Abstract
Purpose of Review
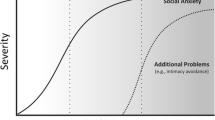
In current review, we evaluate the current literature examining the role of disgust in eating disorders (EDs), and provide a theoretical model designed to inform the study and treatment of disgust-based symptoms in EDs.
Recent Findings
Findings from this review suggest that aberrant disgust-conditioning processes represent promising but understudied mechanisms that may contribute to the risk and maintenance of core eating disorder (ED) psychopathology. In addition, preliminary evidence supports the use of interventions designed to target aversive disgust cues and disrupt maladaptive disgust-based conditioning that may maintain eating pathology. However, experimental studies designed to elucidate the role of disgust and aversive learning processes remain limited.
Summary
Disgust is a promising risk and maintenance factor in EDs. Future systematic investigation is needed to examine disgust-based processes at a mechanistic level in order to better understand the links between disgust, avoidance behaviors, and EDs. Further investigation of the mechanistic role of disgust in EDs is warranted.

Similar content being viewed by others
Data Availability
Not applicable.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. 2011;68(7):724–31.
Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2006;19(4):438–43.
Winkler LA, Christiansen E, Lichtenstein MB, Hansen NB, Bilenberg N, Støving RK. Quality of life in eating disorders: a meta-analysis. Psychiatry Res. 2014;219(1):1–9.
Culbert KM, Racine SE, Klump KL. Research review: what we have learned about the causes of eating disorders–a synthesis of sociocultural, psychological, and biological research. J Child Psychol Psychiatry. 2015;56(11):1141–64.
Hay P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int J Eat Disord. 2013;46(5):462–9.
Butler RM, Heimberg RG. Exposure therapy for eating disorders: a systematic review. Clin Psychol Rev. 2020. https://doi.org/10.1016/j.cpr.2020.101851.
Cardi V, Leppanen J, Mataix-Cols D, Campbell IC, Treasure J. A case series to investigate food-related fear learning and extinction using in vivo food exposure in anorexia nervosa: a clinical application of the inhibitory learning framework. Eur Eat Disord Rev. 2019;27(2):173–81.
Guarda AS, Schreyer CC, Boersma GJ, Tamashiro KL, Moran TH. Anorexia nervosa as a motivated behavior: relevance of anxiety, stress, fear and learning. Physiol Behav. 2015;152:466–72.
Murray SB, Strober M, Craske MG, Griffiths S, Levinson CA, Strigo IA. Fear as a translational mechanism in the psychopathology of anorexia nervosa. Neurosci Biobehav Rev. 2018;95:383–95.
Strober M. Pathologic fear conditioning and anorexia nervosa: on the search for novel paradigms. Int J Eat Disord. 2004;35(4):504–8.
Swinbourne JM, Touyz SW. The co-morbidity of eating disorders and anxiety disorders: a review. Eur Eat Disord Rev. 2007;15(4):253–74.
Swinbourne J, Hunt C, Abbott M, Russell J, St Clare T, Touyz S. The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatry. 2012;46(2):118–31.
Duits P, Cath DC, Lissek S, Hox JJ, Hamm AO, Engelhard IM, et al. Updated meta-analysis of classical fear conditioning in the anxiety disorders. Depress Anxiety. 2015;32(4):239–53.
Knowles KA, Jessup SC, Olatunji BO. Disgust in anxiety and obsessive-compulsive disorders: recent findings and future directions. Curr Psychiatry Rep. 2018;20(9):68.
Pittig A, Treanor M, LeBeau RT, Craske MG. The role of associative fear and avoidance learning in anxiety disorders: gaps and directions for future research. Neurosci Biobehav Rev. 2018;88:117–40.
Pallister E, Waller G. Anxiety in the eating disorders: understanding the overlap. Clin Psychol Rev. 2008;28(3):366–86.
