees [60]. It also incentivises general practitioners to make unnecessary referrals of patients to specialised care so as to minimise their (general practitioner) input costs [60].
On health governance, strong regulation of health system functions, and specifically price regulation, medicine use, and health workforce regulation were associated with increased technical efficiency [53, 59, 60]. In China and El Salvador, the introduction medicines regulations that strengthened price regulation, generic prescribing, and the enforcement of national essential drugs lists improved health system efficiency [53]. Improved coordination in the health sector, including the coordination of donor initiatives, was also associated with improved health system efficiency [45, 53]. The Democratic Republic of Congo and Zambia realised improvement in health system efficiency by aligning and coordinating donor support with health sector priorities, and coordinating health sector planning, budgeting and resource allocation to reduce waste and duplication [36, 53]. Beyond health sector coordination, multisectoral coordination and partnerships to tackle social determinants of health were thought to improve efficiency [46]. Some studies reported that decentralisation of health functions was associated with higher technical efficiency of national and sub-national health systems [59]. An assessment of the technical efficiency of healthcare systems of selected middle-income countries found that technical efficiency was enhanced by decentralisation, which enhanced the delivery of care in rural areas, and improved the responsiveness of health systems to community needs through improved community participation in healthcare decision making [104]. Effective performance monitoring and accountability was found to improve health system efficiency in Canada [46]. Leadership and management practices and capacity were also thought to be a determinant of health system efficiency [45, 46, 53]. An assessment of the technical efficiency of 27 Latin American and Caribbean countries found a positive association between governance quality and system technical efficiency [26]. Governance quality in the study was defined as a multidimensional index that included measures of government effectiveness, voice and accountability, rule of law, regulatory quality, political stability and absence of violence/terrorism, and control of corruption. Further, assessments of the technical efficiency of WHO member country health systems found that an increase in democratisation and freedom was associated with increased health system technical efficiency [39, 94]. Corruption has also been found to be associated with reduced technical efficiency [69, 93].
The availability and distribution of health system hardware such infrastructure, equipment and health commodities were associated with increased technical efficiency of health systems [83]. Inadequate availability of input led to an inefficient mix of inputs with negative impacts on health system efficiency. For example, an assessment of the technical efficiency of Asian country health systems found that the density of hospital beds had a positive association with technical efficiency [83]. An assessment in Canada found that increased inequitable distribution of health workers was associated with increased technical efficiency of national and sub-national health systems [15]. In Ethiopia, an increase in the number of primary healthcare facilities that was not matched with an increase in the number of health workers resulted in inefficiency [53]. The level and distribution of health workers affected health system efficiency. National and sub-national health systems that had inadequate numbers of health workers were less efficient [97, 105]. Procurement inefficiencies were also identified. This included fragmented procurement of health commodities, high procurement prices, and supply chain challenges leading to delays in deliveries and stock-outs, and procurement corruption [45, 47, 53]. Verhoeven et al. [98] found that high spending on pharmaceuticals was associated with lower health system efficiency. This was thought to be because high pharmaceutical expenditure crowded out other healthcare inputs and hence reduced the efficient use of health resources.
Overprovision of health services (long lengths of stay, high referrals, high doctor consultations, high admission rates, inappropriate drug (such as antibiotic) use), an aspect of quality of care, was associated with reduced technical efficiency [15, 61, 97]. For example, Chai et al. found that negative association of admission rates with technical efficiency implied that a resource-intensive hospitalisation service use was harmful to health system technical efficiency. Ramirez-Valdivia et al. [61] found that increasing annual referrals to specialists increases the intechnical efficiency score. In China, the inappropriate use of drugs reduced health system efficiency [53].
The organisation of care to prioritise lower level basic care primary healthcare is associated with increased health system efficiency. Ding et al. [28] found that an increase in the proportion of medical services in primary facilities would increase the technical efficiency of provincial medical centres. The share of essential/basic services in benefit packages was positively associated with health system efficiency [53, 98]. This was because essential/basic services were more cost-effective compared to advanced/expensive care. Further, health systems with a high share of basic care health workers (rather than specialists) were likely to be more efficient [15, 59]. Policy reforms with a focus on expanding primary and community-based care, and engaging the community were shown to improve the technical efficiency of healthcare systems in OECD countries [43]. Further reforms geared on enhancing access to healthcare for the disadvantaged and vulnerable, and reducing inequality in access to healthcare services was associated with increased technical efficiency [43].
