Abstract
Purpose of Review
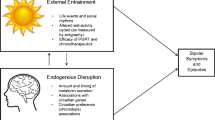
Circadian rhythms are a topic of growing interest in mental health, particularly in obsessive-compulsive disorder. However, the consistency of this link has not been carefully examined. Thus, the present review integrates findings from the past 5 years in order to determine the strength of such a relationship and identify areas for clarification and extension.
Recent Findings
Findings revealed inconsistent evidence for a link between circadian rhythms and OCD. Chronotype is unrelated to OCD symptoms in adolescents but predicts OCD symptoms in adults. Results on delayed sleep timing are equivocal. Circadian rhythm disorders predict OCD treatment outcome. Preliminary evidence implicates decreased light exposure and diurnal symptom variability in OCD.
Summary
The relationship between circadian rhythms and OCD may vary by age, diagnostic status, and assessment method. Recent findings are limited by an overreliance on convenience samples and singular self-report methods. Recommendations for future research on the role of circadian rhythms in OCD are discussed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016;26:R432–43.
Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci. 2010;11:1–11.
Taylor BJ, Hasler BP. Chronotype and mental health: recent advances. Curr Psychiatry Rep. 2018;20:59.
McClung CA. How might circadian rhythms control mood? Let me count the ways. Biol Psychiatry. 2013;74:242–9.
Kronfeld-Schor N, Einat H. Circadian rhythms and mood: human psychopathology and animal models. Neuropsychopharmacol. 2012;62:101–14.
Schubert JR, Coles ME. Obsessive-compulsive symptoms and characteristics in individuals with delayed sleep phase disorder. J Nerv Ment Dis. 2013;201:877–84.
Drummond LM, Wulff K, Rani RS, White S, Mbanga-Sibanda J, Ghodse H, et al. 2012. How should we measure delayed sleep phase shift in severe, refractory obsessive-compulsive disorder? Int J Psychiatry Clin Pract 2012;16:268–276.
Turner J, Drummond LM, Mukhopadhyay S, Ghodse H, White S, Pillay A, et al. A prospective study of delayed sleep phase syndrome in patients with severe resistant obsessive-compulsive disorder. World Psychiatry. 2007;6:08–111.
Kluge M, Schussler P, Kunzel HE, Dresler M, Yassouridis A, Steiger A. Increased nocturnal secretion of ACTH and cortisol in obsessive compulsive disorder. J Psychiatr Res. 2007;41:928–33.
Monteleone P, Catapano F, Tortorella A, Di Martino S, Maj M. Plasma melatonin and cortisol circadian patterns in patients with obsessive-compulsive disorder before and after fluoxetine treatment. Psychoneuroendocrino. 1995;20:763–70.
Catapano F, Monteleone P, Fuschino A, Maj M, Kemali D. Melatonin and cortisol secretion in patients with primary obsessive-compulsive disorder. Psychiatry Res. 1992;44:217–25.
Millet B, Touitou Y, Poirier MF, Bourdel MC, Hantouche E, Bogdan A, et al. Plasma melatonin and cortisol in patients with obsessive-compulsive disorder: relationship with axillary temperature, physical activity, and clinical symptoms. Biol Psychiatry. 1998;44:874–81.
Cox RC, Olatunji BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. 2016;37:104–29.
Nota JA, Sharkey KM, Coles ME. Sleep, arousal, and circadian rhythms in adults with obsessive-compulsive disorder: a meta-analysis. Neurosci Biobehav Rev. 2015;51:100–7.
Duffy JF, Rimmer DW, Czeisler CA. Association of intrinsic circadian period with morningness-eveningness, usual wake time, and circadian phase. Behav Neurosci. 2001;115:895–9.
Bailey SL, Heitkemper MM. Circadian rhythmicity of cortisol and body temperature: morningness-eveningness effects. Chronobiol Int. 2001;18:249–61.
Kerkhof GA, Van Dongen HPA. Morning-type and evening-type individuals differ in the phase position of their endogenous circadian oscillator. Neurosci Lett. 1996;218:153–6.
Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BWJH. Chronotype associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33:75–83.
Nota JA, Coles ME. Duration and timing of sleep are associated with repetitive negative thinking. Cogn Ther Res. 2015;39:253–61.
Alvaro PK, Roberts RM, Harris JK. The independent relationships between insomnia, depression, subtypes of anxiety, and chronotype during adolescence. Sleep Med. 2014;15:934–41.
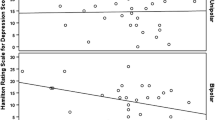
• Cox RC, Tuck B, Olatunji BO. The role of eveningness in obsessive-compulsive symptoms: cross-sectional and prospective approaches. J Affect Disord. 2018;235:448–55 Eveningness predicts OCD symptoms over 4 months, controlling for depression.