Brown M, Robinson L, Campione GC, Wuensch K, Hildebrandt T, Micali N. Intolerance of uncertainty in eating disorders: a systematic review and meta-analysis. Eur Eat Disord Rev. 2017;25(5):329–43.
Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol Bull. 2007;133(1):1–24.
Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, Asmundson GJ. Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J Anxiety Disord. 2012;26(3):468–79.
Smith KE, Mason TB, Lavender JM. Rumination and eating disorder psychopathology: a meta-analysis. Clin Psychol Rev. 2018;61:9–23.
Olatunji BO, Forsyth JP, Cherian A. Evaluative differential conditioning of disgust: a sticky form of relational learning that is resistant to extinction. J Anxiety Disord. 2007;21(6):820–34. https://doi.org/10.1016/j.janxdis.2006.11.004.
Engelhard IM, Leer A, Lange E, Olatunji BO. Shaking that icky feeling: effects of extinction and counterconditioning on disgust-related evaluative learning. Behav Ther. 2014;45(5):708–19. https://doi.org/10.1016/j.beth.2014.04.003.
Harris AA, Romer AL, Hanna EK, et al. The central role of disgust in disorders of food avoidance. Int J Eat Disord. 2019;52(5):543–53. https://doi.org/10.1002/eat.23047This exploratory, cross-sectional study examined the associations between disgust, anxiety, sensory sensitivity, and picky eating in a large sample of adults (N = 1644); evidence indicates that disgust is more strongly related to severity of ARFID and maladaptive picky eating than anxiety, and that disgust may drive the link between anxiety and food aversion.
Hildebrandt T, Grotzinger A, Reddan M, Greif R, Levy I, Goodman W, et al. Testing the disgust conditioning theory of food-avoidance in adolescents with recent onset anorexia nervosa. Behav Res Ther. 2015;71:131–8.
Olatunji BO. Linking Pavlovian disgust conditioning and eating disorder symptoms: an analogue study. Behav Ther. 2020;51(1):178–89 Findings from this clinical analogue study indicate that individuals with elevated eating disorder symptom severity demonstrate enhanced food disgust during a food-disgust conditioning paradigm, and that rate of disgust acquisition was negatively associated with caloric consumption over the 24-h period following disgust conditioning, as compared to individuals with low eating disorder symptoms.
Bell K, Coulthard H, Wildbur D. Self-disgust within eating disordered groups: associations with anxiety, disgust sensitivity and sensory processing. Eur Eat Disord Rev. 2017;25(5):373–80 This cross-sectional online survey study assessed self-reported anxiety, disgust sensitivity, disgust propensity, self-disgust, and sensory processing variables among women with eating disorder diagnoses (n = 270 AN, 104 BN) or no eating disorder diagnosis (n = 217); findings suggest that self-disgust is elevated in individuals with eating disorders and is positively associated with altered sensory traits (e.g., sensory sensitivity, sensory avoidance, low responsiveness to sensory cues).
Kaye WH, Fudge JL, Paulus M. New insights into symptoms and neurocircuit function of anorexia nervosa. Nat Rev Neurosci. 2009;10(8):573–84.
Steinglass JE, Sysko R, Glasofer D, Albano AM, Simpson HB, Walsh BT. Rationale for the application of exposure and response prevention to the treatment of anorexia nervosa. Int J Eat Disord. 2011;44(2):134–41.
Hildebrandt T, Bacow T, Markella M, Loeb KL. Anxiety in anorexia nervosa and its management using family-based treatment. Eur Eat Disord Rev. 2012;20(1):e1–e16.
Menzel JE, Reilly EE, Luo TJ, Kaye WH. Conceptualizing the role of disgust in avoidant/restrictive food intake disorder: implications for the etiology and treatment of selective eating. Int J Eat Disord. 2019;52(4):462–5 This manuscript reviews current findings supporting the role of disgust as a central factor for pathological selective eating patterns characteristic of avoidant/restrictive feeding and eating disorder (ARFID), and introduces future clinical and research directions that may inform our understanding of selective eating and food avoidance in ARFID.
