Abstract
Weight loss, whether achieved by lifestyle intervention, pharmacotherapy, or bariatric surgery, is highly effective as a primary interventional strategy in both the prevention and treatment of type 2 diabetes. In high-risk patients with prediabetes and/or metabolic syndrome, weight loss effectively prevents progression to type 2 diabetes mellitus (T2DM) and improves cardiovascular risk factors. These benefits are the result of improvements in insulin resistance, which is central to the pathophysiology of cardiometabolic disease. In patients with T2DM, weight loss improves glycemia, while reducing the need for conventional glucose-lowering medicines, by affecting all three processes that produce and sustain the hyperglycemic state, namely via increments in peripheral insulin sensitivity with improvements in insulin signal transduction at the cellular level, more robust insulin secretory responses, and reduced rates of hepatic glucose production. In both nondiabetic and diabetic subjects, hypocaloric feeding (e.g., treatment with very low-calorie diet or bariatric surgery) produces a rapid improvement in insulin sensitivity due to mobilization of fat from the intramyocellular, intrahepatocellular, and intra-abdominal compartments, and via a more long-term mechanism that correlates with the loss of total body fat. In diabetes, by improving glycemia, weight loss also enhances glucose homeostasis by reversing the defects in insulin action and secretion attributable to glucose toxicity. Regardless of the therapeutic approach, weight loss of ∼10 % maximally prevents future diabetes in patients with prediabetes or metabolic syndrome. In T2DM, greater degrees of weight loss lead to progressive improvements in glucose homeostasis. Therefore, when accompanied by greater weight loss, the metabolic benefits following bariatric surgery are generally more pronounced than those achieved following lifestyle and medical treatment. In addition, the mechanisms by which bariatric operations improve diabetes may include both weight-dependent and weight-independent mechanisms, and the latter may involve changes in gut hormones, bile acids, or gut microflora.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. J Amer Med Assoc. 2014;311:806–14.
Finkelstein EA, Trogdon JG, Cohen JW, et al. Annual medical spending attributable to obesity: payer-and-service-specific estimates. Health Aff. 2009;28:w822–w31.
Garber AJ, Handelsman Y, Einhorn D, et al. Diagnosis and management of prediabetes in the continuum of hyperglycemia: when do the risks of diabetes begin? A consensus statement from the American College of Endocrinology and the American Association of Clinical Endocrinologists. Endocr Pract. 2008;14:933–46.
American Diabetes Association. Standards of medical care in diabetes—2015. Diabetes Care. 2015;38 Suppl 1:S8–S16.
Grundy SM, Brewer Jr HB, Cleeman JI, American Heart A. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–38.
Eckel R, Grundy S, Zimmet P. The metabolic syndrome. Lancet. 2005;365:1415–28.
Milicevic Z, Raz J, Beattie SD, et al. Natural history of cardiovascular disease in patients with diabetes: role of hyperglycemia. Diabetes Care. 2008;31(2):S155–60.
Van Gaal LF, Mentens IL, De Block CE. Mechanisms linking obesity with cardiovascular disease. Nature. 2006;444:875–80.
Guo F, Moellering DR, Garvey WT. The progression of cardiometabolic disease: validation of a new cardiometabolic disease staging system applicable to obesity. Obesity. 2014;22:110–18.
Nigro J, Osman N, Dart AM, et al. Insulin resistance and atherosclerosis. Endocr Rev. 2006;27:242–59.
Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–46.
Després J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7.
Ärnlöv J, Ingelsson E, Sundström J, et al. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation. 2010;121:230–6.
Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30:753–9.
Rodbard HW, Jellinger PS, Davidson JA, et al. Statement by an American Association of Clinical Endocrinologists/American College of Endocrinology consensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract. 2009;15:540–59.
UKPDS Group. UK prospective diabetes study 7: response of fasting plasma glucose to diet therapy in newly presenting type II diabetic patients. Metabolism. 1990;39:905–12.
Bosello O, Armellini F, Zamboni M, et al. The benefits of modest weight loss in type II diabetes. Int J Obes Relat Metab Disord. 1997;21 Suppl 1:S10–3.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. American association of clinical endocrinologists’ comprehensive diabetes management algorithm 2013 consensus statement—executive summary. Endocr Pract. 2013;19:536–57.
