Abstract
Background
Reducing sodium intake can prevent cardiovascular complications and further decline of kidney function in patients with chronic kidney disease. However, the vast majority of patients fail to reach an adequate sodium intake, and little is known about why they do not succeed.
Purpose
This study aims to identify perceived barriers and support strategies for reducing sodium intake among both patients with chronic kidney disease and health-care professionals.
Method
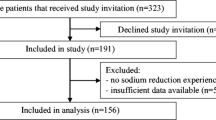
A purposive sample of 25 patients and 23 health-care professionals from 4 Dutch medical centers attended 8 focus groups. Transcripts were analyzed thematically and afterwards organized according to the phases of behavior change of self-regulation theory.
Results
Multiple themes emerged across different phases of behavior change, including the patients’ lack of practical knowledge and intrinsic motivation, the maladaptive illness perceptions and refusal skills, the lack of social support and feedback regarding disease progression and sodium intake, and the availability of low-sodium foods.
Conclusions
The results indicate the need for the implementation of support strategies that target specific needs of patients across the whole process of changing and maintaining a low-sodium diet. Special attention should be paid to supporting patients to set sodium-related goals, strengthening intrinsic motivation, providing comprehensive and practical information (e.g., about hidden salt in products), increasing social support, stimulating the self-monitoring of sodium intake and disease progression, and building a supportive patient–professional relationship that encompasses shared decision making and coaching. Moreover, global programs should be implemented to reduce sodium levels in processed foods, introduce sodium-related product labels, and increase consumer awareness.
Similar content being viewed by others
References
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. J Am Med Assoc. 2007;298(17):2038–47.
Bosma RJ, Krikken JA, van der Heide JJ H, de Jong PE, Navis GJ. Obesity and renal hemodynamics. Contrib Nephrol. 2006;151:184–202.
Baumeister SE, Böger CA, Krämer BK, Döring A, Eheberg D, Fischer B, et al. Effect of chronic kidney disease and comorbid conditions on health care costs: a 10-year observational study in a general population. Am J Nephrol. 2010;31(3):222–9.
De Zeeuw D, Hillege HL, de Jong PE. The kidney, a cardiovascular risk marker, and a new target for therapy. Kidney Int Suppl. 2005;98:S25–9.
Lambers Heerspink HJ, Holtkamp FA, Parving HH, Navis GJ, Lewis JB, Ritz E, et al. Moderation of dietary sodium potentiates the renal and cardiovascular protective effects of angiotensin receptor blockers. Kidney Int. 2012;82(3):330–7.
De Nicola L, Minutolo R, Chiodini P, Zoccali C, Castellino P, Donadio C, et al. Global approach to cardiovascular risk in chronic kidney disease: reality and opportunities for intervention. Kidney Int. 2006;69(3):538–45.
Suzuki H, Takenaka T, Kanno Y, Ohno Y, Saruta T. Sodium and kidney disease. Contrib Nephrol. 2007;155:90–101.
Vogt L, Waanders F, Boomsma F, de Zeeuw D, Navis G. Effects of dietary sodium and hydrochlorothiazide on the antiproteinuric efficacy of losartan. J Am Soc Nephrol. 2008;19(5):999–1007.
Zoja C, Morigi M, Figliuzzi M, Bruzzi I, Oldroyd S, Benigni A, et al. Proximal tubular cell synthesis and secretion of endothelin-1 on challenge with albumin and other proteins. Am J Kidney Dis. 1995;26(6):934–41.
Cianciaruso B, Bellizzi V, Minutolo R, Tavera A, Capuano A, Conte G, et al. Salt intake and renal outcome in patients with progressive renal disease. Miner Electrolyte Metab. 1998;24(4):296–301.
Vegter S, Perna A, Postma MJ, Navis G, Remuzzi G, Ruggenenti P. Sodium intake, ACE inhibition, and progression to ESRD. J Am Soc Nephrol. 2012;23(1):165–73.
Martin LR, Williams SL, Haskard KB, Dimatteo MR. The challenge of patient adherence. Ther Clin Risk Manag. 2005;1(3):189–99.
Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38(3):791–813.
Krikken JA, Laverman GD, Navis G. Benefits of dietary sodium restriction in the management of chronic kidney disease. Curr Opin Nephrol Hypertens. 2009;18(6):531–8.
Van Zuilen AD, Wetzels JF, Bots ML, Van Blankestijn PJ. MASTERPLAN: study of the role of nurse practitioners in a multifactorial intervention to reduce cardiovascular risk in chronic kidney disease patients. J Nephrol Nurs. 2008;21(3):261–7.
Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3 (1):1–150.
Kaptein AA, van Dijk S, Broadbent E, Falzon L, Thong M, Dekker FW. Behavioural research in patients with end-stage renal disease: a review and research agenda. Patient Educ Couns. 2010;81(1):23–9.
Welch JL, Bennett SJ, Delp RL, Agarwal R. Benefits of and barriers to dietary sodium adherence. West J Nurs Res. 2006;28(2):162–80. discussion 181–9.
De Brito-Ashurst I, Perry L, Sanders TAB, Thomas JE, Yaqoob MM, Dobbie H. Barriers and facilitators of dietary sodium restriction amongst Bangladeshi chronic kidney disease patients. J Hum Nutr Diet. 2011;24(1):86–95.
Leventhal H, Meyer D, Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to medical psychology. New York: Pergamon Press; 1980. p. 7–30.
Leventhal H, Brissette IL. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal HE, editors. The self-regulation of health and illness behaviour. London: Routledge; 2003. p. 42–65.