Cisler JM, Olatunji BO, Lohr JM. Disgust, fear, and the anxiety disorders: a critical review. Clin Psychol Rev. 2009;29(1):34–46.
Mason EC, Richardson R. Looking beyond fear: the extinction of other emotions implicated in anxiety disorders. J Anxiety Disord. 2010;24(1):63–70.
Olatunji BO, Smits JA, Connolly K, Willems J, Lohr JM. Examination of the decline in fear and disgust during exposure to threat-relevant stimuli in blood-injection-injury phobia. J Anxiety Disord. 2007;21(3):445–55.
Olatunji BO, Wolitzky-Taylor KB, Willems J, Lohr JM, Armstrong T. Differential habituation of fear and disgust during repeated exposure to threat-relevant stimuli in contamination-based OCD: an analogue study. J Anxiety Disord. 2009;23(1):118–23.
Smits JA, Telch MJ, Randall PK. An examination of the decline in fear and disgust during exposure-based treatment. Behav Res Ther. 2002;40(11):1243–53.
Wierenga CE, Bischoff-Grethe A, Berner LA, Simmons AN, Bailer U, Paulus MP, et al. Increased anticipatory brain response to pleasant touch in women remitted from bulimia nervosa. Transl Psychiatry. 2020;10(1):236.
Khalsa SS, Hassanpour MS, Strober M, Craske MG, Arevian AC, Feusner JD. Interoceptive anxiety and body representation in anorexia nervosa. Front Psychiatry. 2018;9:444.
Boswell JF, Anderson LM, Oswald JM, Reilly EE, Gorrell S, Anderson DA. A preliminary naturalistic clinical case series study of the feasibility and impact of interoceptive exposure for eating disorders. Behav Res Ther. 2019;117:54–64.
Plasencia M, Sysko R, Fink K, Hildebrandt T. Applying the disgust conditioning model of food avoidance: a case study of acceptance-based interoceptive exposure. Int J Eat Disord. 2019;52(4):473–7 This paper presents findings from a single case study supporting the initial efficacy of adjunctive interoceptive exposure, a treatment that targets interoceptive aversive disgust cues, in an adolescent with anorexia nervosa.
Brown M, Hildebrandt T. Parent-facilitated behavioral treatment for avoidant/restrictive food intake disorder: a case report. Cogn Behav Pract. 2020;27:231–51 This paper presents findings from a single case report examining a novel behavioral intervention that utilizes a counter-conditioning approach to target anxiety- and disgust-based food avoidance behaviors in youth with avoidant/restrictive food intake disorder.
Stasik-O’Brien SM, Schmidt J. The role of disgust in body image disturbance: incremental predictive power of self-disgust. Body Image. 2018;27:128–37 Findings from this study suggest that self-disgust may be a particularly important predictor of body image disturbances, above and beyond global negative affect, anxiety sensitivity, disgust propensity, and disgust sensitivity.
Shafran R, Fairburn CG, Robinson P, Lask B. Body checking and its avoidance in eating disorders. Int J Eat Disord. 2004;35(1):93–101.
Griffen TC, Naumann E, Hildebrandt T. Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin Psychol Rev. 2018;65:163–74.
Johnson WG, Schlundt DG, Jarrell MP. Exposure with response prevention, training in energy balance, and problem solving therapy for bulimia nervosa. Int J Eat Disord. 1988;5(1):35–45.
Rosen JC, Litenberg H. The anxiety model of bulimia nervosa and treatment with exposure plus response prevention. In: The psychobiology of bulimia nervosa. Berlin: Springer; 1988. p. 146–51.
Berg KC, Crosby RD, Cao L, Peterson CB, Engel SG, Mitchell JE, et al. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. J Abnorm Psychol. 2013;122(1):111–8.