Norris SL, Zhang X, Avenell A, et al. Long-term non-pharmacological weight loss interventions for adults with type 2 diabetes. Cochrane Database Syst Rev. 2005;CD005270.
Li Z, Maglione M, Tu W, et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med. 2005;142:532–46.
Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. the Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–44.
Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Deedwania PC, Volkova N. Current treatment options for the metabolic syndrome. Curr Treat Options Cardiovasc Med. 2005;7:61–74.
Stefan N, Kantartzis K, Machann J, et al. Identification and characterization of metabolically benign obesity in humans. Arch Intern Med. 2008;168:1609–16.
Wildman RP, Muntner P, Reynolds K, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999–2004). Arch Intern Med. 2008;168:1617–24.
Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab. 2006;91:2906–12.
Yusuf S, Hawken S, Ounpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9.
Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29:2102–7.
Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–86.
Laaksonen DE, Lindstrom J, Lakka TA, et al. Physical activity in the prevention of type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes. 2005;54:158–65.
Lindström J, Ilanne-Parikka P, Peltonen M, et al. Finnish Diabetes Prevention Study Group. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368:1673–9.
Li G, Zhang P, Wang J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diab Endocrinol. 2014;2:474–80.
Barte JC, ter Bogt NC, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11:899–906.
Wadden TA, Fujioka K, Toubro S, et al. A randomized trial of lifestyle modification and taranabant for maintaining weight loss achieved with a low-calorie diet. Obesity. 2010;18:2301–10.
Torgerson JS, Hauptman J, Boldrin MN, et al. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care. 2004;27:155–61.
Garvey WT, Ryan DH, Look M, et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr. 2012;95:297–308.
Garvey WT, Ryan DH, Henry R, et al. Prevention of type 2 diabetes in subjects with prediabetes and metabolic syndrome treated with phentermine and topiramate extended release. Diabetes Care. 2014;37:912–21.
Wentworth JM, Hensman T, Playfair J, et al. Laparoscopic adjustable gastric banding and progression from impaired fasting glucose to diabetes. Diabetologia. 2014;57:463–8.
Sjöholm K, Anveden A, Peltonen M, et al. Evaluation of current eligibility criteria for bariatric surgery: diabetes prevention and risk factor changes in the Swedish Obese Subjects (SOS) study. Diabetes Care. 2013;36:1335–40.
Carlsson LM, Peltonen M, Ahlin S, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish Obese Subjects. N Engl J Med. 2012;367:695–704.
Magliano DJ, Barr EL, Zimmet PZ, et al. Glucose indices, health behaviors, and incidence of diabetes in Australia: the Australian Diabetes, Obesity and Lifestyle study. Diabetes Care. 2008;31:267–72.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. J Amer Med Assoc. 2012;307:56–65.
Booth H, Khan O, Prevost T, et al. Incidence of type 2 diabetes after bariatric surgery: population-based matched cohort study. Lancet Diab Endocrinol. 2014;2:963–8. This study demonstrates that bariatric surgery is associated with a reduced incidence of T2DM in patients with obesity.
Guare JC, Wing RR, Grant A. Comparison of obese NIDDM and nondiabetic women: short- and long-term weight loss. Obes Res. 1995;3:329–35.
Wing RR, Marcus MD, Epstein LH, et al. Type II diabetic subjects lose less weight than their overweight nondiabetic spouses. Diabetes Care. 1987;10:563–6.
Henry RR, Chilton R, Garvey WT. New options for the treatment of obesity and type 2 diabetes mellitus (narrative review). J Diab Complic. 2013;27:508–18.
Wing RR, Lang W, Wadden TA, The Look AHEAD Research Group, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–6.
Group TLAR, Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170:1566–75.
Belalcazar LM, Haffner SM, Lang W, et al. Lifestyle intervention and/or statins for the reduction of C-reactive protein in type 2 diabetes: from the look AHEAD study. Obesity. 2013;21:944–50.
Look AHEAD Research Group, Wing RR, Bolin P, Brancati FL, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–54.
Gregg EW, Chen H, Wagenknecht LE, Look AHEAD Research Group, et al. Association of an intensive lifestyle intervention with remission of type 2 diabetes. J Amer Med Assoc. 2012;308:2489–96.