4 Discussion
Previous reviews of health system efficiency have either focused on the methods used in the analysis [106,107,108] or on synthesising the evidence on health facility level efficiency [107, 109]. This study presents a systematic review of empirical studies that have examined the efficiency of national or sub-national health systems. Our findings show that there were more publications from high and upper middle-income countries than from low-income and lower middle-income countries. One of the factors that may have contributed to this is the availability of rich cross-country data on high income countries such as the ones held by OECD and EU, and health system observatory databases. It underlies the need for LMICs to set up mechanisms to collate and curate health system data that could be used for monitoring health system performance.
All the identified studies assessed technical efficiency and its determinants and used quantitative approaches except for five studies that used qualitative approaches and three that used mixed methods and considered efficiency more broadly (beyond technical). While quantitative approaches quantified the level and determinants of health system efficiency, they did not provide insights on the mechanisms by which determinants interact with the technical efficiency of health systems. Quantitative approaches were also limited to assessing quantifiable factors (typically health system hardware), and missed non-quantifiable, software aspects of health systems. On the other hand, qualitative approaches provided more information about how certain factors might affect health system efficiency. They also identified determinants of efficiency that are not easily quantifiable—software factors such as the role of leadership and management practices, and health sector coordination. This highlights the need for mixed methods approaches that incorporate the use of qualitative methods to undertake in-depth assessments of the interplay of factors that determine health system efficiency.
While studies used a range of inputs, these were generally the building blocks of health systems, health risk factors, and social determinants of health. The common justification for the use of specific inputs and outputs in efficiency analysis was the fact that it had been used by a similar analysis in other settings and data availability. This finding is similar to that of a review efficiency analysis of primary-care systems [107]. A limitation to this input/output selection approach is the likelihood that the selected inputs/outputs may not be relevant and suitable to characterising specific health systems. Exercises to engage health system decision makers and implementors in specific contexts to understand their health systems and identify context-appropriate inputs and outputs for efficiency analysis should be explored. Such efforts will require and inform the strengthening of data systems for health system performance monitoring and evaluations in specific contexts.
The findings on factors that determine the efficiency of health systems highlight several issues. First, that the efficiency of national and sub-national health system is partly determined by factors not easily influenced by health system policy makers. Broader contextual factors such as the demographic, individual and household socio-economic, macro-economic, and governance and political system characteristics of the national and sub-national unit are outside of the control of health system policy makers. This emphasises the fact that health systems are part of and are affected by the larger society that forms their contexts and underlies the need for countries to strengthen multisectoral coordination and approaches to health [110, 111].
Second, the efficiency of national and sub-national health systems is also affected by the general health and wellbeing of populations. This underlies the need for health policy makers to prioritise investments in preventive and promotive interventions that reduce the risk of disease, and the management of chronic conditions to reduce their burden on health systems. Health system reforms aimed at promoting efficiency should not only focus on optimising health system functions to provide care for the sick, but also prioritise interventions to prevent and promote health and wellbeing of the population. Investing in preventive and promotive health interventions has been shown to be cost effective [112] and prioritising preventive and promotive health has been identified as an efficiency enhancing intervention by the WHO 2010 world health report [113].