Schaefer LM, Smith KE, Anderson LM, Cao L, Crosby RD, Engel SG, et al. The role of affect in the maintenance of binge-eating disorder: evidence from an ecological momentary assessment study. J Abnorm Psychol. 2020;129(4):387–96.
Krypotos AM, Effting M, Kindt M, Beckers T. Avoidance learning: a review of theoretical models and recent developments. Front Behav Neurosci. 2015;9:189.
Arnaudova I, Kindt M, Fanselow M, Beckers T. Pathways towards the proliferation of avoidance in anxiety and implications for treatment. Behav Res Ther. 2017;96:3–13.
Scheveneels S, Boddez Y, Vervliet B, Hermans D. The validity of laboratory-based treatment research: bridging the gap between fear extinction and exposure treatment. Behav Res Ther. 2016;86:87–94.
Vervliet B, Raes F. Criteria of validity in experimental psychopathology: application to models of anxiety and depression. Psychol Med. 2013;43(11):2241–4.
Lissek S, Powers AS, McClure EB, et al. Classical fear conditioning in the anxiety disorders: a meta-analysis. Behav Res Ther. 2005;43(11):1391–424.
Foa EB, McLean CP. The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: the case of OCD and PTSD. Annu Rev Clin Psychol. 2016;12:1–28.
Ougrin D. Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry. 2011;11:200.
Booth DA. Culturally corralled into food abuse: the eating disorders as physiologically reinforced excessive appetites. In: Pirke KM, Vandereycken W, Ploog D, editors. The psychobiology of bulimia nervosa: Springer; 1988;18–32.
Jansen A. A learning model of binge eating: cue reactivity and cue exposure. Behav Res Ther. 1998;36(3):257–72.
Steinglass J, Walsh BT. Habit learning and anorexia nervosa: a cognitive neuroscience hypothesis. Int J Eat Disord. 2006;39(4):267–75.
Leehr EJ, Schag K, Brinkmann A, Ehlis AC, Fallgatter AJ, Zipfel S, et al. Alleged approach-avoidance conflict for food stimuli in binge eating disorder. PLoS One. 2016;11(4):e0152271.
Fricke K, Vogel S. How interindividual differences shape approach-avoidance behavior: relating self-report and diagnostic measures of interindividual differences to behavioral measurements of approach and avoidance. Neurosci Biobehav Rev. 2020;111:30–56.
Armstrong T, Olatunji BO. Pavlovian disgust conditioning as a model for contamination-based OCD: evidence from an analogue study. Behav Res Ther. 2017;93:78–87.
Olatunji BO, McKay D. Disgust and its disorders: theory, assessment, and treatment implications. Washington, DC: American Psychological Association; 2009;9–292.
Spreckelsen PV, Glashouwer KA, Bennik EC, Wessel I, de Jong PJ. Negative body image: relationships with heightened disgust propensity, disgust sensitivity, and self-directed disgust. PLoS One. 2018;13(6):e0198532.
Houben K, Havermans RC. A delicious fly in the soup. The relationship between disgust, obesity, and restraint. Appetite. 2012;58(3):827–30.
Anderson LM, Reilly EE, Thomas JJ, Eddy KT, Franko DL, Hormes JM, et al. Associations among fear, disgust, and eating pathology in undergraduate men and women. Appetite. 2018;125:445–53.
Harvey T, Troop NA, Treasure JL, Murphy T. Fear, disgust, and abnormal eating attitudes: a preliminary study. Int J Eat Disord. 2002;32(2):213–8.
Troop N, Baker A. Food, body, and soul: the role of disgust in eating disorders. In: Olatunji BO, McKay D, editors. Disgust and its disorders: theory, assessment, and treatment implications. Washington, DC: American Psychological Association; 2009. p. 229–51.
McLaughlin KA, Lambert HK. Child trauma exposure and psychopathology: mechanisms of risk and resilience. Curr Opin Psychol. 2017;14:29–34.
