Abstract
Purpose of Review
This review aims to highlight key factors in the perioperative environment that contribute to transmission of infectious pathogens, leading to healthcare-associated infection. This knowledge will provide anesthesia providers the tools to optimize preventive measures, with the goal of improved patient and provider safety.
Recent Findings
Over the past decade, much has been learned about the epidemiology of perioperative pathogen transmission. Patients, providers, and the environment serve as reservoirs of origin that contribute to infection development. Ongoing surveillance of pathogen transmission among these reservoirs is essential to ensure effective perioperative infection prevention.
Summary
Recent work has proven the efficacy of a strategic approach for perioperative optimization of hand hygiene, environmental cleaning, patient decolonization, and intravascular catheter design and handling improvement protocols. This work, proven to generate substantial reductions in surgical site infections, can also be applied to aide prevention of SARS-CoV-2 spread in the COVID-19 era.
Similar content being viewed by others
Introduction
On May 15, 1850, the Hungarian obstetrician Ignaz Semmelweis lectured at the Vienna Medical Society and implored his colleagues to wash their hands in order to prevent the spread of infection between patients. [1] According to the Centers for Disease Control (CDC), 1 in 25 hospitalized patients in the United States is diagnosed annually with an infection that is the result of simply being hospitalized. [2] The healthcare-associated infection (HAI) risk in the operating room is even higher with 7% of surgical patients suffering from one or more infections. It is estimated that the direct cost of HAIs is upwards of $45 billion annually. [3]
Over the past decade, much has been published about the role of the perioperative environment in cross-contamination. [4••, 5, 6••] In this review, we detail what is known to date about factors contributing to perioperative pathogen transmission and present the importance of an infection prevention bundle that will allow anesthesiologists to impact the perioperative safety of patients and providers by preventing the spread of infectious pathogen. An editorial comment by Drs. Roy, Brull, and Eichhorn characterizes so well the need for anesthesiologists to address the issue of surgical site infections, “we’ve all been slimed! Now what are we going to do about it?” [7] In response, much work has been done to show exactly what we can and should do to address this persistent and significant issue.
Modes of Transmission of Healthcare-Associated Infections
Despite advances in surgical technique, sterilization, and improved disinfection programs, the U.S. health care system has struggled to generate a sustained, overall improvement in HAI rates. [8,9,10] The operating room (OR) environment includes health care tools and surfaces used within the anesthesia work environment (AWE), the surrounding air, as well as the patient and the anesthesia providers themselves. [11,12,13,14] This is a significant issue for both patients and providers because of current cleaning failures and/or lapses in practice that increase the risk of cross-contamination during patient care. [15] Further, contamination of intravascular devices has been repeatedly associated with increased patient mortality. [15, 16]
The risk of HAI is especially problematic in the COVID-19 era where the highly transmissible and infectious SARS-CoV-2 virus is transmitted to providers and patients even without evidence of aerosolization in some studies. [17] Such work highlights the importance of fomite transmission where contact with residual contamination can lead to recurrent, downstream provider, and/or patient transmission events that can lead to devastating consequences including death. [17] Importantly, COVID-19 can remain viable for at least 4 days on a variety of materials commonly encountered in ORs. [18] Other enveloped viruses such as hepatitis continue to cause HAIs as a result of unsafe injection practices and contaminated medical equipment. [19,20,21]
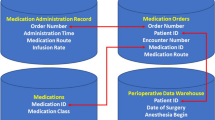
Emerging knowledge has shed light on three important sources of perioperative pathogen vectors: (1) the anesthesia provider, (2) the operative patient, and (3) the operative environment. A complex dynamic exists as an anesthesiologist must interface rapidly with these vectors in parallel to provide safe perioperative patient care which makes the risk for pathogen cross-contamination seemingly inevitable. For example, due to the high task density of the anesthesia work environment, there are up to 150 World Health Organization (WHO)-based hand hygiene opportunities per hour of anesthesia care. [22] As shown in Fig. 1, there are a very high number of patient-provider-environmental interactions for anesthesia providers during routine, elective surgery. This task density can lead to failures in basic preventive measures, further highlighting the need for ongoing surveillance for system optimization, an effective approach for prevention of perioperative Staphylococcus aureus spread and surgical site infection development that can be applied to control the perioperative spread of SARS-CoV-2. [23••, 24••] The evidence pertaining to the components of this effective strategy is summarized below.
The Anesthesia Provider
Intraoperatively, the hands of the anesthesia providers have been directly linked by advanced molecular techniques to stopcock contamination and postoperative infection. [14, 16] Fukada et al. sought to examine bacterial contamination on the anesthesiologists’ hands during general anesthesia and found that they were contaminated with bacterial pathogens throughout all phases of anesthesia care. [14] Another study examining bacterial cross-contamination reported that the contaminated hands serve as a source of environmental and stopcock set contamination in the OR. [15] Yet, perioperative hand hygiene compliance remains low.