Foster GD, Borradaile KE, Sanders MH, for the Sleep AHEAD Research Group of the Look AHEAD Research Group, et al. A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med. 2009;169:1916–26.
Hollander PA, Elbein SC, Hirsch IB, et al. Role of orlistat in the treatment of obese patients with type 2 diabetes. A 1-year randomized double-blind study. Diabetes Care. 1998;21:1288–94.
Kelley DE, Bray GA, Pi-Sunyer FX, et al. Clinical efficacy of orlistat therapy in overweight and obese patients with insulin-treated type 2 diabetes: a 1-year randomized controlled trial. Diabetes Care. 2002;25:1033–41.
Garvey WT, Ryan DH, Bohannon NJ, et al. Weight-loss therapy in type 2 diabetes: effects of phentermine and topiramate extended-release. Diabetes Care. 2014;37:3309–16.
Gadde KM, Allison DB, Ryan DH, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341–52.
O’Neil PM, Smith SR, Weissman NJ, et al. Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. Obesity. 2012;20:1426–36.
Hollander P, Gupta AK, Plodkowski R, COR-Diabetes Study Group, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36:4022–9.
Sjöström L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. J Amer Med Assoc. 2014;311:2297–304.
Schauer PR, Bhatt DL, Kirwan JP, STAMPEDE Investigators, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–13. This study reports 3-year outcomes of the STAMPEDE trial comparing bariatric surgery with medical therapy alone. It demonstrates improved outcomes in glycemic control, body weight, use of glucose-lowering medications, and quality of life in the surgery group.
O’Brien PE, Macdonald L, Anderson M, et al. Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg. 2013;257:87–94.
Adams TD, Davidson LE, Litwin SE, et al. Gastrointestinal surgery: cardiovascular risk reduction and improved long-term survival in patients with obesity and diabetes. Curr Atheroscler Rep. 2012;14:606–15.
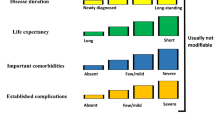
Garvey WT. New tools for weight-loss therapy enable a more robust medical model for obesity treatment: rationale for a complications-centric approach. Endocr Pract. 2013;19:864–74.
Garvey WT, Garber AJ, Mechanick JI, et al, On Behalf Of The AACE Obesity Scientific Committee. American Association of Clinical Endocrinologists and American College of Endocrinology consensus conference on obesity: building an evidence base for comprehensive action. Endocrine Practice. 2014;20:956--76.
Garvey WT, Garber AJ, Mechanick JI, et al, On Behalf Of The AACE Obesity Scientific Committee. American Association of Clinical Endocrinologists and American College of Endocrinology position statement on the 2014 advanced framework for a new diagnosis of obesity as a chronic disease. Endocrine Practice. 2014; 20:977--89.
Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100:342--62.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocrine Practice. 2013;19:337--72.
Heneghan HM, Nissen S, Schauer PR. Gastrointestinal surgery for obesity and diabetes: weight loss and control of hyperglycemia. Curr Atheroscler Rep. 2012;14:579–87.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. J Amer Med Assoc. 2004;292:1724–37.
Mingrone G, Panunzi S, Gaetano AD, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery vs intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–76.
Ikramuddin S, Korner J, Lee W-J, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the diabetes surgery study randomized clinical trial. J Amer Med Assoc. 2013;309:2240–9.
Liang Z, Wu Q, Chen B, et al. Effect of laparoscopic Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus with hypertension: a randomized controlled trial. Diabetes Res Clin Pract. 2013;1:50–6.
Courcoulas AP, Goodpaster BH, Eagleton JK, et al. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA Surg. 2014;149:707–15.
Halperin F, Ding S-A, Simonson DC, et al. Roux-en-Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes: feasibility and 1-year results of a randomized clinical trial. JAMA Surg. 2014;149:716–26.
Gill RS, Birch DW, Shi X, et al. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6:707-13.
Garvey WT, Lara-Castro C. Diet, Insulin Resistance, and Obesity: Zoning in on Data for Atkins Dieters Living in South Beach. J Clin Endocrinol Metab. 2004;89:4197-205.
Weiss R, Taksali SE, Dufour S, et al. The "obese insulin-sensitive" adolescent: importance of adiponectin and lipid partitioning. J Clin Endocrinol Metab. 2005;90:3731-7.