Lastly, health system arrangements offer several policy levers for improving the efficiency of national and sub-national health systems. These factors are key because they are under the direct control of health system managers and policy makers and can be leveraged to enhance health system efficiency. On health governance, strengthening health sector leadership and management, enhancing health sector coordination as well as multisectoral coordination, decentralisation of health functions, and introducing/strengthening the regulation of health workers and healthcare costs/pricing should be considered. These findings resonate with those of other analyses. For instance, a review of 10 case studies of health system efficiency found that strengthening health sector regulation, pharmaceutical pricing, and enhancing donor coordination enhanced the efficiency of country health systems [114]. With regard to health financing, interventions include scaling-up prepayment health financing mechanisms and reducing the level of out-of-pocket payments. Purchasing and public finance management (PFM) reforms that include defining evidence-based, cost-effective benefit packages, reforming payment systems to transition to prospective payment mechanisms, strengthening budget execution and flexibility of budgets, the direct payment of healthcare providers (to improve provider autonomy, and flow of funds), health facility autonomy, and ensuring patient choice of health providers may promote the efficiency of health systems. Yip and Hafez [114] found that the introduction of evidence based benefit packages enhanced health system efficiency in Chile and Uruguay while scaling population coverage with prepayment financing systems was efficiency enhancing in Mexico. On health system hardware, investing in adequate levels of health workers, health commodities, and health infrastructure, as well as interventions to ensure equity (including geographical) in their distribution and access are key. Having an optimal mix of health system inputs has been identified by other studies as efficiency enhancing [113]. On service delivery, policy options include re-orienting health systems to prioritise primary health care and strengthening community health systems and strengthening gate keeping and referral systems. Investments are needed to support care at all levels, for example, increasing PHC financing, coverage of basic services, prioritising health workers providing primary healthcare. In Ethiopia, investment in health extension workers that provided community health services to catchment populations improved the efficiency of the health system by improving access to primary healthcare [53]. Further, interventions to strengthen quality of care and curb overprovision of unnecessary care should be considered. The WHO report on the ten leading causes of efficiency identified examples that include inappropriate hospital admissions, medical errors, and overuse of equipment, investigations, and procedures [113]. Further, the introduction of essential medicines list to guide medicine procurement was found to be efficiency enhancing in China [114].
Policy options will, however, need to appropriate for context and take a whole system view given that policy reforms are efficiency enhancing only if they are implemented in policy environments that they are aligned with or coherent. For instance, while increasing the level of financing to the health sector may enhance efficiency, this needs to be accompanied by reforms to contain overprovision/unnecessary care or price increases. While gate keeping by primary healthcare providers may enhance health system efficiency in contexts with good availability and quality of secondary care services, and controls that check against unnecessary referrals. Further, cost-sharing appears to be efficiency enhancing in settings in context with adequate prepayment health financing mechanisms. Policy interventions will therefore need to be contextualised for specific settings.
A potential limitation of this review is the likelihood of missing out key literature since we conducted searches on only two databases. Further, this review presents a qualitative evaluation of determinants of efficiency rather thana quantification of their impacts. Further research could therefore include meta-analysis of the impact of interventions to address health system efficiency.
5 Conclusion
This review highlights the asymmetry of evidence on health system efficiency between HICs and LMICs, with most studies focusing on HICs. It underscores the need to carry out studies to understand the levels and determinants of system level health system efficiency in LMICs. The review also reveals the dearth of efficiency studies that use mixed methods approaches by incorporating qualitative inquiry. While the standard quantitative approaches determine the level of efficiency and the factors that influence efficiency, they fall short in illuminating how and why certain factors influence health systems efficiency in certain contexts. There is therefore a need for mixed methods approaches to deepen the understanding of efficiency and its determinants in different settings. Lastly, the review offers insights on the drivers of the efficiency of national and sub-national health systems, highlights potential targets for reforms to improve health system efficiency.
References
World Health Organization. The World Health Report 2000. Health systems: improving performance. 2000.
Jacobs R, Smith PC, Street A. Measuring efficiency in health care: analytic techniques and health policy. Cambridge: Cambridge University Press; 2006.
Hollingsworth B. Cost, production, efficiency, or effectiveness: where should we focus? Lancet Glob Health. 2013;1(5):e249–50.
Cylus J, Papanicolas I, Smith PC. Health system efficiency. How to make measurement matter for policy and management. 2016.
World Health Organization. Everybody's business. Strengthening health systems to improve health outcomes. WHO's framework for action. 2007.
Kutzin J. Health financing policy: a guide for decision-makers. Health financing policy paper. Copenhagen, WHO Regional Office for Europe, 24, 2008.
Palmer S, Torgerson DJ. Definitions of efficiency. BMJ. 1999;318(7191):1136.
Farrell MJ. The measurement of productive efficiency. 1957.
Coelli TJ, et al. An introduction to efficiency and productivity analysis. 2nd ed. New York: Springer Science & Business Media; 2005.
Hollingsworth B, Peacock S. Efficiency measurement in health and health care. Oxon: Routledge; 2008.
World Health Organization. Health systems financing: the path to universal coverage. 2010.
Tandon A, Cashin C. Assessing public expenditure on health from a fiscal space perspective. Washington, DC: World Bank; 2010. p. 1–84.
Powell-Jackson, T., K. Hanson, and D. McIntyre, Fiscal space for health: a review of the literature. 2012: London, UK.