Barriers to hand hygiene compliance include environmental and cultural issues. [22] Physical access to hand sanitizers plays a large role, as does continuous education regarding the risks. [25] Biddle and Shah (2012) reported a hand hygiene failure rate of 82% for anesthesia providers. [26] Tait and Tuttle surveyed anesthesiologists and reported that 95% of the providers reported hand washing after caring for “high-risk” patients, but only 58% washed their hands in “low-risk” situations. [27] In a study by Munoz-Price, only 13 hand hygiene events were witnessed during 8 h of observation of 19 anesthesiologists who collectively interacted with their work environment more than 1000 times. [28] When characterized, evidence reveals that these lapses frequently involve failure to wash one’s hands before and/or after aseptic tasks involving line insertions, bronchoscopy, or even after blood administration and handling. [29] As highlighted by Fernandez et al., many of these lapses are related to knowledge deficits pertaining to the importance of the contaminated environment in cross-contamination events involving infectious pathogens; the anesthesia environment is in fact the most potent transmission vehicle. [15, 16, 30]
When taken together, these data support the potential links between anesthesia providers and postoperative infectious outbreaks reported as early as the 1960s. One outbreak involved group A β-hemolytic streptococci-derived puerperal sepsis occurring in the postoperative period, whereas another involved two outbreaks of Staphylococcus aureus surgical site infections (SSIs) thought to originate with the contaminated hands of an anesthesia provider suffering from psoriasis. [31,32,33] Unfortunately, these early findings have been further substantiated by recent work involving single-nucleotide variant analysis that definitively links the hands of anesthesia providers to transmission of high-risk desiccation tolerant sequence type 5 Staphylococcus aureus strain characteristics that resulted in downstream infection development. [34] Thus, there is a substantial body of evidence highlighting the role of anesthesia provider hands in perioperative infection and the need to act for patient safety. This is even more important in the COVID-19 era with the tremendous transmission pressure related to SARS-CoV-2 community spread, a risk to both patients and providers during elective surgery that is in part related to OR hand hygiene compliance. [35] Importantly, when employed as a single measure, hand hygiene improvement strategies in the perioperative and similarly fast-paced intensive care unit (ICU) may increase the risk of HAI development. [3, 9] Hence, it is an important component of a multifaceted approach shown to reduce SSIs by greater than 80%. [23••]
Another provider infection control consideration involves the common practice of wearing masks in the OR for the purpose of decreasing the aerosolization of bacteria originating in the providers nasopharynx. A Cochrane review in 2014 suggested that it is unclear whether the wearing of surgical masks by OR personnel during “clean” surgery either increases or reduces the risk of SSIs. [36] However, for prevention of perioperative viral spread, there is evidence that various types of masks, whether donned by the provider or patient, can help to reduce shedding of the virus from the person to the surrounding environment. A limitation is coughing where the beneficial impact of the mask is attenuated. [37]
The Operative Patient
Pathogenic organisms from patient colonization of the nose, mouth, and skin are a known source of SSIs, with Staphylococcus aureus being the most commonly implicated organism. [38] Rectal colonization that commonly occurs in conjunction with skin colonization and the antecubital fossa, where the blood pressure cuff comes into contact with the axilla, have also been shown to be significant predictors of gram-negative bacterial transmission. [39, 40] In a prospective randomized observational study, the authors reported that for Acinetobacter, Pseudomonas, Brevundimonas, Enterobacter, and Moraxella, provider hands are less likely to serve as the reservoir of origin for transmission events than contaminated environmental or patient skin surfaces such as the axilla. [41] Bitkover prospectively investigated 20 operating rooms and reported that bacteria in the sternal wound originated from both the patient’s own skin and the surgical team. [42] Recent work involving a study design across 20 institutions demonstrated an association between a bundled intervention involving preoperative Staphylococcus aureus screening combined with customized decolonization and prophylactic antibiotic selection and a significant reduction in complex infections for patients undergoing hip and knee surgeries (17 fewer infections per 10,000 surgeries; 95% CI − 39 to 0; risk ratio 0.48). [43] While preoperative decolonization represents an evidence-based strategy for SSI prevention, the impact of this approach alone is far less effective than a multifaceted approach. [23••]
The Operative Environment
It has been well established that syringes and intravascular catheters can become contaminated directly via bacterial contamination of the provider’s hands, or indirectly during connection to patient intravenous (IV) tubing. [44,45,46] Blogg et al. reported that syringes can become contaminated with bacterial pathogens after a single use, thereby providing a plausible mechanism for the bacterial contamination of propofol vials linked to a series of Staphylococcus aureus bloodstream infections. [47,48,49] Breaches in aseptic practices and failure to decontaminate vials lead to microbial contamination of the vials, and then subsequently line associated bloodstream infections. [50] Residual microbial contamination of laryngoscopes, associated with suboptimal disinfection practices, has been linked to infectious outbreaks. [51] Contamination of anesthesia machine surfaces with blood, mucus, and bacterial organisms after standard cleaning processes has been confirmed. [11, 52] Other reports have documented an association of residual contamination of the anesthesia machine circuit and Ambu-bag with outbreaks of Pseudomonas aeruginosa respiratory infections. [53]