McLaughlin KA, DeCross SN, Jovanovic T, Tottenham N. Mechanisms linking childhood adversity with psychopathology: learning as an intervention target. Behav Res Ther. 2019;118:101–9.
Hildebrandt T (2019) Disgust conditioning as a model for food avoidance among adolescents with low-weight eating disorders. Paper presented at: Association for Behavioral and Cognitive Therapies 53rd Annual Convention; Atlanta, GA.
Berg H, Cooper SE, Ross JP, Lissek S (2019) Generalization of conditioned disgust: individual differences and temporal dynamics. Paper presented at: Association for Behavioral and Cognitive Therapies 53rd Annual Convention; Atlanta, GA.
Kaczkurkin AN, Burton PC, Chazin SM, Manbeck AB, Espensen-Sturges T, Cooper SE, et al. Neural substrates of overgeneralized conditioned fear in PTSD. Am J Psychiatry. 2017;174(2):125–34.
Lissek S, Rabin S, Heller RE, Lukenbaugh D, Geraci M, Pine DS, et al. Overgeneralization of conditioned fear as a pathogenic marker of panic disorder [published correction appears in Am J Psychiatry. 2010 Jan;167(1):106]. Am J Psychiatry. 2010;167(1):47–55.
Lissek S, Kaczkurkin AN, Rabin S, Geraci M, Pine DS, Grillon C. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75(11):909–15.
Hunt C, Cooper SE, Hartnell MP, Lissek S. Anxiety sensitivity and intolerance of uncertainty facilitate associations between generalized Pavlovian fear and maladaptive avoidance decisions. J Abnorm Psychol. 2019;128(4):315–26.
Pittig A, Wong AHK, Glück VM, Boschet JM. Avoidance and its bi-directional relationship with conditioned fear: mechanisms, moderators, and clinical implications. Behav Res Ther. 2020;126:103550.
Abramowitz JS, Blakey SM. Overestimation of threat. In: Abramowitz JS, Blakey SM, editors. Clinical handbook of fear and anxiety: maintenance processes and treatment mechanisms: American Psychological Association; 2020. p. 7–25.
Ottaviani C, Watson DR, Meeten F, Makovac E, Garfinkel SN, Critchley HD. Neurobiological substrates of cognitive rigidity and autonomic inflexibility in generalized anxiety disorder. Biol Psychol. 2016;119:31–41.
Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol Med. 2007;37(8):1075–84.
Prefit AB, Cândea DM, Szentagotai-Tătar A. Emotion regulation across eating pathology: a meta-analysis. Appetite. 2019;143:104438.
Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. 2017;57:141–63.
Kaye WH, Bulik CM, Thornton L, Barbarich N, Masters K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161(12):2215–21.
Aharoni R, Hertz MM. Disgust sensitivity and anorexia nervosa. Eur Eat Disord Rev. 2012;20(2):106–10.
Anestis MD, Holm-Denoma JM, Gordon KH, Schmidt NB, Joiner TE. The role of anxiety sensitivity in eating pathology. Cogn Ther Res. 2014;32(3):370–85.
Davey GC, Buckland G, Tantow B, Dallos R. Disgust and eating disorders. Eur Eat Disord Rev. 1998;6(3):201–11.
Harrison A, O’Brien N, Lopez C, Treasure J. Sensitivity to reward and punishment in eating disorders. Psychiatry Res. 2010;177(1–2):1–11.
Jappe LM, Frank GK, Shott ME, et al. Heightened sensitivity to reward and punishment in anorexia nervosa. Int J Eat Disord. 2011;44(4):317–24.
Monteleone AM, Cardi V, Volpe U, Fico G, Ruzzi V, Pellegrino F, et al. Attachment and motivational systems: relevance of sensitivity to punishment for eating disorder psychopathology. Psychiatry Res. 2018;260:353–9.
Troop NA, Treasure JL, Serpell L. A further exploration of disgust in eating disorders. Eur Eat Disord Rev. 2002;10(3):218–26.
