Abstract
COVID-19 was recognized as a pandemic in the United States in March 2020. Since the emergence, research has explored conditions associated with the illness; however, racial disparities remain underexplored. The purpose of this paper is to explore disparities in conditions associated with an increased severity risk of COVID-19 including race, personal factors, healthcare accessibility, and affordability. Using data from the 2018 National Health Interview Survey (NHIS), univariate and multivariate analysis were performed. More Non-Hispanic (NH) Blacks (61.1%) and NH Whites (61.2%) had conditions associated with increased severity risk of COVID-19 compared to Hispanics (47.1%) (p < .001). Racial differences revealed a higher proportion of NH Blacks with increased severity risk of COVID-19 were female (p < .001), not married (p < .001), not employed for wages (p < .001), had accessibility issues with transportation (p < .001), and had affordability issues with paying for medicine (p < .001). A higher proportion of Hispanic persons had a health place change (p = .020), had accessibility issues (e.g. telephone (p < .001), longer wait times (p < .001), closed facility (p = .038)) and had affordability issue with worrying about pay (p < .001). Significant predictors that were positively associated with increased severity risk of COVID-19 for all racial/ethnic groups were being NH Black, older age, having appointment issues, and affordability issues with medicine. Differences in magnitude across racial group dynamics were observed. Racial disparities exist in conditions associated with increased severity risk of COVID-19. As future policies and interventions are developed, it is important to consider differentials across racial group dynamics.
Similar content being viewed by others
Introduction
COVID-19 was recognized as a pandemic in the United States in March 2020. Since the emergence, research has explored conditions associated with the illness such as pulmonary conditions, cancer, diabetes, obesity, and older age (CDC 2020; Garg et al. 2020; Jordan et al. 2020; Guan, et al. 2020; Yancy 2020). More recently, race and ethnicity have been identified as risk factors of COVID-19 illustrating that disparities exist (Yancy 2020; Hooper, et al. 2020). Particularly, Blacks and Hispanic persons have been disproportionately impacted by COVID-19 (Hooper et al. 2020).
Although trends are dynamic and constantly evolving, recent data has supported higher rates of age-adjusted hospitalizations and death rates from COVID-19 in minority populations (CDC 2020). In December 2020, it was reported that the hospitalization from COVID-19 for Blacks was 3.7 times the rate compared to Whites. Price-Haywood et al. (2020), in an article exploring hospitalization and mortality among Black and White COVID-19 patients in a large cohort study, found that 70.4% of COVID-19 patients were Black compared to 29.6% patients who were White. Black patients who tested as COVID-19 positive also had higher rates of conditions associated with illnesses such as diabetes, hypertension, kidney disease, and obesity. Similar trends have been observed for other racial minority and ethnic groups such as American Indian or Alaska Native persons, Asian, and Hispanic persons. Whereas the hospitalization rate of Asian persons are 1.2 times the rate of Whites, the rate for American Indian or Alaska Native and Hispanic persons are 4 times higher than Whites. Similar ratios are observed for death rates. The death rate from COVID-19 for Asian persons compared to Whites was 1.1 times higher, whereas for American Indian or Alaska Native persons the death rate was 2.6 times higher and for Hispanic persons 2.8 times higher (CDC 2020).
Health differences by racial group dynamics for COVID-19 are multifactorial and have been linked to social determinants of health such as personal factors (e.g. SES, health behaviors), social factors (e.g. neighborhood and physical environment), and systemic structures (e.g. health care system). A guiding social determinant of health (SDOH) conceptual framework that has been used in this health disparities research is “The five domains of social determinants of health (SDOH)” (Singu et al. 2020) which has revised concepts from Marmot and Wilkinson’s (2005) SDOH model.
Singu’s et al. (2020) SDOH model can be categorized into five key components: (1) health & health care; (2) social & community context; (3) neighborhood & built environment; (4) education; and (5) economic stability. The model has many common elements of well-known SDOH conceptual frameworks (Healthy People 2020; KFF 2018; NCHS 2016). The health and health care component addresses access to health care including primary care and health coverage. This tenet impacts an individual’s likelihood of early detection and optimum management of the chronic health conditions that increase the risk of contracting COVID-19 as well as the early detection and treatment of the virus. The health and health care element of the model aligns with the systemic structures from this study as well as personal factors. Education, from the model, refers to educational attainment. Economic stability assesses income a4nd employment status. Both elements of the SDOH model align with person factors from the current study. Social & community context aligns with the universal definition of SDOH and assesses the environment including where a person live, work, learn, and play (Healthy People 2020). Similarly, neighborhood and built environment have similar underpinnings and assess where people reside (e.g. housing and neighborhood). Both tenets align with the social factors assessed in this study (Singu ert al. 2020).