Early work by Albrecht and Dryden identified an association between combined preoperative decontamination of the external surface of anesthesia machine circuits and use of new absorbers with a reduction in postoperative pneumonia. These authors concluded that contaminated anesthesia machines can indeed transmit bacteria to patients. [54, 55] Leijten et al. published the results of a study in which they found that without an in-line circuit filter in place, bacterial organisms were universally transmitted to the patient circuit. [56] Edmiston et al. published the results of a study whereby air samples were taken during 70 different vascular procedures from a single OR. Coagulase-negative Staphylococcus and Staphylococcus aureus were recovered from 86% and 64% of all samples, respectively, with Gram-negative bacteria recovered less frequently (33%). [57] Isolation of 100 colony-forming units per surface area sampled (CPSS) from the AWE is associated with increased probability of high-risk stopcock contamination events that are in turn associated with increased mortality. [15, 16] A study by van Vlymen demonstrated that poor hand hygiene practices inadvertently cause tiny amounts of hepatitis C virus to be placed on the outside of a medication vial, leading to further contamination and infection. [58] Improved frequency and quality of environmental cleaning of the AWE following induction and emergence of anesthesia have reduced the proportion of environmental sites reaching the 100 CFU threshold associated with high-risk stopcock transmission events. [59] This involved post-induction cleaning with a surface disinfection wipe containing both a quaternary ammonium compound and alcohol along with improved organization with designation of clean and dirty spaces, decreasing the proportion of sites reaching or exceeding 100 CFU from > 40 to 12%. A port-guard designed to shield stopcocks from the contaminated environment significantly reduced contamination of injected fluid. This involved an ex vivo study where 33 providers injected 1 mL of sterile saline into 4 different devices with the primary outcome effluent contamination. [60] Thus, this study shows directly that shielding from the contaminated environment can reduce high-risk transmission events.
Overview of a Perioperative Infection Control Bundle
We have summarized evidence characterizing the epidemiology of perioperative transmission. As this is a complex problem occurring in a fast-paced arena with a high task-density, a multi-faceted approach is indicated. [16] The impact of a strategic, multifaceted approach on the incidence of Staphylococcus aureus transmission and SSI development has been evaluated. A significant reduction in Staphylococcus aureus transmission events was achieved, events tightly associated with SSI development. In turn, SSIs were reduced by > 80%. [23••] The timely implementation of an evidence-based, perioperative infection control program can be used for prevention of SSI development and perioperative SARS-CoV-2 spread, especially when the interventions are augmented by parallel implementation of efficient OR management strategies (Table 1). The elements of this evidence-based approach as applied to each contributing reservoir are described below. A key point is that these interventions should be implemented in parallel during the process of patient care, not as single interventions.
The Anesthesia Provider
In the high task density perioperative environment, nadirs in hand hygiene compliance occur during the fast-paced periods of induction and emergence of anesthesia. [61] This barrier can be effectively combated by leveraging proximity to the provider. In the study by Koff et al., simple provision of personalized, body-worn, alcohol dispensers increased hourly hand decontamination events by 20-fold which correlated with a significant reduction in environmental and stopcock contamination and postoperative infections. In a randomized trial investigating the effect of basic preventive measures on prevention of perioperative Staphylococcus aureus transmission and the incidence of SSIs, the concept of proximity to the provider was again leveraged by placing a one-handed 70% alcohol dispenser on the IV pole to the left of the provider. [23••] Thus, to augment perioperative provider hand hygiene, an evidence-based approach includes hand sanitizer placement in proximity to the provider. [3, 23••, 61] Double gloving during induction allows the anesthesia provider to reduce environmental contamination by removing the outer glove to sheathe the laryngoscope blade which serves as a vector to both patients and providers. [62]
The Operative Environment
Hand hygiene improvement initiatives are directly tied to environmental cleaning, as hand hygiene noncompliance correlates with peaks in environmental contamination occurring during induction and emergence of anesthesia, and environmental contamination is linked to contaminated provider hands. [61, 63] It is important to maintain clean and dirty areas within the AWE. [59] Based on a proven multifaceted approach, we recommend that the following areas be designated as “clean”: IV pole to left of provider, IV stopcock set, all medication syringes and the anesthesia supply/medication cart. Similarly, following areas should be designated as “dirty”: the IV pole to the right of the provider, the anesthesia machine, and computer screens attached. Further, a specific area should be designated for storage of contaminated airway instruments (laryngoscope blades and handles). For example, a wire basket with zip closure bag on the IV pole to the right of the provider or a kidney emesis basin on the shelf of the anesthesia machine. [23••]
Following induction of anesthesia and patient stabilization, it is recommended that the anesthesia provider wipe down any surfaces that the provider interacted with following his/her interaction with the patient (stethoscope, anesthesia machine, computer, ventilation bag), with disinfection wipes that contain quaternary ammonium compound and alcohol. SARS-CoV-2 antiseptic effect will be achieved with 30% alcohol. [24••] Single-dose containers should only be used once for a single procedure on a single patient and the use of multi-dose vials should be limited, to prevent transmission of viral diseases like HCV from the surrounding environment to the multi-dose vial. [64]
