Abstract
Purpose of Review
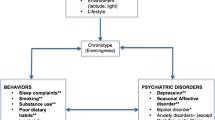
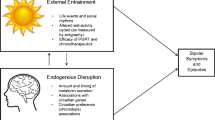
Evening chronotype is increasingly recognized as a correlate of, and perhaps a contributor to, mental illness. The current review evaluates recent evidence for the association between chronotype and mental illness and putative mechanisms underlying the association, while highlighting methodological advances and areas of research that are relatively under-examined in the literature.
Recent Findings
While evening chronotype is most consistently associated with severity of mood disorder symptoms, emerging evidence implicates evening chronotype as a transdiagnostic correlate of substance use severity, anxiety symptoms, attentional difficulties, and maladaptive behaviors such as aggression. Longitudinal studies point to the possibility that evening chronotype precedes problematic substance use, depression, and anxiety. Neural processes related to reward and affective regulation may underlie associations between evening chronotype and illness.
Summary
The literature on chronotype and mental illness has evolved to (1) include associations with a broader range of psychiatric symptom profiles; (2) explore underlying mechanisms; and (3) expand on earlier research using objective measures and more sophisticated study designs. In addition to further mechanistic research, additional work is needed to examine the stability and key subcomponents of the chronotype construct, as well as more attention to pediatric and special populations. This research is needed to clarify the chronotype-mental health relationship, and to identify how, when, and what aspects of chronotype can be targeted via therapeutic interventions.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major Importance
Broms U, Pitkaniemi J, Backmand H, Heikkila K, Koskenvuo M, Peltonen M, et al. Long-term consistency of diurnal-type preferences among men. Chronobiol Int. 2014;31(2):182–8.
Fischer D, Lombardi DA, Marucci-Wellman H, Roenneberg T. Chronotypes in the US—influence of age and sex. PLoS One. 2017;12(6):e0178782.
Randler C, Fassl C, Kalb N. From lark to owl: developmental changes in morningness-eveningness from new-borns to early adulthood. Sci Rep. 2017;7:45874.
Roenneberg T. Q & A: Till Roenneberg Curr Biol : CB 2004;14(11):R405,
Merikanto I, Lahti T, Kronholm E, Peltonen M, Laatikainen T, Vartiainen E, et al. Evening types are prone to depression. Chronobiol Int. 2013;30(5):719–25.
Wood J, Birmaher B, Axelson D, Ehmann M, Kalas C, Monk K, et al. Replicable differences in preferred circadian phase between bipolar disorder patients and control individuals. Psychiatry Res. 2009;166(2–3):201–9.
Murray G, Allen NB, Trinder J. Seasonality and circadian phase delay: prospective evidence that winter lowering of mood is associated with a shift towards Eveningness. J Affect Disord. 2003;76(1–3):15–22.
Caci H, Bouchez J, Bayle FJ. Inattentive symptoms of ADHD are related to evening orientation. J Atten Disord. 2009;13(1):36–41.
Azad-Marzabadi E, Amiri S. Morningness-eveningness and emotion dysregulation incremental validity in predicting social anxiety dimensions. Int J Gen Med. 2017;10:275–9.
Hasler BP, Sitnick SL, Shaw DS, Forbes EE. An altered neural response to reward may contribute to alcohol problems among late adolescents with an evening chronotype. Psychiatry Res. 2013;214(3):357–64.
Schlarb AA, Sopp R, Ambiel D, Grunwald J. Chronotype-related differences in childhood and adolescent aggression and antisocial behavior—a review of the literature. Chronobiol Int. 2014;31(1):1–16.
Muller MJ, Haag A. The concept of chronotypes and its clinical importance for depressive disorders. Int J Psychiatry Med. 2018;53(3):224–40.
• Au J, Reece J. The relationship between chronotype and depressive symptoms: a meta-analysis. J Affect Disord. 2017;218:93–104. A meta-analysis of 36 studies showed that the size of the association was small but significant. Effect sizes were significantly larger when studies used the Composite Scale of Morningness as the measure of chronotype.
Johansson C, Willeit M, Smedh C, Ekholm J, Paunio T, Kieseppä T, et al. Circadian clock-related polymorphisms in seasonal affective disorder and their relevance to diurnal preference. Neuropsychopharmacology. 2003;28(4):734–9.