The SDOH framework has been used to guide this study. Personal factors such as income, education, and employment have been linked to an increased risk of exposure to COVID-19 (CDC 2020). Health disparities research literature comparing racial group dynamics have posited that on average, racial and ethnic minorities have lower levels of income (Reeves et al. 2016), lower educational attainment levels (National Center for Education Statistics 2015), and higher rates of unemployment (Rodgers 2008). For social factors, research has emphasized the importance of social distancing to reduce the spread of COVID-19 (Anderson 2020; Courtemanche 2020). However, research has emphasized that this is more difficult for some racial/ethnic minority groups than others. For example, the Centers for Disease Control and Prevention (2020a, b) highlighted that racial and ethnic minorities are more likely to live in densely populated areas; they are more likely to live in multi-family households; and are over-represented in group facilities (e.g. shelters). Similarly, related to systemic structures (e.g. healthcare system), racial and ethnic minorities are more likely to lack health insurance coverage or have barriers when accessing health care (Millett et al. 2020; Williams et al. 2010).
Research regarding COVID-19 is evolving. Although there has been some preliminary research regarding racial disparities and inequities that exist with COVID-19, this area remains underexplored. Laurencin and McClinton (2020) highlighted the need to identify and address unique challenges that may persist for ethnic minority communities as it relates to COVID-19. Using data from the 2018 National Health Interview Survey (NHIS), the purpose of this paper is to explore disparities in conditions associated with an increased severity risk of COVID-19 including race, personal factors, healthcare accessibility, and affordability.
Methods
Setting and Study Design
This study uses 2018 data from the Centers for Disease Control and Prevention (CDC) National Health Interview Survey (NHIS). The 2018 NHIS data is the most recent data released (National Center for Health Statistics 2019b, c). The NHIS is a national cross-sectional survey and dataset that assesses the basic health of the United States population through the collection of information on health conditions (e.g. illnesses and disabilities). Similarly, the NHIS collects demographic, socioeconomic, health behavior, accessibility to healthcare, and affordability of health care data in which measures of each are used in this study. The national dataset has several public data files such as a family, household, person, sample child, and sample adult. Each data file has a different set of core questions pertaining to health conditions of the respective populations in each datafile (e.g. family, household, child, and adult). In this study, the sample adult data file was used. This dataset includes a nationally representative sample of 25,417 responses.
Factors (Demographic Characteristics, Personal Factors, General Health, Access to Healthcare, Healthcare Affordability, and Health Conditions Related to COVID-19)
Demographic Characteristics
The demographic characteristics explored in this study were race, gender, and age. Missing data were excluded from this analysis. Race was defined as non-Hispanic (NH) Whites, NH Blacks, and Hispanic persons. This study restricted analysis to the three racial groups because of the emerging trends of COVID-19 with Blacks and Hispanic persons as well as the small sample sizes of other racial categories within the NHIS. More specifically, COVID-19 has impacted NH Blacks and Hispanic persons at alarming rates compared to other racial groups (Macias Gil et al. 2020; Thebault et al. 2020; Yancy 2020) and sample sizes of other populations were not comparable in size to NH Blacks, Hispanic persons and NH Whites (e.g. representations from each racial category was less than 5% of the total population). In both the original 2018 NHIS data and in our study, gender was dichotomized as either: (1) male or (2) female. Age was a continuous variable. The age range of the adult NHIS file was 18 to 85. The mean age of the population was 51.69 (SD 18.338).
Personal Factors
In this study, personal factors were operationalized as marital status, and employment status. Both marital status and employed for wages were dichotomized in this study. In the original 2018 NHIS data, marital status was defined by: (1) married (spouse in household), (2) married (spouse not in household), (3) married (spouse in household unknown), (4) widowed, (5) divorced, (6) separated, (7) never married, and (8) living with partner. In this study, marital status was coded as either: (1) married (response categories 1–3) or (2) not married (response categories 4–8). Employment status was defined as either employed for wages or not employed for wages.
General Health
General health was defined in this study by health status and a change in health place. In the NHIS study, health status was assessed by the question, “Compared with 12 months ago, would you say your health is better, worse, or about the same?” The possible responses were: (1) better, (2) worse, or (3) about the same. In this study, responses were dichotomized to reflect either: (1) worse or (2) about the same/better. The variable, “a change in health place”, was assessed in the original NHIS dataset and this study by the question, “At any time in the past 12 months, did you change the place(s) to which you usually go for health care?” The possible responses were either: (1) yes or (2) no.
Issues with Healthcare Access
In this study, there were five variables that accessed issues with health access which explored accessibility issues with the following: the telephone, making an appointment, long wait times, facility closed, and transportation to receive healthcare services. Each of the variables were dichotomized with a response format of yes or no.
Issues with Healthcare Affordability
This study assessed issues with healthcare affordability by exploring two variables: (1) cannot afford medicine and (2) worried cannot pay for medical bills. In the NHIS data and this study, the question for issues with affordability for medicine was, “During the past 12 months, was there any time when you needed [prescription medicines], but didn't get it because you couldn't afford it?” The responses were either yes or no. The second question assessing affordability in the NHIS dataset was, “If you get sick or have an accident, how worried are you that you will be able to pay your medical bills? Are you very worried, somewhat worried, or not at all worried?” The original response categories were reflected accordingly (e.g. worried, somewhat worried, or not worried at all). In this study, responses were dichotomized to reflect either: (1) worried or somewhat worried, or (2) not worried at all.