Poor attention to intraoperative vascular care is a well-documented source of bacterial transmission that results in HAIs. The aim is to maintain an aseptic interface between medication syringes and IV stopcock ports. Use of closed lumen IV systems during perioperative care is recommended as these have been shown to decrease IV pathogen contamination when compared to open lumen systems. [65] Alcohol-impregnated disinfection caps are to be placed on IV lumens until use and replaced when syringes are not in place on the lumen. Use of a disinfection workstation for improving intravascular device disinfection (DOCit™ and HubScrub™ devices-Braun Medical Inc) optimizes aseptic medication administration. [23••]
Effective surface disinfection of the operating room, between operative cases and during terminal cleaning at end of day, is critical. A key component to this is routine assessment of whether or not current disinfection strategies are adequate. This can be achieved by use of evidence-based OR PathTrac surveillance that will also provide guidance for strategic use of UV-C, or it is equivalent, for augmentation of surface disinfection. [23••, 24••, 35, 66••, 67, 68, 69]
The Operative Patient
Extensive evidence shows the impact of preoperative patient decolonization across multiple surgical patient populations. [70] Preoperative patient decolonization has historically targeted known carriers of Staphylococcus aureus using intranasal mupirocin, and now, intranasal povidone-iodine has emerged as an alternative. [71, 72] Most authorities (such as the Society for Healthcare Epidemiology of America and the Infectious Disease Society of America) have been inconclusive in their recommendations whether bathing with antiseptic soap (i.e., chlorhexidine) prevents SSI. [73] That being said, the use of chlorhexidine soap preoperatively is recommended for total joint surgery. A randomized trial incorporating preoperative use of povidone iodine chlorhexidine gluconate as part of a multifaceted approach generated substantial reductions in Staphylococcus aureus transmission and SSIs. [23••] These agents are also effective antiseptics for SARS-CoV-2, and by addressing the patient reservoir, these may help to attenuate further environmental contamination and fomite spread to patients and providers. [24••, 35, 74•]
Preoperative patient decolonization for all surgical patients should include (a) use of 2% chlorhexidine gluconate wipes to the entire body, (b) 0.12% chlorhexidine gluconate oral mouthwash swish and spit, and (c) intranasal povidone-iodine treatment. Given evidence that infants younger than 2 months of age are at risk for skin burns when exposed to chlorhexidine, this antiseptic should be avoided in this population. [75]
Importance of Surveillance
All of the above interventions are behavioral and therefore prone to early fatigue and/or failure. The multifaceted approach described above was only effective after data feedback generated by OR PathTrac surveillance. Further, specific contributions of a particular vector and thus the particular intervention may differ in different institutions. For example, hand hygiene by anesthesia providers may be particularly poor at one hospital while aseptic IV care may be subpar at another. [23••] Hence, one must first assess baseline pathogen burden and modes of transmission. The use of validated surveillance failure mode analysis (OR PathTrac™, RDB Bioinformatics) is key to this process. [66••] This can be used to determine reservoirs that are temporally associated with pathogen transmission events thus providing targets for improvement. [6, 67] Furthermore, failure mode analysis can be used to regularly evaluate the initial impact of improvement strategies and the fidelity of those strategies over time. Contamination can help mitigate human factors known to limit the impact of environmental surface cleaning alone. [76, 77] An effective sampling strategy for OR PathTrac analysis has been delineated. [67] A 5-step strategy with simple interventions to decrease the incidence of HAI has been described in Table 2.
Conclusion
In summary, the role of anesthesia providers and surrounding reservoirs in transmission of infectious pathogens and infection development has been clearly delineated over the last decade. Anesthesia providers, historical and current leaders in patient safety, are poised to lead a national dissemination of an evidence-based, best practice for perioperative infection control as outlined above. In addition to reducing the incidence of SSIs, these measures can be used to help prevent the perioperative spread of viral pathogens such as SARS-CoV-2 in the COVID-19 era. This will improve both patient and provider safety.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Markel H. In 1850, Ignaz Semmelweis saved lives with three words: wash your hands. 2015.
Control CfD, Prevention N. Personnel. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32:470–85.
Koff MD, Brown JR, Marshall EJ, O'Malley AJ, Jensen JT, Heard SO, et al. Frequency of hand decontamination of intraoperative providers and reduction of postoperative healthcare-associated infections: a randomized clinical trial of a novel Hand hygiene system. Infect Control Hosp Epidemiol. 2016;37(8):888–95. https://doi.org/10.1017/ice.2016.106.
•• Loftus RW, Campos JH. The anaesthetists' role in perioperative infection control: what is the action plan? Br J Anaesth. 2019;123(5):531–4. https://doi.org/10.1016/j.bja.2019.07.013This paper discusses the utility the evidence-based tools to achieve perioperative improvements in intravascular catheter design and handling, improved hand hygiene compliance, improved environmental cleaning, and perioperative patient decolonization.
Loftus RW, Koff MD, Brown JR, Patel HM, Jensen JT, Reddy S, et al. The epidemiology of Staphylococcus aureus transmission in the anesthesia work area. Anesth Analg. 2015;120(4):807–18. https://doi.org/10.1213/ANE.0b013e3182a8c16a.
•• Loftus RW, Dexter F, Robinson ADM. High-risk Staphylococcus aureus transmission in the operating room: a call for widespread improvements in perioperative hand hygiene and patient decolonization practices. Am J Infect Control. 2018;46(10):1134–41. https://doi.org/10.1016/j.ajic.2018.04.211 This paper associated transmission of Staphylococcus aureus with provider hands and also demonstrated that improved compliance with hand hygiene and patient decolonization may help to control the spread of these dangerous pathogens.