Klabunde M, Acheson DT, Boutelle KN, Matthews SC, Kaye WH. Interoceptive sensitivity deficits in women recovered from bulimia nervosa. Eat Behav. 2013;14(4):488–92.
Jenkinson PM, Taylor L, Laws KR. Self-reported interoceptive deficits in eating disorders: a meta-analysis of studies using the eating disorder inventory. J Psychosom Res. 2018;110:38–45.
Brown TA, Berner LA, Jones MD, Reilly EE, Cusack A, Anderson LK, et al. Psychometric evaluation and norms for the Multidimensional Assessment of Interoceptive Awareness (MAIA) in a clinical eating disorders sample. Eur Eat Disord Rev. 2017;25(5):411–6.
Khalsa SS, Craske MG, Li W, Vangala S, Strober M, Feusner JD. Altered interoceptive awareness in anorexia nervosa: effects of meal anticipation, consumption and bodily arousal. Int J Eat Disord. 2015;48(7):889–97.
Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered interoceptive activation before, during, and after aversive breathing load in women remitted from anorexia nervosa. Psychol Med. 2018;48(1):142–54.
Zucker NL, Bulik CM. On bells, saliva, and abdominal pain or discomfort: Early aversive visceral conditioning and vulnerability for anorexia nervosa. Int J Eat Disord. 2020;53(4):508–12 This article briefly reviews emerging evidence for conceptualizing aversive visceral conditioning, early gastrointestinal pain or discomfort, and altered interoceptive processes as key vulnerability factors for later onset and maintenance of anorexia nervosa.
Berner LA, Simmons AN, Wierenga CE, Bischoff-Grethe A, Paulus MP, Bailer UF, et al. Altered anticipation and processing of aversive interoceptive experience among women remitted from bulimia nervosa. Neuropsychopharmacology. 2019;44(7):1265–73.
Kambanis PE, Kuhnle MC, Wons OB, Jo JH, Keshishian AC, Hauser K, et al. Prevalence and correlates of psychiatric comorbidities in children and adolescents with full and subthreshold avoidant/restrictive food intake disorder. Int J Eat Disord. 2020;53(2):256–65.
Zucker NL, Merwin RM, Bulik CM, Moskovich A, Wildes JE, Groh J. Subjective experience of sensation in anorexia nervosa. Behav Res Ther. 2013;51(6):256–65.
Vartanian LR, Herman CP, Polivy J. Consumption stereotypes and impression management: how you are what you eat. Appetite. 2007;48(3):265–77.
Puhl RM, Moss-Racusin CA, Schwartz MB, Brownell KD. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008;23(2):347–58.
Boswell JF, Anderson LM, Anderson DA. Integration of interoceptive exposure in eating disorder treatment. Clin Psychol Sci Pract. 2015;22(2):194–210.
McIntosh VV, Carter FA, Bulik CM, Frampton CM, Joyce PR. Five-year outcome of cognitive behavioral therapy and exposure with response prevention for bulimia nervosa. Psychol Med. 2011;41(5):1061–71.
Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E. Fear of food as a treatment target: exposure and response prevention for anorexia nervosa in an open series. Int J Eat Disord. 2012;45(4):615–21.
Schmidt U, Marks I. Cue exposure to food plus response prevention of binges for bulimia: a pilot study. Int J Eat Disord. 1988;7(5):663–72.
Hildebrandt T. Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin Psychol Rev. 2018;65:163–74.
Craske MG, Treanor M, Conway CC, Zbozinek T, Vervliet B. Maximizing exposure therapy: an inhibitory learning approach. Behav Res Ther. 2014;58:10–23.