Health Conditions Related to COVID-19
The CDC’s guidelines (CDC 2020) of people who are at higher risk for severe illness was used to identify health conditions associated with an increased severity risk of COVID-19 in the NHIS database. According the CDC’s recommendations (CDC 2020), people with high-risk for severe illness from COVID-19 are: (1) people with asthma, (2) people with heart conditions, (3) people who are immunocompromised, (4) people with diabetes, (5) people with chronic kidney disease, and (6) people with liver disease. Aligned with the recommendations, the variables used in this study to create a “COVID-19 risk” variable were: hypertension, cholesterol, heart disease, asthma, cancer, and diabetes. In the NHIS database, the core questionnaire assessed, “Have you ever been told by a doctor or other health professional that you had [the specific health condition]?” The possible responses were either yes or no. In this study, if an individual indicated that they had one or more of the illnesses, they were considered as a population with “COVID-19 risk”. “COVID-19 risk” was defined as likely factors associated with a more severe outcome of having the illness. The final “COVID-19 risk” variable was dichotomized as either yes or no.
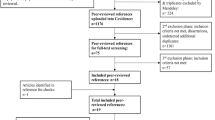
Statistical Analysis
Using data from the 2018 National Health Interview Survey (NHIS), univariate (e.g. descriptive statistics and chi-square analysis) and multivariate analysis were performed. The univariate analysis assessed statistical population differences (e.g. total population and populations with conditions with increased severity risk of COVID-19) and racial differentials (e.g. NH Black, NH White, and Hispanic populations). Multivariate logistic regression models were used to assess the likelihood of having conditions with increased severity risk of COVID-19 based on demographic, personal factors, general health, healthcare access issues, and healthcare affordability issues. Similarly, magnitude differences were explored by calculating Cohen’s f2. Multinominal logit modeling were conducted to determine if the social determinants of health account for the racial differences between NH Black, NH White, and Hispanic persons. All analysis were performed using IBM SPSS v.25.
Results
Univariate analyses were conducted to assess the total population, the population with conditions associated with an increased severity risk of COVID-19, and racial differentials between NH Blacks, NH Whites, and Hispanic persons. The NHIS 2018 dataset contained 25, 417 cases. There were 17,360 NH Whites (68.3%), 2,838 NH Blacks (11.2%) and 3,179 Hispanic persons (12.5%). In the general population, most individuals were female (54.6%), not married (54.7%), and employed for wages (55.5%). As for general health, healthcare accessibility, and healthcare affordability, most individuals indicated that their health status is about the same or better compared to 12 months ago (91.2%), did not change the place where they go to receive health care (79.1%), and they did not have accessibility issues (e.g. telephone, appointment, long wait times, closed facility, transportation) or affordability issues (e.g. cannot afford medicine or worried cannot pay). The mean age was 51.69 (SD = 18.338).
In the population with conditions associated with an increased severity risk of COVID-19, there were 10,624 NH Whites (71.2%), 1,732 NH Blacks (11.6%), and 1,496 Hispanic persons (10.0%). Similar to the general population, most individuals were female (54.4%), not married (54.2%), indicated that their health status was about the same or better (87.9%), did not change the place where they go to receive health care (84.4%), and did not have accessibility or affordability issues. In contrast to the general population, in this population of individuals with increased severity risk of COVID-19, most individuals not employed for wages (55.3%). The mean age (58.59, SD = 16.767) was higher than the general population (p < .001) (Table 1).
Racial Differentials
In the population with conditions associated with an increased severity risk of COVID-19, racial differentials were observed for NH Whites, NH Blacks, and Hispanic persons. There were more NH Blacks (61.1%) and NH Whites (61.2%) with conditions associated with an increased severity risk of COVID-19 compared to Hispanic persons (47.1%) (p < .001). The mean age of NH Whites was 60.06 (SD = 16.322); for Blacks, it was 56.93 (SD = 16.402); and for Hispanic persons, the mean age was 52.66 (SD = 17.855). Regardless of race, most people with conditions associated with an increased severity risk of COVID-19 were females, not married, not employed for wages, indicated that their health status was about the same or better, did not change the place where they go to receive health care, and did not have accessibility or affordability issues. However, statistical racial differences were observed across gender, marital status, employment status, age, health place, accessibility issues, and affordability issues (e.g. cannot afford medicine and worried about paying).
Compared to NH Whites and Hispanic persons with increased severity risk of COVID-19, a higher proportion of NH Blacks were female (p < .001), not married (p < .001), not employed for wages (p < .001), had accessibility issues with transportation (p < .001), and had affordability issues with paying for medicine (p < .001). A higher proportion of Hispanic persons (compared to NH Blacks and NH Whites) had a health place change (p = .020), had accessibility issues with the telephone (p < .001), longer wait times (p < .001), and the facility being closed (p = .038). More Hispanic persons also had affordability issue with worrying about pay (p < .001) compared to NH Whites and NH Blacks (Table 2).