Roy RC, Brull SJ, Eichhorn JH. Surgical site infections and the anesthesia professionals' microbiome: we've all been slimed! Now what are we going to do about it? Anesth Analg. 2011;112(1):4–7. https://doi.org/10.1213/ANE.0b013e3181fe4942.
National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32(8):470–85. doi: https://doi.org/10.1016/s0196655304005425.
Rupp ME, Fitzgerald T, Puumala S, Anderson JR, Craig R, Iwen PC, et al. Prospective, controlled, cross-over trial of alcohol-based hand gel in critical care units. Infect Control Hosp Epidemiol. 2008;29(1):8–15. https://doi.org/10.1086/524333.
Konvalinka A, Errett L, Fong IW. Impact of treating Staphylococcus aureus nasal carriers on wound infections in cardiac surgery. J Hosp Infect. 2006;64(2):162–8. https://doi.org/10.1016/j.jhin.2006.06.010.
Caffau S, Nadali L. On the bacterial contamination of anesthetic equipment. Friuli Med. 1965;20(4):515–31.
Friis H, Helms P. Bacterial contamination of anesthetic equipment during use. Ugeskr Laeger. 1963;125:619–23.
Madar R, Novakova E, Baska T. The role of non-critical health-care tools in the transmission of nosocomial infections. Bratisl Lek Listy. 2005;106(11):348–50.
Fukada T, Tachibana C, Tsukazaki Y, Satoh K, Furuya Y, Ohe Y. Bacterial contamination of anesthesiologists' hands and the efficacy of handwashing. Masui. 1996;45(8):1026–30.
Loftus RW, Koff MD, Burchman CC, Schwartzman JD, Thorum V, Read ME, et al. Transmission of pathogenic bacterial organisms in the anesthesia work area. Anesthesiology. 2008;109(3):399–407. https://doi.org/10.1097/ALN.0b013e318182c855.
Loftus RW, Brown JR, Koff MD, Reddy S, Heard SO, Patel HM, et al. Multiple reservoirs contribute to intraoperative bacterial transmission. Anesth Analg. 2012;114(6):1236–48. https://doi.org/10.1213/ANE.0b013e31824970a2.
Songjie, Wu YW, Jin X, Tian J, Liu J, Mao Y. Environmental contamination by SARS-CoV-2 in a designated hospital for coronavirus disease. American Journal of Infection Control. 2020. https://doi.org/10.1016/j.ajic.2020.05.003.
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 162020:1564–7.
Apostolou A, Bartholomew ML, Greeley R, Guilfoyle SM, Gordon M, Genese C, et al. Transmission of hepatitis C virus associated with surgical procedures - New Jersey 2010 and Wisconsin 2011. MMWR Morb Mortal Wkly Rep. 2015;64(7):165–70.
Branch-Elliman W, Weiss D, Balter S, Bornschlegel K, Phillips M. Hepatitis C transmission due to contamination of multidose medication vials: summary of an outbreak and a call to action. Am J Infect Control. 2013;41(1):92–4. https://doi.org/10.1016/j.ajic.2012.01.022.
DeMaria A Jr, Snydman DR. Nosocomial hepatitis C: more of a hidden epidemic. Ann Intern Med. 2012;7. United States:534–5.
Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D. Prevention of central line-associated bloodstream infections through quality improvement interventions: a systematic review and meta-analysis. Clin Infect Dis. 2014;59(1):96–105. https://doi.org/10.1093/cid/ciu239.
•• Loftus RW, Dexter F, Goodheart MJ, Mcdonald M, Keech J, Noiseux N, et al. The effect of improving basic preventive measures in the perioperative arena on Staphylococcus aureus transmission and surgical site infections: a randomized clinical trial. JAMA Netw Open. 2020;3(3):e201934. https://doi.org/10.1001/jamanetworkopen.2020.1934 This randomized clinical trial demonstrated that improved basic preventive measures in the perioperative arena can reduce Staphylococcus aureus transmission and surgical site infections.
•• Dexter F, Parra MC, Brown JR, Loftus RW. Perioperative COVID-19 defense: an evidence-based approach for optimization of infection control and operating room management. Anesth Analg. 2020. https://doi.org/10.1213/ANE.0000000000004829 This paper describes an evidence-based approach for optimization of infection control and operating room management during the COVID-19 pandemic.
Helms B, Dorval S, Laurent PS, Winter M. Improving hand hygiene compliance: a multidisciplinary approach. Am J Infect Control. 2010;38(7):572–4. https://doi.org/10.1016/j.ajic.2009.08.020.
Biddle C, Shah J. Quantification of anesthesia providers' hand hygiene in a busy metropolitan operating room: what would Semmelweis think? Am J Infect Control. 2012;40(8):756–9. https://doi.org/10.1016/j.ajic.2011.10.008.
Tait AR, Tuttle DB. Preventing perioperative transmission of infection: a survey of anesthesiology practice. Anesth Analg. 1995;80(4):764–9. https://doi.org/10.1097/00000539-199504000-00020.