Johansson C, Willeit M, Smedh C, Ekholm J, Paunio T, Kieseppa T, et al. Circadian clock-related polymorphisms in seasonal affective disorder and their relevance to diurnal preference. Neuropsychopharmacol: Off Publ Am Coll Neuropsychopharmacol. 2003;28(4):734–9.
Dimitrov A, Veer IM, Kleeblatt J, Seyfarth F, Roenneberg T, Ising M, Uhr M, Keck ME, Kramer A, Berger M, von Koch L, Walter H, Adli M Chronotype is associated with psychological well-being depending on the composition of the study sample. J Health Psychol 2018:1359105317751618, 135910531775161.
Rumble ME, Dickson D, McCall WV, Krystal AD, Case D, Rosenquist PB, et al. The relationship of person-specific eveningness chronotype, greater seasonality, and less rhythmicity to suicidal behavior: a literature review. J Affect Disord. 2018;227:721–30.
Giglio LM, Magalhaes PV, Andersen ML, Walz JC, Jakobson L, Kapczinski F. Circadian preference in bipolar disorder. Sleep Breath. 2010;14(2):153–5.
Melo MCA, Abreu RLC, Linhares Neto VB, de Bruin PFC, de Bruin VMS. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev. 2017;34:46–58.
Gershon A, Kaufmann CN, Depp CA, Miller S, Do D, Zeitzer JM, et al. Subjective versus objective evening chronotypes in bipolar disorder. J Affect Disord. 2018;225:342–9.
Seleem MA, Merranko JA, Goldstein TR, Goldstein BI, Axelson DA, Brent DA, et al. The longitudinal course of sleep timing and circadian preferences in adults with bipolar disorder. Bipolar Disord. 2015;17(4):392–402.
Baek JH, Kim JS, Kim MJ, Ryu S, Lee K, Ha K, et al. Lifetime characteristics of evening-preference and irregular bed-rise time are associated with lifetime seasonal variation of mood and behavior: comparison between individuals with bipolar disorder and healthy controls. Behav Sleep Med. 2016;14(2):155–68.
Kanagarajan K, Gou K, Antinora C, Buyukkurt A, Crescenzi O, Beaulieu S, et al. Morningness-Eveningness questionnaire in bipolar disorder. Psychiatry Res. 2018;262:102–7.
Subramanian K, Sarkar S, Kattimani S. Bipolar disorder in Asia: illness course and contributing factors. Asian J Psychiatr. 2017;29:16–29.
Alloy LB, Ng TH, Titone MK, Boland EM. Circadian rhythm dysregulation in bipolar spectrum disorders. Curr Psychiatry Rep. 2017;19(4):21.
Pirkola S, Eriksen HA, Partonen T, Kieseppa T, Veijola J, Jaaskelainen E, et al. Seasonal variation in affective and other clinical symptoms among high-risk families for bipolar disorders in an Arctic population. Int J Circumpolar Health. 2015;74:29671.
Zanini MA, Castro J, Cunha GR, Asevedo E, Pan PM, Bittencourt L, et al. Abnormalities in sleep patterns in individuals at risk for psychosis and bipolar disorder. Schizophr Res. 2015;169(1–3):262–7.
Castro J, Zanini M, Goncalves Bda S, Coelho FM, Bressan R, Bittencourt L, et al. Circadian rest-activity rhythm in individuals at risk for psychosis and bipolar disorder. Schizophr Res. 2015;168(1–2):50–5.
Ng TH, Chung KF, Ng TK, Lee CT, Chan MS. Correlates and prognostic relevance of sleep irregularity in inter-episode bipolar disorder. Compr Psychiatry. 2016;69:155–62.
Taylor BJ, Hasler BP, Roecklein KA, Hall MH. Chronotype and risk taking: a review of the literature with an emphasis on adolescence and sex differences. Chronobiol Int Under Rev.
Hasler BP, Casement MD, Sitnick SL, Shaw DS, Forbes EE. Eveningness among late adolescent males predicts neural reactivity to reward and alcohol dependence 2 years later. Behav Brain Res. 2017;327:112–20.
• Hasler BP, Franzen PL, de Zambotti M, Prouty D, Brown SA, Tapert SF, et al. Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: initial findings from the National Consortium on alcohol and neurodevelopment in adolescence study. Alcohol Clin Exp Res. 2017;41(6):1154–65. This longitudinal study found that eveningness predicted greater alcohol dependence two years later in late adolescent males. The association between evening chronotype and alcohol dependence was mediated via medial prefrontal cortex reactivity to monetary reward, suggesting that altered reward functioning may be a mechanism underlying the association between chronotype and suboptimal functioning.