Multivariate analyses were performed to analyze predictors of “COVID-19 risk of severity” based on demographic characteristics, personal factors, general health, healthcare accessibility and healthcare affordability. COVID-19 risk was defined by conditions associated with an increased severity risk of COVID-19 based on the CDC’s guidelines. The statistical model for NH Blacks yielded a Cox & Snell R2 = .229; for NH Whites, the model resulted in a Cox & Snell R2 = .199; and for Hispanic persons, the Cox & Snell value for R2 was .226. Consistent with other studies (Lin et al. 2011), to account for the large number of predictors used in the study (14 predictors), the significance level threshold was reduced from alpha = .05 to alpha = .004.
Significant predictors that were associated with an increased likelihood of severe COVID-19 risk were being NH Black (OR = 1.23, p < .001), older age (OR = 1.06, p < .001), having appointment issues (OR = 1.43, p < .001), and having affordability issues with medicine (OR = 1.84, p < .001). A decreased likelihood was associated with being male (OR = .77, p < .001), being employed (OR = .73, p < .001), and healthcare status better (OR = .51, p < .001). A large effect size was observed for health care status and affordability of medicine.
Exploring racial differentials in the multivariate models indicated that significant predictors that were associated with an increased likelihood of severe COVID-19 risk for NH Blacks were older age (OR = 1.06, p < .001), and having affordability issues with medicine (OR = 1.89, p = 002). A decreased likelihood was associated with being married (OR = .70, p = .001), being employed (OR = .66, p < .001), and healthcare status better (OR = .45, p < .001). A large effect size was observed for healthcare status better and medicine affordability (Table 3).
For Hispanic persons, significant predictors that were associated with an increased likelihood of severe COVID-19 risk were older age (OR = 1.06, p < .001), having appointment issues (OR = 2.17, p < .001), and having affordability issues with medicine (OR = 2.31, p < .001). A decreased likelihood was associated with being male (OR = .74, p = .002), being employed (OR = .71, p < .001), and healthcare status better (OR = .35, p < .001). A large effect size was observed for health care status better, appointment issues, and medicine affordability.
For NH Whites, significant predictors that were associated with an increased likelihood of severe COVID-19 risk were older age (OR = 1.06, p < .001), having appointment issues (OR = 1.32, p = .001), and having affordability issues with medicine (OR = 1.76, p < .001). A decreased likelihood was associated with being male (OR = .73, p < .001), being employed (OR = .73, p < .001), and healthcare status better (OR = .54, p < .001). A large effect size was observed for health care status better and medicine affordability.
Multivariate nested logit modeling was conducted to assess racial differences in severe COVID-19 risk, as we controlled for social determinants of health defined by demographic characteristics, general health characteristics, healthcare accessibility and healthcare affordability. In each model, the changes in the odds ratio (OR) for racial groups (e.g. NH Black and Hispanic persons) observed as we added variables to the model. In the baseline model, Hispanic persons were 44.0% less likely to have conditions with increased severity risk of COVID-19. Demographic characteristics were added to model 2 without controlling for other factors (e.g. general health characteristics, healthcare accessibility, and healthcare affordability). In this model, the odds ratio (OR) for NH Blacks became statistically significant, with 1.17 times more likely to have conditions with increased severity risk of COVID-19. For Hispanic persons, the OR moved closer to 1, narrowing the racial difference to NH Whites. In model 3 (addition of general health characteristics), the OR for NH Blacks increased to 1.24 times more likely to have conditions with increased severity risk of COVID-19. For Models 4 and 5 when healthcare accessibility and affordability were added to the model respectively, the OR for NH Blacks remained approximately 1.2, whereas the OR for Hispanic persons yielded a decreased likelihood (OR = .83 in Model 4 and OR = .82 in Model 5) of having conditions with increased severity risk of COVID-19 (Table 4).
Discussion
In this study, we explored disparities in conditions associated with an increased severity risk of COVID-19 including race, personal factors, healthcare accessibility, and affordability. There were several key findings of this study. Generally, results indicated that racial disparities exist in conditions associated with increased severity risk of COVID-19.
