Abstract
Introduction
Our objective was to describe the contemporary outcomes of orbital atherectomy (OA) vs. rotational atherectomy (RA) use for inpatient percutaneous coronary intervention (PCI) in the United States. Data on the use of OA vs. RA in contemporary inpatient PCI are limited.
Methods
We queried the Nationwide Readmission Database (NRD) from January to November for the years 2016–2017 to identify hospitalizations of patients who underwent PCI with atherectomy. We conducted a multivariate regression analysis to identify variables associated with in-hospital mortality.
Results
We included 77,040 records of patients who underwent inpatient PCI with atherectomy. Of those, 71,610 (93%) had RA, and 5430 (7%) had OA. There was no significant change in the trend of using OA or RA over 2016 and 2017. OA was less utilized in patients presenting with ST-segment elevation myocardial infarction (STEMI) (4.3% vs. 46.8%, p < 0.001). In our cohort, OA was associated with lower in-hospital mortality (3.1% vs. 5%, p < 0.001) and 30-day urgent readmission (< 0.01% vs. 0.2%, p = 0.009), but a higher risk of coronary perforation (1.7% vs. 0.6%, p < 0.001) and cardiac tamponade (1% vs. 0.3%, p < 0.001) and a higher cost of index hospitalization ($28,199 vs. $23,188, p < 0.001) compared with RA.
Conclusion
RA remains the predominant atherectomy modality for inpatient PCI in the United States (93%). There was no change in the trend of use for either modality over the years 2016 and 2017. OA was noted to have a lower incidence of in-hospital death, but a higher risk of coronary perforation and a higher cost of index hospitalization for the overall unmatched cohorts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
RA was the predominant atherectomy tool used for inpatient PCI in 2016 and 2017 in the United States (93%). |
There was no significant change in the trends of using OA or RA for inpatient PCI for 2016 and 2017. |
OA was most likely to be used in large and teaching hospitals and not in the STEMI setting. In unmatched cohorts, despite a higher incidence of coronary perforation and tamponade, OA was associated with a lower incidence of in-hospital mortality. |
OA was associated a lower incidence of 30-day urgent readmission, ischemic stroke, complete heart block, and ventricular tachycardia, but with a higher hospital cost. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13643225
Introduction
Severe coronary artery calcification is a significant risk factor for procedural failure and complications, and long-term adverse events in contemporary percutaneous coronary intervention (PCI) [1,2,3]. The prevalence of moderate to severe calcification in patients undergoing PCI is around 20% angiographically [4]. Different calcium-specific technologies are available to address coronary calcification, including atherectomy devices and, more recently, intravascular lithotripsy, which is yet to be approved for coronary use in the United States [5]. The main contemporary indication of atherectomy devices is the preparation of the vessel for subsequent balloon angioplasty and stenting.
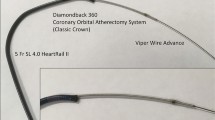
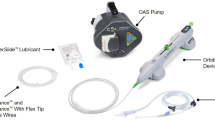
Rotational atherectomy (RA) (Boston Scientific, Natick, MA, USA) has been the traditional modality for treating calcified coronary lesions in the United States for the past three decades. RA uses a rotating abrasive burr at high speeds to ablate and crack superficial calcium [6]. Orbital atherectomy (OA) (Cardiovascular Systems, Inc., St. Paul, MN, USA) was approved in 2013 as an adjunctive tool for PCI in heavily calcified vessels [7]. It uses a drive shaft with an eccentrically mounted crown to perform proximal and distal sanding that is abrasive only to fibrotic and calcified vessels, minimizing damage to the medial layer of the vessel [8]. Both modalities help enlarge the lumen and enhance equipment delivery. We performed a comprehensive analysis of the Nationwide Readmissions Database (NRD) to describe the outcomes of RA and OA.