Prat G, Adan A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiol Int. 2011;28(3):248–57.
Watson NF, Buchwald D, Harden KP. A twin study of genetic influences on diurnal preference and risk for alcohol use outcomes. J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med. 2013;9(12):1333–9.
Tavernier R, Munroe M, Willoughby T. Perceived morningness-eveningness predicts academic adjustment and substance use across university, but social jetlag is not to blame. Chronobiol Int. 2015;32(9):1233–45.
Haynie DL, Lewin D, Luk JW, Lipsky LM, O'Brien F, Iannotti RJ, et al. Beyond sleep duration: bidirectional associations between chronotype, social jetlag, and drinking behaviors in a longitudinal sample of US high school students. Sleep. 2017;
Nowakowska-Domagala K, Mokros L, Jablkowska-Gorecka K, Grzelinska J, Pietras T. The relationship between chronotype and personality among patients with alcohol dependence syndrome: pilot study. Chronobiol Int. 2016;33(10):1351–8.
• Coogan AN, McGowan NM. A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. Attention Deficit and Hyperactivity Disorders. 2017;9(3):129–47. A systematic review of studies examining associations between circadian factors and attention deficit hyperactivity disorder (ADHD) found that ADHD was consistently associated with greater eveningness as well as bio-markers of circadian delay such as dim-light melatonin onset. This review demonstrates that evening chronotype may represent a transdiagnostic risk factor for mental illness above and beyond mood disorders.
Passos GS, Santana MG, Poyares D, D'Aurea CV, Teixeira AA, Tufik S, et al. Chronotype and anxiety are associated in patients with chronic primary insomnia. Rev Bras Psiquiatr (Sao Paulo, Brazil : 1999). 2017;39(2):183–6.
Fares S, Hermens DF, Naismith SL, White D, Hickie IB, Robillard R. Clinical correlates of chronotypes in young persons with mental disorders. Chronobiol Int. 2015;32(9):1183–91.
Antypa N, Vogelzangs N, Meesters Y, Schoevers R, Penninx BW. CHRONOTYPE associations with depression and anxiety disorders in a large cohort study. Depress Anxiety. 2016;33(1):75–83.
Evans DS, Snitker S, Wu SH, Mody A, Njajou OT, Perlis ML, et al. Habitual sleep/wake patterns in the Old Order Amish: heritability and association with non-genetic factors. Sleep. 2011;34(5):661–9.
Hur YM. Stability of genetic influence on morningness-eveningness: a cross-sectional examination of South Korean twins from preadolescence to young adulthood. J Sleep Res. 2007;16(1):17–23.
Toomey R, Panizzon MS, Kremen WS, Franz CE, Lyons MJ. A twin-study of genetic contributions to morningness-eveningness and depression. Chronobiol Int. 2015;32(3):303–9.
Sebela A, Novak T, Kemlink D, Goetz M. Sleep characteristics in child and adolescent offspring of parents with bipolar disorder: a case control study. BMC Psychiatry. 2017;17(1):199.
• Lane JM, Vlasac I, Anderson SG, Kyle SD, Dixon WG, Bechtold DA, et al. Genome-wide association analysis identifies novel loci for chronotype in 100,420 individuals from the UK Biobank. Nat Commun. 2016;7:10889. A genome-wide association analysis (GWAS) found that gene loci associated with chronotype were overrepresented in genes associated with fear and behavioral defense responses using a gene-set enrichment analysis, suggesting that evening chronotypes may be predisposed to mental health disturbances through a behavioral inhibition pathway. Chronotype appeared to share an underlying genetic pathway with schizophrenia but not with mood disorders, despite significant correlations between self-reported chronotype and self-reported depression.
Suzuki M, Dallaspezia S, Locatelli C, Lorenzi C, Uchiyama M, Colombo C, et al. CLOCK gene variants associated with the discrepancy between subjective and objective severity in bipolar depression. J Affect Disord. 2017;210:14–8.
Liberman AR, Kwon SB, Vu HT, Filipowicz A, Ay A, Ingram KK. Circadian clock model supports molecular link between PER3 and human anxiety. Sci Rep. 2017;7(1):9893.