The first key finding of this study was the relationship between race and the percentage of the population with conditions associated with increased severity risk of COVID-19. Past research has indicated that the factors that may increase the risk for severe illness from COVID-19 are asthma, heart conditions, immunocompromised conditions, diabetes, chronic kidney disease, and liver disease (CDC 2020; Shi et al. 2020; Bonow et al. 2020; Grasselli et al. 2020). In this study, NH Blacks and Hispanic persons were largely overrepresented in the percentage of population with conditions associated with increased severity risk of COVID-19. Racial differences indicated that 61.1% of the NH Black population and 47.1% of the Hispanic population had conditions associated with an increased severity risk of COVID-19. The results align with data concerning the prevalence rates of the risk factors. Racial and ethnic minorities have a higher prevalence of most of the risk factors associated with increased severity risk of COVID-19 compared to Whites (Cunningham et al. 2017). Compared to NH Whites, NH Blacks are more impacted by asthma (Akinbami et al. 2012; Nyenhuis et al. 2017). Although collectively, asthma rates are lower for Hispanic persons overall when compared to NH Whites, the rates of some Hispanic subgroups nearly double the rate of NH Whites (American Lung Association 2020). Similarly, racial and ethnic minorities have the highest death rates from heart disease (Van Dyke et al. 2018), have the highest prevalence of diabetes (Cheng et al. 2019), and are the most impacted population for kidney disease (U.S. Renal Data System 2016). In some health conditions, striking racial differences are noted. Cheng’s et al. (2019) study indicated the prevalence of diabetes in NH White was 12.1% and for NH Blacks, the prevalence rate was 20.4%. Trends in kidney disease have highlighted a similar disparity. The National Institute of Diabetes and Digestive and Kidney Diseases (U.S. Renal Data System 2016) noted a four-fold disparity between NH Blacks and NH Whites in kidney failure development. Similarly, NH Blacks and Hispanic persons are more likely to have Chronic Kidney Disease compared to NH Whites (U.S. Renal Data System 2016). The disparities in health conditions that have been noted in recent literature support and possibly explains the findings of this study illustrating an overrepresentation of NH Blacks and Hispanic persons with conditions associated with increased severity risk of COVID-19.
Another key finding of this study indicated that NH Blacks (mean age 57) and Hispanic persons (mean age 53) who had conditions associated with an increased severity risk of COVID-19 were younger than Whites (mean age 60). Results regarding age differences align with research of Elo and Preston (1997) in which findings indicate that death rates for racial minorities are more than two-fold that of NH Whites at younger ages. Similarly, the younger age of conditions associated with an increased severity risk of COVID-19 could be attributed to a racial disparity in health coverage. Berchick et al. (2018) noted that in 2017, 10.6% of NH Blacks and 16.1% of Hispanic persons were uninsured compared to 5.9% of NH Whites. Aligned with the findings, the CDC (2020) posited that 12.1% of NH Blacks and 20.1% of Hispanic persons under the age of 65 do not have health insurance coverage. The lack of insurance coverage in minority populations may explain the age differs across racial groups in conditions associated with an increased severity risk of COVID-19.
Results related to race and gender yielded important findings. NH Black females had the highest percent within population (61.5%) that had conditions associated with an increased severity risk of COVID-19. In data from the Health Statistics 2018 (NCHS 2019a) assessing perceived health status by race, NH White males who indicated poor health were 2.1%; NH White females, 2.3%, NH Black males, 2.8%, and NH Black females, 3.0%. In a similar study exploring health related quality of life and racial differences, Skarupski (2007) found that NH Black females were at increased odds of having poor health related quality of life compared to other racial and gender groups. The findings from literature assessing health outcomes of NH Black females are consistent with the findings in this study. The poorer health outcomes of NH Black females that have been reported in literature may explain the highest population percent of individuals who had conditions associated with an increased severity risk of COVID-19.
Along with the stark differences noted in age and gender racial differences, our findings posited key information regarding accessibility and affordability of health care. Compared to NH Whites, more NH Black and Hispanic persons who had conditions associated with an increased severity risk of COVID-19 had accessibility issues (e.g. telephone, appointments, long wait times, facility closed, transportation) and affordability issues (e.g. could not afford medicine, and worried that they could not pay bills for health care). Goins et al. (2005) noted five key barriers to health care including challenges with transportation, inadequate care, limited supplies, social isolation, and financial issues. In a related study, Syed et al. (2013) discussed the relationship between barriers to healthcare access and health outcomes indicating a direct association: barriers lead to poor management of illnesses which lead to poor health outcomes. In our study, since NH Blacks and Hispanic persons had more barriers to healthcare, which included accessibility and affordability issues, this could possibly explain the higher population percentages of minority racial groups with poorer health outcomes (e.g. conditions associated with an increased severity risk of COVID-19).
To further explore racial differentials in conditions associated with increased severity risk of COVID-19, this study examined key predictors that were associated with an increased or decreased likelihood of the illness. Regardless of racial and ethnicity group, significant predictors were observed with increased likelihood of COVID-19 risk for NH Blacks, NH Whites, and Hispanic persons for the variables older age, and having affordability issues with medicine. The results for age and health status were not surprising. As age increases, so does the increase in comorbidities and thus, an increased severity risk of COVID-19. As for affordability issues with medicine, if individuals are unable to obtain their health necessities and experience barriers to health care access, this may make them more prone to becoming ill (Jeon et al. 2009; Syed et al. 2013) which may explain the increased association of “affordability issues with medicine” to increased severity risk of COVID-19. A decreased likelihood for NH Blacks, NH Whites, and Hispanic persons was observed for the variables being employed and health care status better. Generally, individuals without a lot of illnesses and comorbidities are more likely to be employed (i.e. those with health burdens are less likely to be able to work). Similarly, those who perceive their health as the same or better compared to 12 months ago, may be at a lower risk of the illness.