Maes S, Karoly P. Self-regulation assessment and intervention in physical health and illness: a review. Appl Psychol. 2005;54(2):267–99.
Morse JM. The significance of saturation. Qual Health Res. 1995;5(2):147–9.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;2:CD000011.
Curtin RB, Mapes D, Schatell D, Burrows-Hudson S. Self-management in patients with end stage renal disease: exploring domains and dimensions. Nephrol Nurs J. 2005;32(4):389–95.
Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. J Am Med Assoc. 2002;288(19):2469–75.
Chen SH, Tsai YF, Sun CY, Wu IW, Lee CC, Wu MS. The impact of self-management support on the progression of chronic kidney disease: a prospective randomized controlled trial. Nephrol Dial Transplant. 2011;26(11):3560–6.
Wright Nunes JA, Wallston KA, Eden SK, Shintani AK, Ikizler TA, Cavanaugh KL. Associations among perceived and objective disease knowledge and satisfaction with physician communication in patients with chronic kidney disease. Kidney Int. 2011;80(12):1344–51.
Safeer RS, Keenan J. Health literacy: the gap between physicians and patients. Am Fam Physician. 2005;72(3):463–8.
Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–34.
Broadbent E, Petrie KJ, Main J, Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–7.
Chilcot J, Wellsted D, Farrington K. Illness representations are associated with fluid nonadherence among hemodialysis patients. J Psychosom Res. 2010;68(2):203–12.
O’Connor SM, Jardine AG, Millar K. The prediction of self-care behaviors in end-stage renal disease patients using Leventhal’s self-regulatory model. J Psychosom Res. 2008;65(2):191–200.
Clark S, Farrington K, Chilcot J. Nonadherence in dialysis patients: prevalence, measurement, outcome, and psychological determinants. Semin Dial. 2014;27(1):42–9.
Van Dijk S, Scharloo M, Kaptein AA, Thong MSY, Boeschoten EW, Grootendorst DC, et al. Patients’ representations of their end-stage renal disease: relation with mortality. Nephrol Dial Transplant. 2009;24(10):3183–5.
Parfeni M, Nistor I, Covic A. A systematic review regarding the association of illness perception and survival among end-stage renal disease patients. Nephrol Dial Transplant. 2013;28(10):2407–14.
Rifkin DE, Laws MB, Rao M, Balakrishnan VS, Sarnak MJ, Wilson IB. Medication adherence behavior and priorities among older adults with CKD: a semistructured interview study. Am J Kidney Dis. 2010;56(3):439–46.
Elliott WJ. Improving outcomes in hypertensive patients: focus on adherence and persistence with antihypertensive therapy. J Clin Hypertens. 2009;11(7):376–82.
Rollnick S, Miller WR, Butler CC. Motivational interviewing in health care. Helping patients change behavior. New York: Guilford press; 2008.
Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111.
VanBuskirk KA, Wetherell JL. Motivational interviewing with primary care populations: a systematic review and meta-analysis. J Behav Med. 2014;37(4):768–80.
Murray MA, Brunier G, Chung JO, Craig LA, Mills C, Thomas A, et al. A systematic review of factors influencing decision-making in adults living with chronic kidney disease. Patient Educ Couns. 2009;76(2):149–58.
Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. J Hypertens. 2011;29(6):1043–50.
Kim MK, Lopetcharat K, Gerard PD, Drake MA. Consumer awareness of salt and sodium reduction and sodium labeling. J Food Sci. 2012;77(9):S307–13.
Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52(1):1–9.
Jaana M, Paré G. Home telemonitoring of patients with diabetes: a systematic assessment of observed effects. J Eval Clin Pract. 2007;13(2):242–53.
Imai Y, Hosaka M, Elnagar N, Satoh M. Clinical significance of home blood pressure measurements for the prevention and management of high blood pressure. Clin Exp Pharmacol Physiol. 2014;41(1):37–45.
Newson RS, Elmadfa I, Biro G, Cheng Y, Prakash V, Rust P, et al. Barriers for progress in salt reduction in the general population. An international study. Appetite. 2013;71:22–31.
DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23(2):207–18.
Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Heal Educ Behav. 2003;30(2):170–95.
Lindner H, Menzies D, Kelly J, Taylor S, Shearer M. Coaching for behaviour change in chronic disease: a review of the literature and the implications for coaching as a self-management intervention. Aust J Prim Health. 2003;9(3):177–85.
Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10:383–93.
Dötsch M, Busch J, Batenburg M, Liem G, Tareilus E, Mueller R, et al. Strategies to reduce sodium consumption: a food industry perspective. Crit Rev Food Sci Nutr. 2009;49(10):841–51.
Acknowledgments
We would like to thank the participating patients and health-care professionals for their time and contribution. Y.M., L.t.B, and S.v.D. were responsible for the data collection. All authors participated in the design and the revision of the manuscript and gave final approval.
The present study was supported by a grant from The Netherlands Organisation for Health Research and Development-Medical Sciences (ZonMw 300020016) and the Dutch Kidney Foundation (SB93). They had no role in the study design (collecting, analysis or interpretation of data), writing of the paper, and the decision to submit this paper.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study. We confirm all personal identifiers have been removed or disguised so the persons described are not identifiable and cannot be identified through the details of the story.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meuleman, Y., ten Brinke, L., Kwakernaak, A.J. et al. Perceived Barriers and Support Strategies for Reducing Sodium Intake in Patients with Chronic Kidney Disease: a Qualitative Study. Int.J. Behav. Med. 22, 530–539 (2015). https://doi.org/10.1007/s12529-014-9447-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-014-9447-x