Lara-Castro C, Newcomer BR, Rowell J, et al. Effects of short-term very low calorie diet on intramyocellular lipid and insulin sensitivity in nondiabetic and type 2 diabetic subjects. Metabolism. 2008;57:1–8.
Vitola E, Deivanayagam S, Stein RI, et al. Weight loss reduces liver fat and improves hepatic and skeletal muscle insulin sensitivity in obese adolescents. Obesity. 2009;17:1744–8.
Henry RR, Wallace P, Olefsky JM. Effects of weight loss on mechanisms of hyperglycemia in obese non-insulin-dependent diabetes mellitus. Diabetes. 1986;35:990–8.
Garvey WT, Olefsky JM, Griffin J, et al. The effect of insulin treatment on insulin secretion and insulin action in type II diabetes mellitus. Diabetes. 1985;34:222–34.
Garvey W, Birnbaum M. Insulin resistance and disease. Bailliere’s clinical endocrinology and metabolism, edited by Ferrannini E: Bailliere Tindall:785–873, 1994.
Rossetti L, Giaccari A, DeFronzo RA. Glucose toxicity. Diabetes Care. 1990;13:610–30.
Richter EA, Hansen BF, Hansen SA. Glucose-induced insulin resistance of skeletal-muscle glucose transport and uptake. Biochem J. 1988;252:733–7.
Baron AD, Zhu JS, Zhu JH, et al. Glucosamine induces insulin resistance in vivo by affecting GLUT 4 translocation in skeletal muscle. Implications for glucose toxicity. J Clin Invest. 1995;96:2792–801.
Garvey WT, Olefsky JM, Matthaei S, et al. Glucose and insulin co-regulate the glucose transport system in primary cultured adipocytes. A new mechanism of insulin resistance. J Biol Chem. 1987;262:189–97.
Bailey CJ, Turner SL. Glucosamine-induced insulin resistance in L6 muscle cells. Diabetes Obes Metab. 2004;6:293–8.
Marshall S. Role of insulin, adipocyte hormones, and nutrient-sensing pathways in regulating fuel metabolism and energy homeostasis: a nutritional perspective of diabetes, obesity, and cancer. Sci STKE. 2006;2006:re7.
Scarlett JA, Kolterman OG, Ciaraldi TP, et al. Insulin treatment reverses the postreceptor defect in adipocyte 3-O-methylglucose transport in type II diabetes mellitus. J Clin Endocrinol Metab. 1983;56:1195–201.
Friedman JE, Dohm GL, Leggett-Frazier N, et al. Restoration of insulin responsiveness in skeletal muscle of morbidly obese patients after weight loss. Effect on muscle glucose transport and glucose transporter GLUT4. J Clin Invest. 1992;89:701–5.
Greenfield MS, Doberne L, Rosenthal M, et al. Effect of sulfonylurea treatment on in vivo insulin secretion and action in patients with non-insulin-dependent diabetes mellitus. Diabetes. 1982;31:307–12.
Yki-Jarvinen H, Helve E, Koivisto VA. Hyperglycemia decreases glucose uptake in type I diabetes. Diabetes. 1987;36:892–6.
Bradley D, Magkos F, Klein S. Effects of bariatric surgery on glucose homeostasis and type 2 diabetes. Gastroenterology. 2012;143:897–912.
Isbell JM, Tamboli RA, Hansen EN, et al. The importance of caloric restriction in the early improvements in insulin sensitivity after Roux-en Y gastric bypass surgery. Diabetes Care. 2010;33:1438–42.
Kadera BE, Lum K, Grant J, et al. Remission of type 2 diabetes after Roux-en Y gastric bypass is associated with greater weight loss. Surg Obes Relat Dis. 2009;5:305–9.
Dixon JB. Obesity and diabetes: the impact of bariatric surgery on type-2 diabetes. World J Surg. 2009;33:2014–21.
Hamza N, Abbas MH, Darwish A, et al. Predictors of remission of type 2 diabetes mellitus after laparoscopic gastric banding and bypass. Surg Obes Relat Dis. 2011;7:691–6.
Chikunguwo SM, Wolfe LG, Dodson P, et al. Analysis of factors associated with durable remission of diabetes after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2010;6:254–9.