Of particular interest, results from exploring racial differentials indicated that in the NH Black population, being married was associated with a 30% decreased likelihood of “increased severity risk of COVID-19”. Research has indicated that marriage has some positive benefits (Schone and Weinick 1998; Grundy and Tomassini 2010) such as a positive impact economically (Waite and Gallagher 2002) and a social benefit (Umberson et al. 2010). The economic and social benefit can improve health. Parelli-Harris et al. (2018) findings indicated that individuals who were married in the U.S. had higher perceived health. Both, Johnson et al. (2000) and Schoenborn (2004) have posited that marriage is protective for NH Blacks. This may explain the decrease association of the findings in this study regarding marriage.
In Hispanic populations and NH Whites, an increased association to increased severity risk of COVID-19 was observed for appointment issues, whereas a decreased association was observed for being male. As noted previously, barriers to health care access can lead to poor management of illnesses and poor health outcomes (Syed et al. 2013) which may explain the association to appointment issues. The decreased association observed for being male may be attributed to an underestimate of illnesses diagnosed. In a study exploring the relationship of masculinity and health, Courtenay (2000) found gender differences in preventative health care services indicating that men tend to minimize their needs and have lower levels of provider engagement when seeking care. This may explain the decreased association to increased severity risk of COVID-19.
To examine the strength of the predictors in conditions associated with increased severity risk of COVID-19, effect sizes were explored. Regardless of race/ethnicity, a large effect size was observed for health care status and medicine affordability issues; however, there were differences in magnitude. The differences in magnitude of health status and affordability may be linked to cultural mistrust and health insurance. NH Blacks and Hispanic persons who indicated a worse health status and affordability issues with medicine may not have adequate insurance to cover their medical necessities. Similarly, NH Blacks and Hispanic persons with poorer general health and affordability issues may not go to the doctor. A possible reason that may explain why NH Blacks with poorer general health do not go to the doctor is mistrust of the medical system (Brandon et al. 2005) or perceived perspectives that going to the doctor is more burdensome that beneficial (Blake 1984). Similarly, Hispanic persons health outcomes may be linked to higher levels of being uninsured. If NH Blacks and Hispanic persons feel that their insurance will not adequately cover the expenses of receiving care (or do not have insurance), they are more likely to avoid going. The relationship between not receiving adequate health care services may explain the higher likelihoods of having conditions associated with increased severity risk of COVID-19 for racial/ethnic minorities.
Results from the multinomial models illustrated the effect on racial differences in severe COVID-19 risk, as we controlled for social determinants of health. When demographic characteristics, general health characteristics, healthcare accessibility and healthcare affordability were considered, the racial gap in increased severity risk of COVID-19 became more evident for racial and ethnic minorities. Results show the complexity of the substantive impact that SES, accessibility and affordability can have on health outcomes, particularly for racial and ethnic minorities. More research is needed in this area regarding increased severity risk of COVID-19.
Limitations
There are several limitations to this study. One limitation is the study population. Our research specifically focuses on NH White, NH Black, and Hispanic populations. However, it is acknowledged that COVID-19 has had an impact on all racial group dynamics. Particularly, stark increases in cases have been noted amongst NH American Indian or Alaska Native persons. Future research should explore disparities in other populations as well.
Second, data were used from the NHIS due to limited data availability. Currently, there is limited public data available for COVID-19. Therefore, data for this study was extrapolated from other risk factors and conditions associated with an increased severity risk of COVID-19 based on the CDC’s guidelines. It is also noted that there is a difference in severity risk of COVID-19 and acquiring COVID-19. Although it is acknowledged that some of the factors examined in this research may be more associated with acquiring COVID-19 (e.g. younger age, gender, employment status, access to transportation) and others factors are more associated with severity, we were limited in the exploration of the differences due to structural considerations of the secondary data. Future research should assess the risk of COVID-19 in a population that has been diagnosed with the illness, also the risk of acquiring COVID-19.
Lastly, it is acknowledged that because of the lack of ‘actual’ COVID-19 cases in this study, the data may not be congruent across all measures. Therefore, the data and disparities in this study may be underreported. Future research should assess a COVID-19 population to ensure accuracy in the percentage differentials that exist between racial group dynamics.
Conclusion
COVID-19 was recognized as a pandemic in the United States in March 2020 and since, a plethora of research has emerged concerning the illness; however, information presented has been disproportionate with a lack of information concerning details about racial disparities. The purpose of this paper was to explore disparities in conditions associated with an increased severity risk of COVID-19 including race, personal factors, healthcare accessibility, and affordability. Results indicated that racial disparities exist in conditions associated with increased severity risk of COVID-19. As future policies and interventions are developed regarding COVID-19, it is critical to consider differentials across racial group dynamics.
Data Availability
References
American Lung Association. (2020). Current Asthma Demographics. https://www.lung.org/research/trends-in-lung-disease/asthma-trends-brief/current-demographics
Akinbami, L. J., Moorman, J. E., Bailey, C. et al. (2012). Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS data brief, no 94. Hyattsville, MD: National Center for Health Statistics.
Berchick, E. R., Hood, E., & Barnett, J. C. (2018). Health insurance coverage in the United States: 2017. Current population reports. Washington DC: US Government Printing Office.