• Alvaro PK, Roberts RM, Harris JK, Bruni O. The direction of the relationship between symptoms of insomnia and psychiatric disorders in adolescents. J Affect Disord. 2017;207:167–74 Eveningness does not predict OCD symptoms over 6 months in adolescents.
Kani AS, Poyraz CA, Poyraz BC, Bayar MR, Akin E, Kose S. The role of affective temperaments and chronotype in pharmacotherapy response in patients with obsessive-compulsive disorder. Psychiatry Clin Psychopharmacol. 2018;28:58–65.
Simor P, Harsanyi A, Csigo K, Miklos G, Lazar AS, Demeter G. Eveningness is associated with poor sleep quality and negative affect in obsessive–compulsive disorder. J Behav Addict. 2018;7:10–20.
Coles ME, Schubert JR, Sharkey KM. Delayed bedtimes and obsessive-compulsive symptoms. Behav Sleep Med. 2012;10:258–65.
Roenneberg T. What is chronotype? Sleep Biol Rhythms. 2012;10:75–6.
Kantermann T, Burgess HJ. Average mid-sleep time as a proxy for circadian phase. Psych J. 2017;6:290–1.
Paine SJ, Gander PH. Differences in circadian phase and weekday/weekend sleep patterns in a sample of middle-aged morning types and evening types. Chronobiol Int. 2016;33:1009–17.
Schubert JR, Coles ME. The experience and impact of intrusive thoughts in individuals with late bedtimes. Biol Rhythm Res. 2015;46:81–9.
Nota JA, Schubert JR, Coles ME. Sleep disruption is related to poor response inhibition in individuals with obsessive-compulsive and repetitive negative thought symptoms. J Behav Ther Exp Psychiatry. 2016;50:23–32.
• Donse L, Sack AT, Fitzgerald PB, Arns M. Sleep disturbances in obsessive-compulsive disorder: association with non-response to repetitive transcranial magnetic stimulation (rTMS). J Anxiety Disord. 2017;49:31–9 Adults with OCD report increased symptoms of circadian rhythm disorders compared to healthy controls. Circadian rhythm disorders and bedtime predict treatment outcome.
Jaspers-Fayer F, Lin SY, Belschner L, Mah J, Chan E, Bleakley C, et al. A case-control study of sleep disturbances in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2018;55:1–7.
Sivertsen B, Harvey AG, Pallesen S, Hysing M. Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway. J Sleep Res. 2015;24:11–8.
Nota JA, Gibb BE, Coles ME. Obsessions and time of day: a self-monitoring study in individuals with obsessive-compulsive disorder. J Cogn Psychother. 2014;28:134–44.
Kenardy J, Fried L, Kraemer HC, Taylor CB. Psychological precursors of panic attacks. Br J Psychiatry 1992;160:668–73.
English T, Carstensen LL. Emotional experience in the mornings and the evenings: consideration of age differences in specific emotions by time of day. Front Psychol. 2014;5:1–9.
Willis TA, O’Connor DB, Smith L. The influence of morningness–eveningness on anxiety and cardiovascular responses to stress. Physiol Behav. 2005;85:125–33.
Boland EM, Ross RJ. Recent advances in the study of sleep in the anxiety disorders, obsessive-compulsive disorder, and posttraumatic stress disorder. Psychiatr Clin N Am. 2015;38:761–76.
Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, et al. Epidemiology of the human circadian clock. Sleep Med Rev. 2007;11:429–38.
• Coles ME, Wirshba CJ, Nota J, Schubert J, Grunthal BA. Obsessive compulsive disorder prevalence increases with latitude. J Obsessive-Compulsive Relat Disord. 2018;18:25–30 Higher latitude and fewer hours of light exposure associated with increased OCD prevalence.
Adamsson M, Laike T, Morita T. Annual variation in daily light exposure and circadian change of melatonin and cortisol concentrations at a northern latitude with large seasonal differences in photoperiod length. J Physiol Anthropol. 2017;36:6.
Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8:602–12.
Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–77.
Broussard JL, Reynolds AC, Depner CM, Ferguson SA, Dawson D, Wright KP. Circadian rhythms versus daily patterns in human physiology and behavior. In Kumar V, editor. Biological timekeeping: clocks, rhythms and behaviour. Springer; 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Cox, R.C., Olatunji, B.O. Circadian Rhythms in Obsessive-Compulsive Disorder: Recent Findings and Recommendations for Future Research. Curr Psychiatry Rep 21, 54 (2019). https://doi.org/10.1007/s11920-019-1033-0
Published:
DOI: https://doi.org/10.1007/s11920-019-1033-0