Munoz-Price LS, Lubarsky DA, Arheart KL, Prado G, Cleary T, Fajardo-Aquino Y, et al. Interactions between anesthesiologists and the environment while providing anesthesia care in the operating room. Am J Infect Control. 2013;41(10):922–4. https://doi.org/10.1016/j.ajic.2013.03.306.
Munoz-Price LS, Birnbach DJ, Lubarsky DA, Arheart KL, Fajardo-Aquino Y, Rosalsky M, et al. Decreasing operating room environmental pathogen contamination through improved cleaning practice. Infect Control Hosp Epidemiol. 2012;33(9):897–904. https://doi.org/10.1086/667381.
Fernandez PG, Loftus RW, Dodds TM, Koff MD, Reddy S, Heard SO, et al. Hand hygiene knowledge and perceptions among anesthesia providers. Anesth Analg. 2015;120(4):837–43. https://doi.org/10.1213/ANE.0000000000000408.
Walter CW, Kundsin RB, Harding AL, Page LK. The infector on the surgical team. Clin Neurosurg. 1966;14:361–79. https://doi.org/10.1093/neurosurgery/14.cn_suppl_1.361.
Schaffner W, Lefkowitz LB Jr, Goodman JS, Koenig MG. Hospital outbreak of infections with group a streptococci traced to an asymptomatic anal carrier. N Engl J Med. 1969;280(22):1224–5. https://doi.org/10.1056/nejm196905292802209.
Paul SM, Genese C, Spitalny K. Postoperative group A beta-hemolytic Streptococcus outbreak with the pathogen traced to a member of a healthcare worker's household. Infect Control Hosp Epidemiol. 1990;11(12):643–6. https://doi.org/10.1086/646115.
Loftus RW, Dexter F, Robinson ADM, Horswill AR. Desiccation tolerance is associated with Staphylococcus aureus hypertransmissibility, resistance and infection development in the operating room. J Hosp Infect. 2018;100(3):299–308. https://doi.org/10.1016/j.jhin.2018.06.020.
Dexter F, Elhakim M, Loftus RW, Seering MS, Epstein RH. Strategies for daily operating room management of ambulatory surgery centers following resolution of the acute phase of the COVID-19 pandemic. J Clin Anesth. 2020;64:109854. https://doi.org/10.1016/j.jclinane.2020.109854.
Lipp A, Edwards P. Disposable surgical face masks for preventing surgical wound infection in clean surgery. Cochrane Database Syst Rev. 2014;(2):Cd002929. https://doi.org/10.1002/14651858.CD002929.pub2.
Bae S, Kim MC, Kim JY, Cha HH, Lim JS, Jung J, et al. Effectiveness of surgical and cotton masks in blocking SARS-CoV-2: a controlled comparison in 4 patients. Ann Intern Med. 2020. https://doi.org/10.7326/M20-1342.
Hidron AI, Edwards JR, Patel J, Horan TC, Sievert DM, Pollock DA, et al. NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006-2007. Infect Control Hosp Epidemiol. 2008;29(11):996–1011. https://doi.org/10.1086/591861.
Beezhold DW, Slaughter S, Hayden MK, Matushek M, Nathan C, Trenholme GM, et al. Skin colonization with vancomycin-resistant enterococci among hospitalized patients with bacteremia. Clin Infect Dis. 1997;24(4):704–6. https://doi.org/10.1093/clind/24.4.704.
Hayden MK, Blom DW, Lyle EA, Moore CG, Weinstein RA. Risk of hand or glove contamination after contact with patients colonized with vancomycin-resistant enterococcus or the colonized patients' environment. Infect Control Hosp Epidemiol. 2008;29(2):149–54. https://doi.org/10.1086/524331.
Loftus RW, Brown JR, Patel HM, Koff MD, Jensen JT, Reddy S, et al. Transmission dynamics of gram-negative bacterial pathogens in the anesthesia work area. Anesth Analg. 2015;120(4):819–26. https://doi.org/10.1213/ane.0000000000000626.
Bitkover CY, Marcusson E, Ransjö U. Spread of coagulase-negative staphylococci during cardiac operations in a modern operating room. Ann Thorac Surg. 2000;69(4):1110–5. https://doi.org/10.1016/s0003-4975(99)01432-0.
Schweizer ML, Chiang HY, Septimus E, Moody J, Braun B, Hafner J, et al. Association of a bundled intervention with surgical site infections among patients undergoing cardiac, hip, or knee surgery. Jama. 2015;313(21):2162–71. https://doi.org/10.1001/jama.2015.5387.
Lutz CT, Bell CE Jr, Wedner HJ, Krogstad DJ. Allergy testing of multiple patients should no longer be performed with a common syringe. N Engl J Med. 1984;310(20):1335–7. https://doi.org/10.1056/nejm198405173102024.
Fleming A, Ogilvie AC. Syringe needles and mass inoculation technique. Br Med J. 1951;1(4706):543–6. https://doi.org/10.1136/bmj.1.4706.543.
Koepke JW, Selner JC. Allergy testing of multiple patients with a common syringe. N Engl J Med. 1984;311(18):1188–9. https://doi.org/10.1056/nejm198411013111820.