Karpa W, Leśniowska J. Efficiency of Health Care Systems: Stochastic Frontier Analysis Including Innovation Component. Prace Naukowe Akademii im. Jana Długosza w Częstochowie. Pragmata Tes Oikonomias. 2014; (8): 159–67
Allin S, Grignon M, Wang L. The determinants of efficiency in the Canadian health care system. Health Econ Policy Law. 2016;11(1):39–65.
PRISMA. PRISMA-TRANSPARENT REPORTING of SYSTEMATIC REVIEWS and META-ANALYSES. 2015. http://www.prisma-statement.org/. Accessed 31 Dec 2017.
Mijovic H, McKnight J, English M. What does the literature tell us about health workers’ experiences of task-shifting projects in sub-Saharan Africa? A systematic, qualitative review. J Clin Nurs. 2016;25(15–16):2083–100.
CASP UK. Critical Appraisal Skills Programme (CASP) Check lists. 2017. http://www.casp-uk.net/casp-tools-checklists. Accessed 31 July 2017.
Hannes K. Chapter 4: Critical appraisal of qualitative research in Noyes J, Booth A, Hannes K, Harden A, Harris J, Lewin S, Lockwood C (editors), Supplementary Guidance for Inclusion of Qualitative Research in Cochrane Systematic Reviews of Interventions. 2011. http://cqrmg.cochrane.org/supplemental-handbook-guidance. Accessed 1 Sept 2015.
Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Alan B, Robert GB, editors. Analyzing qualitative data. The qualitative researcher’s companion. Oxon: Routledge; 1994. p. 173–94.
Bekaroglu C, Heffley D. A multi-stage efficiency analysis of OECD healthcare systems. J Manag Econ Res. 2018;16(2):264–85.
Evans DB, et al. The comparative efficiency of national health systems in producing health: an analysis of 191 countries. World Health Organization. 2000;29(29):1–36.
Aristovnik A. Measuring relative efficiency in health and education sector: the case of East European countries. Actual Probl Econ. 2012;10(136):305–14.
Kim Y, Park MJ, Atukeren E. Healthcare and Welfare Policy Efficiency in 34 Developing Countries in Asia. Int J Environ Res Public Health. 2020;17:4617.
Singh S, et al. Application of DEA-Based Malmquist Productivity Index on healthcare system efficiency of ASEAN Countries. Int J Health Plan Manag. 2020;36:1236–50.
Moreno-Serraa R et al. An exploratory application of data envelopment analysis to the efficiency of health service coverage and access. Results for Development Institute. 2012.
Novignon J, Lawanson A. Efficiency of health systems in sub-Sahara Africa: a comparative analysis of time varying stochastic frontier models, MPRA paper 56897. Berlin: University Library of Munich; 2014.
Ding J, et al. Equity and efficiency of medical service systems at the provincial level of China’s mainland: a comparative study from 2009 to 2014. BMC Public Health. 2018;18(1):214.
Du T. Performance measurement of healthcare service and association discussion between quality and efficiency: evidence from 31 provinces of mainland china. Sustainability. 2017;10(1):74.
Ngobeni V, Breitenbach MC, Aye GC. Technical efficiency of provincial public healthcare in South Africa. Cost Eff Resour Alloc. 2020;18(3):1–19.
Mousa W, Aldehayyat JS. Regional efficiency of healthcare services in Saudi Arabia. Middle East Dev J. 2018;10(1):152–74.
Schleiniger R. Regional quantity, productivity and efficiency measures of the Swiss health care system. Swiss J Econ Stat. 2008;144(3):459–76.
Varela PS, de Andrade Martins G. Efficiency of primary health care spending by municipalities in the metropolitan region of Sao Paulo: a comparative analysis pf DEA models. Rev Bus. 2011;32(1):17–35.
Loikkanen HA, Susiluoto I. Cost efficiency of Finnish municipalities in basic service provision 1994–2002. 2005.
Purohit BC. Efficiency in health care sector in Bihar (India): An exploratory analysis using DEA. Afr J Health Econ. 2015;4(2):1–13.
Chansa C, et al. Exploring SWAp’s contribution to the efficient allocation and use of resources in the health sector in Zambia. Health Policy Plan. 2008;23(4):244–51.
Anselmi L, Lagarde M, Hanson K. The efficiency of the local health systems: investigating the roles of health administrations and health care providers. Health Econ Policy Law. 2018;13(1):10–32.