Blake, J. H. (1984). Doctor can’t do me no good: Social concomitants of health care attitudes and practices among elderly blacks in isolated rural populations. Black folk medicine, 55–62.
Bonow, R. O., Fonarow, G. C., O’Gara, P. T., & Yancy, C. W. (2020). Association of coronavirus disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiology.
Brandon, D. T., Isaac, L. A., & LaVeist, T. A. (2005). The legacy of Tuskegee and trust in medical care: is Tuskegee responsible for race differences in mistrust of medical care? Journal of the National Medical Association, 97(7), 951.
Center for Disease Control and Prevention. (2020). People who are at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html
Center for Disease Control and Prevention. (2020). Infographic: COVID-19 Cases, Hospitalization, and Death by Race/Ethnicity. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/racial-ethnic-disparities/infographic-cases-hospitalization-death.html
Centers for Disease Control and Prevention. (2020). Health of Hispanic or Latino Population. https://www.cdc.gov/nchs/fastats/hispanic-health.htm
Centers for Disease Control and Prevention. (2020). Health of Black or African American non-Hispanic population.https://www.cdc.gov/nchs/fastats/black-health.htm
Cheng, Y. J., Kanaya, A. M., Araneta, M. R. G., Saydah, S. H., Kahn, H. S., Gregg, E. W., ... & Imperatore, G. (2019). Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA, 322(24), 2389–2398
Courtemanche, C., Garuccio, J., Le, A., Pinkston, J., & Yelowitz, A. (2020). Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate: Study evaluates the impact of social distancing measures on the growth rate of confirmed COVID-19 cases across the United States. Health Affairs, 10–1377.
Courtenay, W. H. (2000). Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Social Science & Medicine, 50(10), 1385–1401.
Cunningham, T. J., Croft, J. B., Liu, Y., Lu, H., Eke, P. I., & Giles, W. H. (2017). Vital signs: racial disparities in age-specific mortality among blacks or African Americans—United States, 1999–2015. MMWR. Morbidity and mortality weekly report, 66(17), 444.
Elo, I. T., & Preston, S. H. (1997). Racial and ethnic differences in mortality at older ages. Racial and ethnic differences in the health of older Americans, 10–42.
Garg, S., Kim, L., & Whitaker, M. (2020). Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020. MMWR. Morbidity and Mortality Weekly Report, 69(15), 4458–4464.
Goins, R. T., Williams, K. A., Carter, M. W., Spencer, S. M., & Solovieva, T. (2005). Perceived barriers to health care access among rural older adults: a qualitative study. The Journal of Rural Health, 21(3), 206–213.
Grasselli, G., Zangrillo, A., Zanella, A., Antonelli, M., Cabrini, L., Castelli, A., ... & Iotti, G.(2020). Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. Jama, 323(16), 1574–581.
Grundy, E., & Tomassini, C. (2010). Marital history, health and mortality among older men and women in England and Wales. BMC Public Health, 10(554). Retrieved from http://www.biomedcentral.com/bmcpublichealth/about.
Guan, W. J., Liang, W. H., Zhao, Y., Liang, H. R., Chen, Z. S., Li, Y. M., ... & Ou, C. Q. (2020). Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. European Respiratory Journal, 55(5).
Healthy People. (2020). Social Determinants of Health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
Hooper, M., Nápoles, A. M., & Pérez-Stable, E. J. (2020). COVID-19 and racial/ethnic disparities. JAMA. https://doi.org/10.1001/jama.2020.8598.
Jeon, Y. H., Essue, B., Jan, S., Wells, R., & Whitworth, J. A. (2009). Economic hardship associated with managing chronic illness: A qualitative inquiry. BMC Health Services Research, 9(1), 182.
Johnson, N. J., Backlund, E., Sorlie, P. D., & Loveless, C. A. (2000). Marital status and mortality: The National Longitudinal Mortality Study. Annals of Epidemiology, 10, 224–238.
Jordan, R., Adab, P., & Cheng, K. (2020). Covid-19: Risk factors for severe disease and death. BMJ, 368, 1198.
Kaiser Family Foundation. (2018). Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity. https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/.
Laurencin, C. T., & McClinton, A. (2020). The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. Journal of racial and ethnic health disparities, 1–5.
Lin, M., Lucas, H. C., Shmueli, G. (2011). Too big to fail: larger samples and false discoveries. Robert H. Smith School Research Paper No. RHS 06–068, Available at SSRN: https://ssrn.com/abstract=1336700 or https://doi.org/10.2139/ssrn.1336700.
Macias Gil, R., Marcelin, J. R., Zuniga-Blanco, B., Marquez, C., Mathew, T., & Piggott, D. A. (2020). COVID-19 pandemic: Disparate health impact on the Hispanic/Latinx population in the United States. The Journal of Infectious Diseases, 222(10), 1592–1595.
Millett, G. A., Jones, A. T., Benkeser, D., Baral, S., Mercer, L., Beyrer, C., ... & Sherwood, J. (2020). Assessing differential impacts of COVID-19 on Black communities. Annals of Epidemiology.