Methods
Data Source
We used the Nationwide Readmissions Database (NRD) of the Healthcare Cost and Utilization Project (HCUP), Agency for Healthcare Research and Quality, to obtain our cohort [9]. The NRD contains discharge data from 28 geographically dispersed states, accounting for 60.0% of the total US resident population and 58.2% of all US hospitalizations. We identified our cohort, procedures, and outcomes using the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) and Procedure Coding System (ICD-10-PCS) codes along with ICD-10 Clinical Classifications Software (CCS). The codes used are summarized in Table S1.
Study Population
We identified our cohort using the ICD-10 codes for OA and RA used for inpatient PCI for the years 2016 and 2017 (Table S1). Patient and hospital-level variables provided by HCUP NRD were used to identify demographics and baseline characteristics. The Elixhauser method was used to assess comorbidities [10]. Additional comorbidities were identified using appropriate ICD-10-CM codes (Table S1). We excluded patients with missing data on in-hospital mortality, who had combined RA and OA, and whose admission month was December to be able to assess the 30-day readmission rate. The NRD is a publicly available database with de-identified hospitalization records; therefore, the study was exempt from institutional review board evaluation at Banner University Medical Center.
Outcomes
The primary outcome of our study was in-hospital mortality. Secondary outcomes included in-hospital coronary artery bypass graft surgery (CABG), coronary perforation, ischemic or hemorrhagic stroke, vascular complications, renal complications, discharge to a nursing facility, length of hospital stay, the cost of index hospitalization, and non-elective 30-day readmission.
Statistical Analysis
All analyses were conducted using the appropriate weighting, stratifying, and clustering samples following HCUP regulations [11, 12]. Given the extreme heterogeneity between the two groups, we did not perform propensity-score matching and aimed to report outcomes in a descriptive fashion. Continuous variables are summarized as medians and interquartile range (IQR) (25th and 75th percentiles) and compared with the Mann–Whitney U test. Categorical variables are displayed as numbers and percentages and compared with Pearson’s chi-square or Fisher’s exact tests. Outcomes in the matched groups were reported as odds ratios (OR) with a 95% confidence interval (CI). All p values are two-sided, with a significance threshold < 0.05.
We performed a multivariable regression analysis to identify variables associated with in-hospital mortality. We included all variables considered significant based on background knowledge using the Enter method. The list of the variables used is shown in Table S2. Analysis of readmissions was performed for patients without in-hospital death at the index admission. Statistical analysis was performed using IBM SPSS Statistics for Windows (version 25.0; IBM Corp, Armonk, NY). The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Results
Patient Characteristics
We identified 84,401 total weighted hospitalizations for patients who underwent PCI with atherectomy during the study period. After the exclusion of patients who were admitted in December and those with missing in-hospital mortality data, our final cohort included 77,040 hospitalizations (Fig. S1). RA was the predominant modality of atherectomy in 71,610 records (93%), while OA was used in 5430 (7%) of the cases. Differences in demographics, comorbidities, and hospital characteristics between the OA and RA groups are shown in Table 1. Over 2016 and 2017, there was no significant change in the trends of using OA (p trend = 0.35) or RA (p trend = 0.24) (Fig. 1).
Median patient age was 65 (IQR 56–74) years, and 29.2% were women. Of these patients, about 43.8% presented with ST-elevation myocardial infarction (STEMI). PCI of bifurcation lesions occurred in 3.8%. Impella was used in 4% of records, while intra-aortic balloon pump was used in 7.1%. Intravascular imaging was used in 9.8% of cases (intravascular ultrasound [IVUS] in 9.2% and optical coherence tomography [OCT] in 0.6%).
Patients who had OA were older (73 vs. 64 years, p < 0.001) and were more likely to be women (36.8% vs. 28.6%, p < 0.01). OA was significantly less utilized in patients presenting with STEMI (4.3% vs. 46.8%, p < 0.01), and more utilized in patients with prior CABG (12% vs. 8.9%, p < 0.01), bifurcation lesions (5.4% vs. 3.7%, p < 0.01). Both Impella (7.5% vs. 3.8%, p < 0.01) and intravascular imaging including IVUS (13.5% vs. 9.5%, p < 0.01) and OCT (2.3% vs. 0.5%, p < 0.01) were more likely to be used with OA. OA was more used in large (68.2% vs. 63%, p < 0.01) and teaching hospitals (79.7% vs. 70.1%, p < 0.01).