Evans DB, et al. Comparative efficiency of national health systems: cross national econometric analysis. BMJ. 2001;323(7308):307–10.
Kumbhakar SC. Efficiency and productivity of world health systems: where does your country stand? Appl Econ. 2010;42(13):1641–59.
Herrera S, Pang G. Efficiency of public spending in developing countries: an efficiency frontier approach. Washington, DC: The World Bank; 2005.
Allin S, et al. How can health system efficiency be improved in Canada? Healthc Policy. 2015;11(1):33.
Popescu C, Asandului L, Fatulescu P. A data envelopment analysis for evaluating Romania’s health system. Procedia Soc Behav Sci. 2014;109:1185–9.
Ozcan YA, Khushalani J. Assessing efficiency of public health and medical care provision in OECD countries after a decade of reform. CEJOR. 2017;25(2):325–43.
Kujawska J. Efficiency of healthcare systems in european countries-the DEA network approach. Metody Ilościowe w Badaniach Ekonomicznych. 2018;19:60–70.
Nyawira L, et al. Examining health sector stakeholder perceptions on the efficiency of county health systems in Kenya. PLoS Glob Public Health. 2021;1(12):e0000077.
Allin S, et al. Improving health system efficiency: perspectives of decision makers. Healthc Q. 2017;20(1):10–3.
Moses MW, et al. Performance assessment of the county healthcare systems in Kenya: a mixedmethods analysis. BMJ Glob Health. 2021;6:e004707.
Zeng W, et al. Understanding the performance of county health service delivery in Kenya: a mixed-method analysis. Health Policy Plan. 2022;37(2):189–99.
Nannyonjo J, Okot N. Decentralization, local government capacity and efficiency of health service delivery in Uganda. J Afr Dev. 2013;15(1):125–58.
Hooda Y. Efficiency in expenditure on healthcare system at state level in India. Int J Adv Res Manag Soc Sci. 2018;7:34–41.
Purohit BC. Efficiency of social sector expenditure in India: a case of health and education in selected Indian states. Healthc Low Resource Settings. 2014;2(1):26–34
Felder S, Tauchmann H. Federal state differentials in the efficiency of health production in Germany: an artifact of spatial dependence? Eur J Health Econ. 2013;14(1):21–39.
Yip W, Hafez R, Organization WH. Improving health system efficiency: reforms for improving the efficiency of health systems: lessons from 10 country cases. World Health Organization. 2015.
Nyawira L, et al. Examining health sector stakeholder perceptions on the efficency of county ehalth systems in Kenya. PLoS Global Public Health. 2021;1(12):e0000077.
Zeng W, et al. Understanding the performance of county health service delivery in Kenya: a mixed-method analysis. Health Policy Plan. 2021;00:1–11.
Charnes A, Cooper W, Rhodes E. Measuring of efficiency of decision making units. Eur J Oper Res. 1978;2:429–39.
Aigner D, Lovell C, Schmidt P. Formulation and estimation of stochastic frontier production function models. J Econom. 1977;6:21–37.
Makiela K. State level efficiency measures for healthcare systems. 2010.
Şenel T, Cengiz MA. A bayesian approach for evaluation of determinants of health system efficiency using stochastic frontier analysis and beta regression. Comput Math Methods Med. 2016.
de Cos PH, Moral-Benito E. Determinants of health-system efficiency: evidence from OECD countries. Int J Health Care Finance Econ. 2014;14(1):69–93.
Ramírez-Valdivia MT, Maturana S, Salvo-Garrido S. A multiple stage approach for performance improvement of primary healthcare practice. J Med Syst. 2011;35(5):1015–28.
De Nicola A, Gitto S, Mancuso P. A two-stage DEA model to evaluate the efficiency of the Italian health system. 2011.
Gravelle H, et al. Comparing the efficiency of national health systems: a sensitivity analysis of the WHO approach. Appl Health Econ Health Policy. 2003;2(3):141–7.
Purohit BC. Healthcare sector efficiency in Gujarat (India): an exploratory study using data envelopment analysis. Healthc Low Resour Settings. 2016;4(1). https://doi.org/10.4081/hls.2016.5525
See KF, Yen SH. Does happiness matter to health system efficiency? A performance analysis. Heal Econ Rev. 2018;8(1):33.