Blogg CE, Ramsay MA, Jarvis JD. Infection hazard from syringes. Br J Anaesth. 1974;46(4):260–2. https://doi.org/10.1093/bja/46.4.260.
Veber B, Gachot B, Bedos JP, Wolff M. Severe sepsis after intravenous injection of contaminated propofol. Anesthesiology. 1994;80(3):712–3. https://doi.org/10.1097/00000542-199403000-00050.
Kuehnert MJ, Webb RM, Jochimsen EM, Hancock GA, Arduino MJ, Hand S, et al. Staphylococcus aureus bloodstream infections among patients undergoing electroconvulsive therapy traced to breaks in infection control and possible extrinsic contamination by propofol. Anesth Analg. 1997;85(2):420–5. https://doi.org/10.1097/00000539-199708000-00031.
Gutelius B, Perz JF, Parker MM, Hallack R, Stricof R, Clement EJ, et al. Multiple clusters of hepatitis virus infections associated with anesthesia for outpatient endoscopy procedures. Gastroenterology. 2010;139(1):163–70. https://doi.org/10.1053/j.gastro.2010.03.053.
Foweraker JE. The laryngoscope as a potential source of cross-infection. J Hosp Infect. 1995;4. England:315–6.
Maslyk PA, Nafziger DA, Burns SM, Bowers PR. Microbial growth on the anesthesia machine. Aana j. 2002;70(1):53–6.
Olds JW, Kisch AL, Eberle BJ, Wilson JN. Pseudomonas aeruginosa respiratory tract infection acquired from a contaminated anesthesia machine. Am Rev Respir Dis. 1972;105(4):628–32. https://doi.org/10.1164/arrd.1972.105.4.628.
Albrecht WH, Dryden GE. Five-year experience with the development of an individually clean anesthesia system. Anesth Analg. 1974;53(1):24–8.
Dryden GE. Risk of contamination from the anesthesia circle absorber: an evaluation. Anesth Analg. 1969;48(6):939–43.
Leijten DT, Rejger VS, Mouton RP. Bacterial contamination and the effect of filters in anaesthetic circuits in a simulated patient model. J Hosp Infect. 1992;21(1):51–60. https://doi.org/10.1016/0195-6701(92)90153-d.
Edmiston CE Jr, Seabrook GR, Cambria RA, Brown KR, Lewis BD, Sommers JR, et al. Molecular epidemiology of microbial contamination in the operating room environment: is there a risk for infection? Surgery. 2005;138(4):573–9; discussion 9-82. https://doi.org/10.1016/j.surg.2005.06.045.
van Vlymen JM, Magnus J, Jaeger M, Breton S, Taylor NG, Phelan R, et al. Hepatitis C contamination of medication vials accessed with sterile needles and syringes. Anesthesiology. 2019;131(2):305–14. https://doi.org/10.1097/aln.0000000000002772.
Clark C, Taenzer A, Charette K, Whitty M. Decreasing contamination of the anesthesia environment. Am J Infect Control. 2014;42(11):1223–5. https://doi.org/10.1016/j.ajic.2014.07.016.
Muffly MK, Beach ML, Tong YC, Yeager MP. Stopcock lumen contamination does not reflect the full burden of bacterial intravenous tubing contamination: analysis using a novel injection port. Am J Infect Control. 2010;38(9):734–9. https://doi.org/10.1016/j.ajic.2010.03.014.
Rowlands J, Yeager MP, Beach M, Patel HM, Huysman BC, Loftus RW. Video observation to map hand contact and bacterial transmission in operating rooms. Am J Infect Control. 2014;42(7):698–701. https://doi.org/10.1016/j.ajic.2014.02.021.
Birnbach DJ, Rosen LF, Fitzpatrick M, Carling P, Arheart KL, Munoz-Price LS. A new approach to pathogen containment in the operating room: sheathing the laryngoscope after intubation. Anesth Analg. 2015;121(5):1209–14. https://doi.org/10.1213/ANE.0000000000000854.
Loftus RW, Muffly MK, Brown JR, Beach ML, Koff MD, Corwin HL, et al. Hand contamination of anesthesia providers is an important risk factor for intraoperative bacterial transmission. Anesth Analg. 2011;112(1):98–105. https://doi.org/10.1213/ANE.0b013e3181e7ce18.
Siegel JD, Rhinehart E, Jackson M, Chiarello L, Committee HCICPA. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35(10):S65–S164.
Loftus RW, Patel HM, Huysman BC, Kispert DP, Koff MD, Gallagher JD, et al. Prevention of intravenous bacterial injection from health care provider hands: the importance of catheter design and handling. Anesth Analg. 2012;115(5):1109–19. https://doi.org/10.1213/ANE.0b013e31826a1016.
•• Robinson ADM, Dexter F, Renkor V, Reddy S, Loftus RW. Operating room PathTrac analysis of current intraoperative Staphylococcus aureus transmission dynamics. Am J Infect Control. 2019;47(10):1240–7. https://doi.org/10.1016/j.ajic.2019.03.028 This prospective cohort study linked the risk of exposure to Staphylococcus aureus to patients skin sites and provider hand, highlighting the importance of both patient decolonization as well as provider hand hygiene.