Outcomes
Study outcomes are summarized in Table 2. The incidence of in-hospital mortality and cardiogenic shock was 4.9% and 10.8%, respectively. The incidence of ischemic and hemorrhagic strokes was 0.9% and 0.3%, respectively. Coronary perforation occurred in 0.7%. The incidence of 30-day urgent readmission was 0.2%.
OA was associated with a lower incidence of in-hospital mortality (3.1% vs. 5%, p < 0.01), in-hospital CABG (1.4% vs. 1.9%, p = 0.029), discharge to a facility (7.1% vs. 11.5%, p < 0.01), and 30-day urgent readmissions (0% vs. 0.2%, p = 0.01). However, it was associated with a higher incidence of coronary perforation (1.7% vs. 0.6%, p < 0.01) and cardiac tamponade (1% vs. 0.3%, p < 0.01). OA was also associated with a slightly longer LOS (4 vs. 3 days, p < 0.01) and higher cost of index hospitalization ($28,199 vs. $23,188, p < 0.01) compared with RA. On multivariable regression analysis, OA was associated with a lower incidence of in-hospital mortality (OR 0.651, 95% CI [0.540–0.784], p < 0.01). Variables associated with in-hospital mortality are shown in Table S3.
Discussion
The main findings of the study can be summarized as follows: (1) RA was the predominant atherectomy tool used for inpatient PCI in 2016 and 2017 in the United States (93%). (2) There was no significant change in the trends of using OA or RA for inpatient PCI for 2016 and 2017. (3) OA was most likely to be used in large and teaching hospitals and not in the STEMI setting. (4) In unmatched cohorts, despite a higher incidence of coronary perforation and tamponade, OA was associated with a lower incidence of in-hospital mortality, 30-day urgent readmission, ischemic stroke, complete heart block, and ventricular tachycardia, but with a longer LOS and a higher cost of index hospitalization, compared with RA.
Coronary artery calcification is associated with a higher risk of target lesion revascularization (TLR) and major adverse cardiovascular events (MACE) after PCI, even with newer-generation drug-eluting stents (DES) [13]. RA has been the primary modality used to deal with calcified arteries, although improvement of long-term outcomes with this device has not been demonstrated [14]. The approval of the Diamondback 360 OA system in 2013 introduced a new tool in the armamentarium of the interventional cardiologist against coronary calcification. In the ORBIT II “Evaluate the Safety and Efficacy of OAS in Treating Severely Calcified Coronary Lesions” trial, OA use was associated with a low incidence of TLR up to 3 years (7.8%), but the study lacked a control arm [15]. Both devices are currently used in contemporary practice to treat coronary calcification. In our analysis, the predominant atherectomy modality was RA (93%), which can be attributed to the comfort level, lower cost, and experience of operators in using the device as well as the lack of randomized data for the OA system.
In our matched cohort and after robust multivariate regression analysis, the OA system was associated with reduced risk of in-hospital mortality, which is similar to the results of the largest study to date comparing the two modalities [16]. This finding, however, should be interpreted with extreme caution given the retrospective nature and the risk of selection bias in our study. In our analysis, OA was also associated with a lower risk of ischemic stroke, ventricular tachycardia, and complete heart block. The lower in-hospital mortality with OA can be secondary to the lower incidence of periprocedural myocardial infarction (MI) with OA compared with RA that was demonstrated by Meraj et al. [16]. RA uses a burr that is always in contact with the plaque, not allowing blood and debris to flow beyond the burr, increasing the risk of thermal injury, platelet activation, distal ischemia, no-reflow phenomenon, and periprocedural MI. On the contrary, OA crown allows blood and particulates to flow during and between activations, reducing the risk of ischemia, distal embolization, and complete heart block. The other possible explanation is the higher risk of burr entrapment of RA, as the RA only ablates in an antegrade fashion, increasing the risk of burr entrapment. The bidirectional ablation ability with the OA, combined with the small crown size, minimizes the risk of crown entrapment.