Sankar D, Kathuria V. Health system performance in rural India: efficiency estimates across states. Econ Political Wkly. 2004: 39(13):1427–33
Sinimole K. Evaluation of the efficiency of national health systems of the members of World Health Organization. Leadersh Health Serv. 2012;25(2):139–50.
Tandon A, et al. Measuring overall health system performance for 191 countries. Geneva: World Health Organization; 2000.
Tandon A. Measuring efficiency of macro systems: an application to Millennium Development Goal attainment. 2005.
Achoki T, et al. Technical and scale efficiency in the delivery of child health services in Zambia: results from data envelopment analysis. BMJ Open. 2017;7(1): e012321.
Stefko R, Gavurova B, Kocisova K. Healthcare efficiency assessment using DEA analysis in the Slovak Republic. Health Econ Rev. 2018;8(1):6.
Dash U, Vaishnavi SD, Muraleedharan VR. Technical efficiency in the use of healthcare resources: a case study of Tamil Nadu. Indian Econ Rev. 2008;43(1):69–82
Anton SG. Technical efficiency in the use of health care resources: a cross-country analysis. Ann Alexandru Ioan Cuza Univ Econ. 2013;60(1):1–12.
Kinfu Y, Sawhney M. Inefficiency, heterogeneity and spillover effects in maternal care in India: a spatial stochastic frontier analysis. BMC Health Serv Res. 2015;15(1):118.
Suraratdecha C, Okunade AA. Measuring operational efficiency in a health care system: a case study from Thailand. Health Policy. 2006;77(1):2–23.
Canagarajah S, Ye X. Public health and education spending in Ghana in 1992–98: issues of equity and efficiently, Vol. 2579. 2001; World Bank Publications.
Hadad S, Hadad Y, Simon-Tuval T. Determinants of healthcare system’s efficiency in OECD countries. Eur J Health Econ. 2013;14(2):253–65.
Ibrahim MD, Daneshvar S. Efficiency analysis of healthcare system in Lebanon using modified data envelopment analysis. J Healthc Eng. 2018;2018:2060138. https://doi.org/10.1155/2018/2060138.
Porcelli F. Electoral accountability and local government efficiency: quasi-experimental evidence from the Italian health care sector reforms. Econ Gov. 2014;15(3):221–51.
Lee S, Kim C. Estimation of association between healthcare system efficiency and policy factors for public health. Appl Sci. 2018;8(12):2674.
González E, Cárcaba A, Ventura J. Value efficiency analysis of health systems: does public financing play a role? J Public Health. 2010;18(4):337–50.
Spinks J, Hollingsworth B. Cross-country comparisons of technical efficiency of health production: a demonstration of pitfalls. Appl Econ. 2009;41(4):417–27.
Ahmed S, et al. Measuring the efficiency of health systems in Asia: a data envelopment analysis. BMJ Open. 2019;9:e022155.
Moreno-Serra R, Anaya-Montes M, Smith PC. Potential determinants of health system efficiency: evidence from Latin America and the Caribbean. PLoS One. 2019;14(5): e0216620.
Zarulli V, et al. Health care system efficiency and life expectancy: a 140-country study. PLoS One. 2021;16(7): e0253450.
Barasa E, et al. Level and determinants of county health system technical efficiency in Kenya: two stage data envelopment analysis. Cost Eff Resour Alloc. 2021;19(78):1–11.
Purohit BC. Efficiency in healthcare sector in Assam: a sub-state level analysis. Online J Health Allied Sci. 2016;14(4):1.
Prachitha J, Shanmugam K. Efficiency of raising health outcomes in the Indian States. Chennai: Madras School of Economics; 2012.
Purohit BC. Efficiency of health care sector at sub-state level in India: a case of Punjab. Online J Health Allied Sci. 2009;8(3):212–25.
Grigoli F, Kapsoli J. Waste not, want not: the efficiency of health expenditure in emerging and developing economies. Rev Dev Econ. 2018;22(1):384–403.
Hassan CM, Djekonbe D, DRD T. The efficiency of the health system in Chad. 2018.
Hollingsworth B, Wildman J. The efficiency of health production: re-estimating the WHO panel data using parametric and non-parametric approaches to provide additional information. Health Econ. 2003;12(6):493–504.
Lagravinese R, Paradiso M, Mastromarco C. Social heterogeneity and efficiency in Italian health care system: a Simar–Wilson methodology analysis. Società Italiana degli Economisti Working Paper September, 2011. 15: p. 2011.