Dexter F, Epstein RH, Gostine AL, Penning DH, Loftus RW. Benefit of systematic selection of pairs of cases matched by surgical specialty for surveillance of bacterial transmission in operating rooms. Am J Infect Control. 2019;48:682–7. https://doi.org/10.1016/j.ajic.2019.09.025.
Pavia M, Simpser E, Becker M, Mainquist WK, Velez KA. The effect of ultraviolet-C technology on viral infection incidence in a pediatric long-term care facility. Am J Infect Control. 2018;46(6):720–2. https://doi.org/10.1016/j.ajic.2018.01.014.
Andersen BM, Bånrud H, Bøe E, Bjordal O, Drangsholt F. Comparison of UV C light and chemicals for disinfection of surfaces in hospital isolation units. Infect Control Hosp Epidemiol. 2006;27(7):729–34. https://doi.org/10.1086/503643.
Schweizer M, Perencevich E, McDanel J, Carson J, Formanek M, Hafner J, et al. Effectiveness of a bundled intervention of decolonization and prophylaxis to decrease Gram positive surgical site infections after cardiac or orthopedic surgery: systematic review and meta-analysis. Bmj. 2013;346:f2743. https://doi.org/10.1136/bmj.f2743.
Vasquez JE, Walker ES, Franzus BW, Overbay BK, Reagan DR, Sarubbi FA. The epidemiology of mupirocin resistance among methicillin-resistant Staphylococcus aureus at a Veterans' Affairs hospital. Infect Control Hosp Epidemiol. 2000;21(7):459–64. https://doi.org/10.1086/501788.
Anderson MJ, David ML, Scholz M, Bull SJ, Morse D, Hulse-Stevens M, et al. Efficacy of skin and nasal povidone-iodine preparation against mupirocin-resistant methicillin-resistant Staphylococcus aureus and S. aureus within the anterior nares. Antimicrob Agents Chemother. 2015;59(5):2765–73. https://doi.org/10.1128/aac.04624-14.
Anderson DJ, Podgorny K, Berríos-Torres SI, Bratzler DW, Dellinger EP, Greene L, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(6):605–27. https://doi.org/10.1086/676022.
• Loftus RW, Dexter F, Parra MC, Brown JR. Importance of oral and nasal decontamination for patients undergoing anesthetics during the COVID-19 era. Anesth Analg. 2020. https://doi.org/10.1213/ANE.0000000000004854 This paper discusses the favorable risk/benefit profile of patient decolonization with nasal povidone and oral chlorhexidine rinse to help mitigate the perioperative spread of COVID-19.
Chapman AK, Aucott SW, Milstone AM. Safety of chlorhexidine gluconate used for skin antisepsis in the preterm infant. J Perinatol. 2012;32(1):4–9. https://doi.org/10.1038/jp.2011.148.
Murrell LJ, Hamilton EK, Johnson HB, Spencer M. Influence of a visible-light continuous environmental disinfection system on microbial contamination and surgical site infections in an orthopedic operating room. Am J Infect Control. 2019;47(7):804–10. https://doi.org/10.1016/j.ajic.2018.12.002.
Anderson DJ, Gergen MF, Smathers E, Sexton DJ, Chen LF, Weber DJ, et al. Decontamination of targeted pathogens from patient rooms using an automated ultraviolet-C-emitting device. Infect Control Hosp Epidemiol. 2013;34(5):466–71. https://doi.org/10.1086/670215.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Archit Sharma declares that he has no conflicts of interest. Patrick G. Fernandez declares that he has no conflicts of interest. John P. Rowlands declares that he has no conflicts of interest. Matthew D. Koff is a minor shareholder of RDB Bioinformatics (Coralville, Iowa, USA). Randy W. Loftus is supported by the Anesthesia Patient Safety Foundation, and has previously received grant funding from Sage Medical and Draeger; has served as a guest speaker at education meetings sponsored by Kenall (Indigo-Clean, AORN) and BBraun (APIC); is founder a shareholder of RDB Bioinformatics, which owns OR PathTrac; and is a co-inventor on two pending patents (PCT/US2017/026557 and 62/682,267 - Method and system for differentiating more pathogenic S. aureus Strains among commonly isolated intraoperative multilocus sequence type).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Patient Safety in Anesthesia
Appendix
Appendix
A figure displaying different levels and frequency of patient-provider-environmental interactions for anesthesia providers during routine, elective surgery. The figure represents interactions during an elective surgical case of approximately 3 h in duration. Each line represents one provider-patient-environmental interaction. Red lines represent the anesthesia team, blue lines represent the surgical team, and black lines represent the circulating nurse. This depicts a high task density work environment for anesthesia providers (picture published with permission from John P. Rowlands, MD)
Rights and permissions
About this article
Cite this article
Sharma, A., Fernandez, P.G., Rowlands, J.P. et al. Perioperative Infection Transmission: the Role of the Anesthesia Provider in Infection Control and Healthcare-Associated Infections. Curr Anesthesiol Rep 10, 233–241 (2020). https://doi.org/10.1007/s40140-020-00403-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-020-00403-8