In our analysis, OA was associated with a higher risk of coronary perforation and pericardial tamponade, which was not previously detected in studies comparing the two modalities [16, 17]. These studies, however, demonstrated a strong trend towards a higher risk of perforation with OA but were not powerful enough to show statistical significance with such a rare clinical event [17]. The higher risk of perforation with OA can have multiple explanations. First, OA results in more modification of the plaque with longer cuts and deeper dissections compared with RA, as shown by intravascular imaging [18]. Second, in the ORBIT II study, vessels smaller than 2.5 mm were excluded as the 1.25 mm crown might lead to perforation in such small vessels. It is possible that in real-life, operators used OA for smaller vessels leading to more perforations. Finally, operators might opt to use OA rather than RA in vessels with eccentric calcific plaques. In eccentric plaques, the wire bias can be exaggerated and using RA in these circumstances increases the risk of asymmetric ablation, burr entrapment and vessel perforation. These risks are reduced with OA as the orbital movement of the crown may overcome these issues. However, the preferential use of OA in eccentric plaques that are already a risk factor of perforation might lead to increased risk of perforation with OA in a non-randomized real-world study like ours.
OA is more efficient to use because it is easier to set up than RA, and the ViperWire can be used to deliver equipment, in contrast to the ROTAWire, which may not provide enough support. Moreover, the ViperWire is easier to use for primary lesion crossing than the ROTAWire, which requires crossing the lesion with a workhorse wire, then exchange through a microcatheter or over the wire balloon. This was reflected in reduced fluoroscopy time with OA compared with RA in prior studies [16, 17]. The luminal gain with RA is related to the burr size, and if a larger lumen is needed, more devices are required, which can be costly and time-consuming. Moreover, the larger burrs (1.75 mm) require 7F guiding catheters, which can be challenging to use in certain situations (e.g., radial approach in patients with smaller radial arteries). Conversely, with OA, increasing the speed of rotation and slowing advancement can help achieve larger luminal gains without the need to exchange the device, and it can be done through a 6F guiding catheter [19]. On the other hand, OA has certain limitations, including unclear data regarding use in small (< 2.5 mm) or large (> 4.0 mm) vessels, and limitations in ablation in cases of subtotal occlusion of calcified vessels, as the ablative crown is proximal to the tip. However, a previous report showed the feasibility of OA in that situation [20].
The principal advantage that OA has introduced to the field is that the orbital technology allows the treatment of the entire vessel, removing calcium more effectively and resulting in deeper and longer dissections throughout the entire artery, compared with RA that ablates only a fixed diameter of the vessel according to the burr size [18]. This results in better stent expansion and apposition compared with RA, as shown by intravascular imaging [18]. The anticipated benefit of these findings in terms of improved long-term outcomes and reduction in TLR is yet to be shown in a randomized trial. However, in a study comparing the two modalities in Japan, OA had a significantly lower risk of TLR at one year compared with RA (5.0 vs. 15.7%) [21]. The ECLIPSE [NCT03108456] trial is currently enrolling patients and would shed more light on the long-term outcomes of OA.
A major limitation to the widespread use of OA is the cost. In our analysis, OA was associated with a higher cost of index hospitalization compared with RA ($28,199 vs. $23,188). This can be attributed to the higher cost of the OA device compared with the RA device. Although with OA there is no need to use multiple devices if a larger luminal gain is needed, unlike RA, this still did not translate into a lower cost in our analysis. However, OA was found to be cost-effective in the Japanese healthcare system, given better clinical outcomes at 1 year [21]. Another cost analysis of the ORBIT II trial showed that OA is cost-effective compared with standard treatment and can be cost-saving in the inpatient setting [22]. More studies are needed to establish the clinical efficacy and cost-effectiveness of OA.