Greene W. Distinguishing between heterogeneity and inefficiency: stochastic frontier analysis of the World Health Organization’s panel data on national health care systems. Health Econ. 2004;13(10):959–80.
Ravangard R, et al. Factors affecting the technical efficiency of health systems: a case study of Economic Cooperation Organization (ECO) countries (2004–10). Int J Health Policy Manag. 2014;3(2):63.
Lagravinese R, Paradiso M, Mastromarco C. Social heterogeneity and efficiency in Italian healthcare system: a Simar–Wilson methodology analysis. 2011, Department of Economics, University of Bari
Chai P, Wan Q, Kinfu Y. Efficiency and productivity of health systems in prevention and control of non-communicable diseases in China, 2008–2015. Eur J Health Econ. 2021;22:267–79.
Verhoeven M, Gunnarsson V, Lugaresi S. The health sector in the Slovak Republic: efficiency and reform. IMF Working Papers, 2007. p. 1–25.
Jafarov E, Gunnarsson V. Efficiency of government social spending in Croatia. Financial Theory Pract. 2008;32(3):289–320.
Gong G, et al. Has the efficiency of China’s healthcare system improved after healthcare reform? A network data envelopment analysis and Tobit regression approach. Int J Environ Res Public Health. 2019;16:4847.
Wranik D. Healthcare policy tools as determinants of health-system efficiency: evidence from the OECD. Health Econ Policy Law. 2012;7(2):197–226.
Chai P, et al. Technical and scale efficiency of provincial health systems in China: a bootsrappin data envelopment analysis. BMJ Open. 2019;9:e027539.
Bhat VN. Institutional arrangements and efficiency of health care delivery systems. Eur J Health Econ. 2005;6(3):215–22.
Nassar H, et al. Technical efficiency of health-care systems in selected middle-income countries: an empirical investigation. Review of economics and political science. 2020;5(4):267–87.
Sousa A, et al. Measuring the efficiency of human resources for health for attaining health outcomes across subnational units in Brazil. World health report, 2006.
Varabyova Y, Müller J-M. The efficiency of health care production in OECD countries: a systematic review and meta-analysis of cross-country comparisons. Health Policy. 2016;120:252–63.
Pelone F, et al. Primary care efficiency measurement using data envelopment analysis: a systematic review. J Med Syst. 2015;39:156.
Hussey PS, et al. A systematic review of health care efficiency measures. Health Services Res. 2009;44(3):784–805.
Asbu EZ, Masri MD, Naboulsi MA. Determinants of hospital efficiency: a literature review. Int J Healthc. 2020;6(2).44–53.
Bennett S, Glandon D, Rasanathan K. Governing multisectoral action for health in low-income and middle-income countries: unpacking the problem and rising to the challenge. BMJ Glob Health. 2018;3(Suppl 4):e000880.
Tangcharoensathien V, et al. Multisectoral actions for health: challenges and opportunities in complex policy environments. Int J Health Policy Manag. 2017;6(7):359–63.
Merkur S, Sassi F, McDaid D. Promoting health, preventing disease: is there an economic case? WHO Regional Office for Europe: Denmark; 2013.
WHO. More health for the money, in World Health Report—Health Systems Financing; the path to universal coverage. 2010, World Health Organization: Geneva.
Yip W, Hafez R. Reforms for improving the efficiency of health systems: lessons from 10 country cases; 2015. World Health Organization.
Acknowledgements
This paper is published with the permission of the director KEMRI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable—this is a review of literature.
Consent for publication
Not applicable—this is a review of literature.
Availability of data and materials
All the data used for this study, as well as the coding framework used, are publicly available as Online Supplementary files.
Conflict of interests
All authors declare no competing interests.
Funding
This work was funded by a MRC/FCDO/ESRC/Wellcome Trust Health Systems Research Initiative (HSRI) Grant no MR/R01373X/1.
Authors’ contributions
EB, JJ, KH, AM, LN, IM, SM, BS, and CN conceived of the study. EB and RM collected data. EB and RM analysed the data and wrote the first version of the manuscript. All authors contributed to further analysis and writing of subsequent versions of the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mbau, R., Musiega, A., Nyawira, L. et al. Analysing the Efficiency of Health Systems: A Systematic Review of the Literature. Appl Health Econ Health Policy 21, 205–224 (2023). https://doi.org/10.1007/s40258-022-00785-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-022-00785-2