Bosman RC, Borg C, de Jong PJ. Optimising extinction of conditioned disgust. PLoS One. 2016;11(2):e0148626.
van’t Wout M, Faucher C, Garnaat S, Philip N, Burwell R. Learning not to avoid: effects of transcranial direct current stimulation on reversal learning. In: Neuropsychopharmacology, vol. 44, no. Suppl 1. London: Nature Publishing Group; 2019. p. 87–8.
van’t Wout-Frank M, Shea MT, Larson VC, Greenberg BD, Philip NS. Combined transcranial direct current stimulation with virtual reality exposure for posttraumatic stress disorder: feasibility and pilot results. Brain Stimul. 2019;12(1):41–3.
Krypotos AM, Engelhard IM. Pavlovian-to-instrumental transfer in subclinical obsessive–compulsive disorder. J Exp Psychopathol. 2020;11(3):2043808720925244.
van Meurs B, Wiggert N, Wicker I, Lissek S. Maladaptive behavioral consequences of conditioned fear-generalization: a pronounced, yet sparsely studied, feature of anxiety pathology. Behav Res Ther. 2014;57:29–37.
Flores A, López FJ, Vervliet B, Cobos PL. Intolerance of uncertainty as a vulnerability factor for excessive and inflexible avoidance behavior. Behav Res Ther. 2018;104:34–43.
Olatunji BO, Sawchuk CN. Disgust: characteristic features, social manifestations, and clinical implications. J Soc Clin Psychol. 2005;24(7):932–62.
Whitton AE, Henry JD, Grisham JR. Cognitive and psychophysiological correlates of disgust in obsessive-compulsive disorder. Br J Clin Psychol. 2015;54(1):16–33.
Klucken T, Schweckendiek J, Koppe G, Merz CJ, Kagerer S, Walter B, et al. Neural correlates of disgust-and fear-conditioned responses. Neuroscience. 2012;201:209–18.
Schweckendiek J, Klucken T, Merz CJ, Kagerer S, Walter B, Vaitl D, et al. Learning to like disgust: neuronal correlates of counterconditioning. Front Hum Neurosci. 2013;7:346.
Kerr KL, Moseman SE, Avery JA, Bodurka J, Zucker NL, Simmons WK. Altered insula activity during visceral interoception in weight-restored patients with anorexia nervosa. Neuropsychopharmacology. 2016;41(2):521–8.
Woody SR, Teachman BA. Intersection of disgust and fear: normative and pathological views. Clin Psychol Sci Pract. 2000;7(3):291–311.
Lissek S, Pine DS, Grillon C. The strong situation: a potential impediment to studying the psychobiology and pharmacology of anxiety disorders. Biol Psychol. 2006;72(3):265–70.
Elsey JW, Kindt M. Breaking boundaries: optimizing reconsolidation-based interventions for strong and old memories. Learn Mem. 2017;24(9):472–9.
Fullana MA, Dunsmoor JE, Schruers KRJ, Savage HS, Bach DR, Harrison BJ. Human fear conditioning: from neuroscience to the clinic. Behav Res Ther. 2020;124:103528.
Rozin P. Food and eating. In: Kitayama S, Cohen D, editors. Handbook of cultural psychology. New York: The Guilford Press. 2010 p. 391–416.
Martins Y, Pliner P. Human food choices: an examination of the factors underlying acceptance/rejection of novel and familiar animal and nonanimal foods. Appetite. 2005;45(3):214–24.
Funding
This research was supported by the National Institute of Mental Health of the National Institutes of Health under award numbers T32MH082761 and K23MH123910. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work. Initial conceptualization and material preparation was performed by Lisa M. Anderson. All authors, Lisa M. Anderson, Hannah Berg, Tiffany A. Brown, Jessie Menzel, and Erin E. Reilly, drafted the work and revised it critically for important intellectual content; read and approved the final manuscript submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethics Approval
Not applicable—no ethical approval was required.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Eating Disorders
Rights and permissions
About this article
Cite this article
Anderson, L.M., Berg, H., Brown, T.A. et al. The Role of Disgust in Eating Disorders. Curr Psychiatry Rep 23, 4 (2021). https://doi.org/10.1007/s11920-020-01217-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s11920-020-01217-5