Limitations
Our study has limitations. First, the goal of our study is to describe rather than compare the two modalities, given the extreme heterogeneity in both groups and the lack of necessary patient and lesion characteristics required to perform proper propensity-score matching, including severe calcification, eccentric plaque, and tortuosity. Second, our study is a retrospective observational study with its inherent limitation of selection bias. The selection bias may have affected our results, which should be interpreted as descriptive rather than comparative. Third, given the administrative database structure of NRD, the study is subject to coding errors. Fourth, our study describes only inpatient PCIs. Finally, long-term outcomes, including TLR and long-term mortality, could not be analyzed.
Conclusions
RA remains the predominant atherectomy modality for inpatient PCI in the United States (93%). There was no change in the trend of use for either modality over the years 2016 and 2017. Orbital atherectomy was noted to have a lower incidence of in-hospital death, but a higher risk of coronary perforation and a higher cost of index hospitalization for the overall unmatched cohorts.
References
Lee MS, Shah N. The impact and pathophysiologic consequences of coronary artery calcium deposition in percutaneous coronary interventions. J Invasive Cardiol. 2016;28:160–7.
Mosseri M, Satler LF, Pichard AD, Waksman R. Impact of vessel calcification on outcomes after coronary stenting. Cardiovasc Revasc Med. 2005;6:147–53.
Colombo A, Stankovic G. Coronary perforations: old screenplay, new actors! J Invasive Cardiol. 2004;16:302–3.
Lee MS, Yang T, Lasala J, Cox D. Impact of coronary artery calcification in percutaneous coronary intervention with paclitaxel-eluting stents: Two-year clinical outcomes of paclitaxel-eluting stents in patients from the ARRIVE program. Catheter Cardiovasc Interv. 2016;88:891–7.
Ali ZA, Nef H, Escaned J, Werner N, Banning AP, Hill JM, Bruyne BD, Montorfano M, Lefevre T, Stone GW, Crowley A, Matsumura M, Maehara A, Lansky AJ, Fajadet J, Mario CD. Safety and effectiveness of coronary intravascular lithotripsy for treatment of severely calcified coronary stenoses. Circ Cardiovasc Interv. 2019;12:e008434.
Sharma SK, Tomey MI, Teirstein PS, Kini AS, Reitman AB, Lee AC, Généreux P, Chambers JW, Grines CL, Himmelstein SI, Thompson CA, Meredith IT, Bhave A, Moses JW. North American expert review of rotational atherectomy. Circ Cardiovasc Interv. 2019;12:e007448.
Tomey MI, Sharma SK. Interventional options for coronary artery calcification. Curr Cardiol Rep. 2016;18:12.
Sotomi Y, Shlofmitz RA, Colombo A, Serruys PW, Onuma Y. Patient selection and procedural considerations for coronary orbital atherectomy system. Interv Cardiol Rev. 2016;11:33.
Mack MJ, Leon MB, Thourani VH, Makkar R, Kodali SK, Russo M, Kapadia SR, Malaisrie SC, Cohen DJ, Pibarot P. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380:1695–705.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998. https://doi.org/10.1097/00005650-199801000-00004
Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to methodological standards in research using the national inpatient sample. JAMA. 2017;318:2011–8.
12Houchens R, Elixhauser A. Using the HCUP nationwide inpatient sample to estimate trends (updated for 1988–2004). HCUP Method Series Report 2006; 5.
Shiode N, Kozuma K, Aoki J, Awata M, Nanasato M, Tanabe K, Yamaguchi J, Kusano H, Nie H, Kimura T. The impact of coronary calcification on angiographic and 3-year clinical outcomes of everolimus-eluting stents: results of a XIENCE V/PROMUS post-marketing surveillance study. Cardiovasc Interv Therap. 2018;33:313–20.
Abdel-Wahab M, Richardt G, Büttner HJ, Toelg R, Geist V, Meinertz T, Schofer J, King L, Neumann F-J, Khattab AA. High-speed rotational atherectomy before paclitaxel-eluting stent implantation in complex calcified coronary lesions: the randomized ROTAXUS (Rotational Atherectomy Prior to Taxus Stent Treatment for Complex Native Coronary Artery Disease) trial. JACC Cardiovasc Interv. 2013;6:10–9.