D’Alessio DA, Prigeon RL, Ensinck JW. Enteral enhancement of glucose disposition by both insulin-dependent and insulin-independent processes. A physiological role of glucagon-like peptide I. Diabetes. 1995;44:1433–7.
Gutzwiller JP, Drewe J, Göke B, et al. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am J Physiol. 1999;276:R1541–4.
Flint A, Raben A, Ersbøll AK, et al. The effect of physiological levels of glucagon-like peptide-1 on appetite, gastric emptying, energy and substrate metabolism in obesity. Int J Obes. 2001;25:781–92.
le Roux CW, Aylwin SJB, Batterham RL, et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243:108–14.
Morínigo R, Moizé V, Musri M, et al. Glucagon-like peptide-1, peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2006;91:1735–40.
Laferrère B, Heshka S, Wang K, et al. Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care. 2007;30:1709–16.
Laferrère B. Diabetes remission after bariatric surgery: is it just the incretins. Int J Obes. 2011;35:S22–5.
Jørgensen NB, Dirksen C, Bøjsen-Moller KN, et al. Exaggerated glucagon-like peptide 1 response is important for improved β-cell function and glucose tolerance after Roux-en-Y gastric bypass in patients with type 2 diabetes. Diabetes. 2013;62:3044–52.
Salehi M, Prigeon RL, D’Alessio DA. Gastric bypass surgery enhances glucagon-like peptide 1-stimulated postprandial insulin secretion in humans. Diabetes. 2011;60:2208–14.
Gill RS, Birch DW, Shi X, et al. Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis. 2010;6:707–13.
Nannipieri M, Baldi S, Mari A, et al. Roux-en-Y gastric bypass and sleeve gastrectomy: mechanisms of diabetes remission and role of gut hormones. J Clin Endocrinol Metab. 2013;98:4391–9.
Korner J, Bessler M, Inabnet W, et al. Exaggerated GLP-1 and blunted GIP secretion are associated with Roux-en-Y gastric bypass but not adjustable gastric banding. Surg Obes Relat Dis. 2007;3:597–301.
Laferrère B, Teixeira J, McGinty J, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008;93:2479–85.
Bojsen-Møller KN, Dirksen C, Jørgensen NB, et al. Early enhancements of hepatic and later of peripheral insulin sensitivity combined with increased postprandial insulin secretion contribute to improved glycemic control after Roux-en-Y gastric bypass. Diabetes. 2014;63:1725–37.
Knop FK, Taylor R. Mechanism of metabolic advantages after bariatric surgery. Diabetes Care. 2013;36:S287–91. This is a recent review of the mechanisms of bariatric surgery focusing on gastrointestinal factors versus food restriction.
Elahi D, Galiatsatos P, Rabiee A, et al. Mechanisms of type 2 diabetes resolution after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2014;10:1028–40.
Lingvay I, Guth E, Islam A, et al. Rapid improvement in diabetes after gastric bypass surgery: is it the diet or surgery? Diabetes Care. 2013;36:2741–7.
Dirksen C, Hansen DL, Madsbad S, et al. Postprandial diabetic glucose tolerance is normalized by gastric bypass feeding as opposed to gastric feeding and is associated with exaggerated GLP-1 secretion. Diabetes Care. 2010;33:375–7.
Hylemon PB, Zhou H, Pandak WM, et al. Bile acids as regulatory molecules. J Lipid Res. 2009;50:1509–20.
Lefebvre P, Cariou B, Lien F, et al. Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev. 2009;89:147–91.
Glicksman C, Pournaras DJ, Wright M, et al. Postprandial plasma bile acid responses in normal weight and obese subjects. Ann Clin Biochem. 2010;47:482–4.
Prawitt J, Caron S, Staels B. Bile acid metabolism and the pathogenesis of type 2 diabetes. Curr Diab Rep. 2011;11:160–6.
Patti M-E, Houten SM, Bianco AC, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity. 2009;17:1671–7.
Nakatani H, Kasama K, Oshiro T, et al. Serum bile acid along with plasma incretins and serum high-molecular weight adiponectin levels are increased after bariatric surgery. Metabolism. 2009;58:1400–7.
Jansen PLM, van Werven J, Aarts E, et al. Alterations of hormonally active fibroblast growth factors after Roux-en-Y gastric bypass surgery. Dig Dis. 2011;29:48–51.