National Center for Education Statistics. (2015). The condition of education 2015 (NCES 2015-144). https://nces.ed.gov/pubs2015/2015144.pdf
National Center for Health Statistics. (2019a). National Health Interview Survey, 2018. Public-use data file and documentation. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm.
National Center for Health Statistics. (2019b). Survey Description, National Health Interview Survey, 2018. Hyattsville, Maryland.
National Center for Health Statistics. (2019c). Health, United States, 2018. Hyattsville, Maryland
National Center for Health Statistics. (2016). Chapter 39: Social Determinants of Health. Healthy People 2020 Midcourse Review. Hyattsville, MD.
Nye nhuis, S. M., Krishnan, J. A., Berry, A., Calhoun, W. J., Chinchilli, V. M., Engle, L., ... & Kraft, M. (2017). Race is associated with differences in airway inflammation in patients with asthma. Journal of Allergy and Clinical Immunology, 140(1), 257–265
Perelli-Harris, B., Hoherz, S., Addo, F., Lappegård, T., Evans, A., Sassler, S., & Styrc, M. (2018). Do marriage and cohabitation provide benefits to Health in mid-life? The role of childhood selection mechanisms and partnership characteristics across countries. Population Research and Policy Review, 37(5), 703–728.
Price-Haywood, E. G., Burton, J., Fort, D., & Seoane, L. (2020). Hospitalization and mortality among black patients and white patients with Covid-19. The New England Journal of Medicine, 382(26), 2534–2543. https://doi.org/10.1056/NEJMsa2011686.
Reeves, R., Rodrigue, E., & Kneebone, E. (2016). Five evils: Multidimensional poverty and race in America. https://www.brookings.edu/wp-content/uploads/2016/06/ReevesKneeboneRodrigue_MultidimensionalPoverty_FullPaper.pdf.
Rodgers, W. M. (2008). Understanding the Black and White earnings gap: Why do African Americans continue to earn less despite dramatic gains in education? http://www.prospect.org/cs/articles?article=understanding_the_black_white_earnings_gap
Schoenborn, C. (2004). Marital status and health: United States, 1999–2002. U.S. National Center for Health Statistics. Advance Data from Vital and Health Statistics, 1–32.
Schone, B. S., & Weinick, R. M. (1998). Health-related behaviors and the benefits of marriage for elderly persons. The Gerontologist, 38(5), 618–627.
Skarupski, K. A., De Leon, C. F. M., Bienias, J. L., Scherr, P. A., Zack, M. M., Moriarty, D. G., & Evans, D. A. (2007). Black–white differences in health-related quality of life among older adults. Quality of Life Research, 16(2), 287–296.
Shi, S., Qin, M., Shen, B., Cai, Y., Liu, T., Yang, F., ... & Huang, H. (2020). Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiology
Singu, S., Acharya, A., Challagundla, K., & Byrareddy, S. N. (2020). Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Frontiers in Public Health, 8, 406. https://doi.org/10.3389/fpubh.2020.00406.
Syed, S. T., Gerber, B. S., & Sharp, L. K. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993.
Thebault R, Ba Tran A, Williams V. (2020). The coronavirus is infecting and killing black Americans at an alarmingly high rate. Washington Post. Retrieved from https://www.washingtonpost.com/nation/2020/04/07/coronavirus-is-infecting-killing-black-americans-an-alarmingly-high-rate-post-analysis-shows/.
Umberson, D., Crosnoe, R., & Reczek, C. (2010). Social relationships and health behavior across the life course. Annual Review of Sociology, 36(1), 139–157. https://doi.org/10.1146/annurev-soc-070308-120011.
U.S. Renal Data System. (2016). USRDS 2016 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD.
Van Dyke, M., Greer, S., Odom, E., Schieb, L., Vaughan, A., Kramer, M., & Casper, M. (2018). Heart disease death rates among blacks and whites aged≥ 35 years—United States, 1968–2015. MMWR Surveillance Summaries, 67(5), 1.
Waite, L., & Gallagher, M. (2002). The case for marriage: Why married people are happier. Crown/Archetype: Healthier and Better Off Financially.
Williams, D. R., Mohammed, S. A., Leavell, J., & Collins, C. (2010). Race, socioeconomic status and health: Complexities, ongoing challenges and research opportunities. Annals of the New York Academy of Sciences, 1186, 69–101. https://doi.org/10.1111/j.1749-6632.2009.05339.x.
Yancy, C. W. (2020). COVID-19 and African Americans. JAMA.
Funding
The authors received no financial support for this article.
Author information
Authors and Affiliations
Contributions
Each author participated sufficiently and contributed to the content of this article.
Corresponding author
Ethics declarations
Conflict of interest
There were no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clay, S.L., Woodson, M., Mazurek, K. et al. Racial Disparities and COVID-19: Exploring the Relationship Between Race/Ethnicity, Personal Factors, Health Access/Affordability, and Conditions Associated with an Increased Severity of COVID-19. Race Soc Probl 13, 279–291 (2021). https://doi.org/10.1007/s12552-021-09320-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12552-021-09320-9