Lee M, Généreux P, Shlofmitz R, Phillipson D, Anose BM, Martinsen BJ, Himmelstein SI, Chambers JW. Orbital atherectomy for treating de novo, severely calcified coronary lesions: 3-year results of the pivotal ORBIT II trial. Cardiovasc Revasc Med. 2017;18:261–4.
Meraj PM, Shlofmitz E, Kaplan B, Jauhar R, Doshi R. Clinical outcomes of atherectomy prior to percutaneous coronary intervention: A comparison of outcomes following rotational versus orbital atherectomy (COAP-PCI study). J Interv Cardiol. 2018;31:478–85.
Goel S, Pasam RT, Chava S, Gotesman J, Sharma A, Malik BA, Frankel R, Shani J, Gidwani U, Latib A. Orbital atherectomy versus rotational atherectomy: A systematic review and meta-analysis. Int J Cardiol. 2020;303:16–21.
Kini AS, Vengrenyuk Y, Pena J, Motoyama S, Feig JE, Meelu OA, Rajamanickam A, Bhat AM, Panwar S, Baber U, Sharma SK. Optical coherence tomography assessment of the mechanistic effects of rotational and orbital atherectomy in severely calcified coronary lesions. Catheter Cardiovasc Interv. 2015;86:1024–32.
Chambers JW, Diage T. Evaluation of the Diamondback 360 coronary orbital atherectomy system for treating de novo, severely calcified lesions. Expert Rev Med Devices. 2014;11:457–66.
Megaly M, Brilakis ES. Primary orbital atherectomy for treating a heavily calcified balloon uncrossable lesion. Cardiovasc Revasc Med. 2020 Feb 8. In press.
Pietzsch JB, Geisler BP, Ikeno F. Cost-effectiveness of orbital atherectomy compared to rotational atherectomy in treating patients with severely calcified coronary artery lesions in Japan. Cardiovasc Interv Therap. 2018;33:328–36.
Garrison LP Jr, Zimmermann MR, Young CH, Crittendon J, Genereux P. Cost-effectiveness analysis of the orbital atherectomy system: two-year follow-up. Cardiovasc Revasc Med. 2017;18:86–90.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Santiago Garcia: consultant for SurModics, Osprey Medical, Medtronic, Edwards Lifesciences, and Abbott. Grant support from Edwards Lifesciences and the VA Office of Research and Development. Emmanouil Brilakis: consulting/speaker honoraria from Abbott Vascular, American Heart Association (associate editor Circulation), Amgen, Biotronik, Boston Scientific, Cardiovascular Innovations Foundation (Board of Directors), ControlRad, CSI, Ebix, Elsevier, GE Healthcare, Infraredx, Medtronic, Siemens, and Teleflex; research support from Regeneron and Siemens. Shareholder: MHI Ventures. Ajay J. Kirtane: Institutional funding to Columbia University and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, ReCor Medical. In addition to research grants, institutional funding includes fees paid to Columbia University and/or Cardiovascular Research Foundation for speaking engagements and/or consulting. Personal: Travel Expenses/Meals from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, ReCor Medical, Chiesi, OpSens, Zoll, and Regeneron. Khaldoon Alaswad: consulting/speaker honoraria from Boston Scientific, Cardiovascular Systems Inc, Abbott Vascular, Teleflex. Michael Megaly, Ramy Sedhom, Mariam Tawadros, Ayman Elbadawi, Amgad Mentias and Ashish Pershad have nothing to disclose.
Compliance with Ethics Guidelines
The NRD is a publicly available database with de-identified hospitalization records; therefore, the study was exempt from institutional review board evaluation at Banner University Medical Center.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Megaly, M., Brilakis, E.S., Sedhom, R. et al. Outcomes with Orbital and Rotational Atherectomy for Inpatient Percutaneous Coronary Intervention. Cardiol Ther 10, 229–239 (2021). https://doi.org/10.1007/s40119-021-00214-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-021-00214-w