Pournaras DJ, Glicksman C, Vincent RP, et al. The role of bile after Roux-en-Y gastric bypass in promoting weight loss and improving glycaemic control. Endocrinology. 2012;153:3613–9.
Ahmad NN, Pfalzer A, Kaplan LM. Roux-en-Y gastric bypass normalizes the blunted postprandial bile acid excursion associated with obesity. Int J Obes. 2013;37:1553–9.
Gerhard GS, Styer AM, Wood GC, et al. A role for fibroblast growth factor 19 and bile acids in diabetes remission after Roux-en-Y gastric bypass. Diabetes Care. 2013;36:1859–64.
Kohli R, Bradley D, Setchell KD, et al. Weight loss induced by Roux-en-Y gastric bypass but not laparoscopic adjustable gastric banding increases circulating bile acids. J Clin Endocrinol Metab. 2013;98:E708–12.
Lefebvre P, Cariou B, Lien F, et al. Role of bile acids and bile acid receptors in metabolic regulation. Physiol Rev. 2009;89:147–91.
Knop FK. Bile-induced secretion of glucagon-like peptide-1: pathophysiological implications in type 2 diabetes? Am J Physiol Endocrinol Metab. 2010;299:E10–3.
Kohli R, Kirby M, Setchell KDR, et al. Intestinal adaptation after ileal interposition surgery increases bile acid recycling and protects against obesity-related comorbidities. Am J Physiol Gastrointest Liver Physiol. 2010;299:G652–60.
Kohli R, Setchell KDR, Kirby M, et al. A surgical model in male obese rats uncovers protective effects of bile acids post-bariatric surgery. Endocrinology. 2013;154:2341–51.
Ryan KK, Trmaroli V, Clemmensen C, et al. FXR is a molecular target for the effects of vertical sleeve gastrectomy. Nature. 2014;509:183–8. This study reports that sleeve gastrectomy is associated with increased circulating bile acids and may act through FXR to improve glucose tolerance in a rodent model.
Goncalves D, Barataud A, De Vadder F, et al. Bile routing modification reproduces key features of gastric bypass in rat. Ann Surg. 2015. doi:10.1097/SLA.0000000000001121.
Ley RE, Turnbaugh PJ, Klein S, et al. Human gut microbes associated with obesity. Nature. 2006;444:1022–3.
Turnbaugh PJ, Ley RE, Mahowald MA, et al. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–31.
Cani PD, Delzenne NM. Gut microflora as a target for energy and metabolic homeostasis. Curr Opin Clin Nutr Metab Care. 2007;10:729–34.
Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457:480–4.
Diamant M, Blaak EE, de Vos WM. Do nutrient-gut-microbiota interactions play a role in human obesity, insulin resistance and type 2 diabetes? Obes Rev. 2010;12:272–81.
Larsen N, Vogensen FK, van den Berg FWJ, et al. Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. Plos One. 2010;5:e9085.
Asrafian H, Beuter M, Ahmed K, et al. Metabolic surgery: an evolution through bariatric animal models. Obes Rev. 2010;11:907–20.
Furet J-P, Kong L-C, Tap J, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–57.
le Roux CW, Bueter M, Theis N, et al. Gastric bypass reduces fat intake and preference. Am J Physiol Regul Integr Comp Physiol. 2011;301:R1057–66.
Aron-Wisnewsky J, Doré J, Clement K. The importance of the gut microbiota after bariatric surgery. Nat Rev Gastroenterol Hepatol. 2012;9:590–8.
Seto CT, Jeraldo P, Orenstein R, et al. Prolonged use of a proton pump inhibitor reduces microbial diversity: implications for Clostridium difficile susceptibility. Microbiome. 2014;2:42.
Zhang H, DiBaise JK, Zuccolo A, et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci U S A. 2009;106:2365–70.
Graessler J, Qin Y, Zhong H, et al. Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenom J. 2013;13:514–22.
Kong L-C, Tap J, Aron-Wisnewsky J, et al. Gut microbiota after gastric bypass in human obesity: increased richness and associations of bacterial genera with adipose tissue genes. Am J Clin Nutr. 2013;98:16–24.
Everard A, Belzer C, Geurts L, et al. Cross-talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci U S A. 2013;110:9066–71.
Bäckhed F, Ding H, Wang T, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A. 2004;101:15718–23.
Brun Paola, Castagliuolo I, Di Leo V, et al. Increased intestinal permeability in obese mice: new evidence in the pathogenesis of nonalcoholic steatohepatitis. Am J Physiol Gastrointest Liver Physiol. 2006;292:G518–25.
Gill SR, Pop M, DeBoy RT, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312:1355–9.
Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–72.
Creely SJ, McTernan PG, Kusminski CM, et al. Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab. 2007;292:E740–7.
Cani PD, Bibiloni R, Knauf C, et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–81.
Schwiertz A, Taras D, Schäfer K, et al. Microbiota and SCFA in lean and overweight healthy subjects. Obesity. 2010;18:190–5.
Li JV, Ashrafian H, Bueter M, et al. Metabolic surgery profoundly influences gut microbial-host metabolic cross-talk. Gut. 2011;60:1214–23.
Liou AP, Paziuk M, Luevano Jr J-M, et al. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5:1–11. This study uses a mouse model of RYGB and transfers microbiota from mice post-RYGB, sham surgery, or sham surgery with caloric restriction into germ-free mice.
Ridaura VK, Faith JJ, Rey FE, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341:1241214.
Vrieze A, van Nood E, Holleman F, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterolology. 2012;143:913–6. To our knowledge, this is the only study in humans investigating the impact of transfer of intestinal microbiota on insulin sensitivity.
Aron-Wisnewsky J, Tordjman J, Poitou C, et al. Human adipose tissue macrophages: M1 and M2 cell surface markers in subcutaneous and omental depots and after weight loss. J Clin Endocrinol Metab. 2009;94:4619–23.
Clement K. Bariatric surgery, adipose tissue and gut microbiota. Int J Obes. 2011;35:S7–15.
Barres R, Kirchner H, Rasmussen M, et al. Weight loss after gastric bypass surgery in human obesity remodels promoter methylation. Cell Rep. 2013;3:1020–7.
Kirchner H, Nylen C, Laber S, et al. Altered promoter methylation of PDK4, IL1 B, IL6, and TNF after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2014;10:671–8.
Heneghan HM, Miller N, Kerin MJ. Role of microRNAs in obesity and the metabolic syndrome. Obes Rev. 2010;11:354–61.
Bruckmueller H, Oswald S, Häsler R, et al. Influence of Roux-en-Y gastric bypass surgery on the gene expression and microRNA in the small intestine. Proc Br Pharmacol Soc. 2013. http://www.pA2online.org/abstracts/Vol11Issue2abst017P.pdf.
Ortega FJ, Mercader JM, Catalán V. Targeting the circulating microRNA signature of obesity. Endocrinol Metab. 2013;59:781–92.
Arterburn DE, Bogart A, Sherwood NE, et al. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg. 2013;23:93–102.
Wang GF, Yan YX, Xu N, et al. Predictive factors of type 2 diabetes mellitus remission following bariatric surgery: a meta-analysis. Obes Surg. 2015;25:199–208.
Acknowledgments
This work was supported by grants from the National Institutes of Health (DK-038765, DK-083562), by the Merit Review Program of the Department of Veterans Affairs, and by a Career Development Award from the Society for Surgery of the Alimentary Tract. We also acknowledge support from the UAB Diabetes Research Center (P30 DK079626).
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
J. Grams declares that he has no conflict of interest.
W. Timothy Garvey reports personal fees from Novo Nordisk, Boehringer-Ingelheim, Takeda, Vivus, LipoScience, Daiichi-Sankyo, Eisai, Janssen, Alkermes, and Astra Zeneca. He also reports grants from Merck, Vivus, Weight Watchers, Astra Zeneca, Sanofi, Eisai, and Pfizer.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Obesity Treatment
Rights and permissions
About this article
Cite this article
Grams, J., Garvey, W.T. Weight Loss and the Prevention and Treatment of Type 2 Diabetes Using Lifestyle Therapy, Pharmacotherapy, and Bariatric Surgery: Mechanisms of Action. Curr Obes Rep 4, 287–302 (2015). https://doi.org/10.1007/s13679-015-0155-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-015-0155-x