Jankowski KS, Dmitrzak-Weglarz M. ARNTL, CLOCK and PER3 polymorphisms—links with chronotype and affective dimensions. Chronobiol Int. 2017;34(8):1105–13.
Viena TD, Gobin CM, Fins AI, Craddock TJ, Tartar A, Tartar JL. A PER3 polymorphism interacts with sleep duration to influence transient mood states in women. J Circadian Rhythms. 2016;14:3.
Chiu WH, Yang HJ, Kuo PH. Chronotype preference matters for depression in youth. Chronobiol Int. 2017;34(7):933–41.
Bakotic M, Radosevic-Vidacek B, Koscec Bjelajac A. Morningness-eveningness and daytime functioning in university students: the mediating role of sleep characteristics. J Sleep Res. 2017;26(2):210–8.
Simor P, Zavecz Z, Palosi V, Torok C, Koteles F. The influence of sleep complaints on the association between chronotype and negative emotionality in young adults. Chronobiol Int. 2015;32(1):1–10.
Selvi Y, Boysan M, Kandeger A, Uygur OF, Sayin AA, Akbaba N, et al. Heterogeneity of sleep quality in relation to circadian preferences and depressive symptomatology among major depressive patients. J Affect Disord. 2018;235:242–9.
Muller MJ, Kundermann B, Cabanel N. Eveningness and poor sleep quality independently contribute to self-reported depression severity in psychiatric inpatients with affective disorder. Nord J Psychiatry. 2016;70(5):329–34.
Mokros L, Witusik A, Michalska J, Lezak W, Panek M, Nowakowska-Domagala K, et al. Sleep quality, chronotype, temperament and bipolar features as predictors of depressive symptoms among medical students. Chronobiol Int. 2017;34(6):708–20.
Togo F, Yoshizaki T, Komatsu T. Association between depressive symptoms and morningness-eveningness, sleep duration and rotating shift work in Japanese nurses. Chronobiol Int. 2017;34(3):349–59.
Kitamura S, Hida A, Watanabe M, Enomoto M, Aritake-Okada S, Moriguchi Y, et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiol Int. 2010;27(9–10):1797–812.
Alvaro PK, Roberts RM, Harris JK, Bruni O. The direction of the relationship between symptoms of insomnia and psychiatric disorders in adolescents. J Affect Disord. 2017;207:167–74.
Gobin CM, Banks JB, Fins AI, Tartar JL. Poor sleep quality is associated with a negative cognitive bias and decreased sustained attention. J Sleep Res. 2015;24(5):535–42.
Lau EY, Hui CH, Lam J, Cheung SF. Sleep and optimism: a longitudinal study of bidirectional causal relationship and its mediating and moderating variables in a Chinese student sample. Chronobiol Int. 2017;34(3):360–72.
Bei B, Ong JC, Rajaratnam SM, Manber R. Chronotype and improved sleep efficiency independently predict depressive symptom reduction after group cognitive behavioral therapy for insomnia. J Clin Sleep Med : JCSM : Off Publ Am Acad Sleep Med 2015;11(9):1021–1027.
Simor P, Harsanyi A, Csigo K, Miklos G, Lazar AS, Demeter G. Eveningness is associated with poor sleep quality and negative affect in obsessive-compulsive disorder. J Behav Addict. 2018;7(1):10–20.
Revell VL, Skene DJ. Light-induced melatonin suppression in humans with polychromatic and monochromatic light. Chronobiol Int. 2007;24(6):1125–37.
Ruger M, St Hilaire MA, Brainard GC, Khalsa SB, Kronauer RE, Czeisler CA, et al. Human phase response curve to a single 6.5 h pulse of short-wavelength light. J Physiol. 2013;591(1):353–63.
Bedrosian TA, Nelson RJ. Timing of light exposure affects mood and brain circuits. Transl Psychiatry. 2017;7(1):e1017.
Min JY, Min KB. Outdoor light at night and the prevalence of depressive symptoms and suicidal behaviors: a cross-sectional study in a nationally representative sample of Korean adults. J Affect Disord. 2018;227:199–205.
Obayashi K, Saeki K, Kurumatani N. Bedroom light exposure at night and the incidence of depressive symptoms: a longitudinal study of the HEIJO-KYO cohort. Am J Epidemiol. 2018;187(3):427–34.
Borniger JC, Maurya SK, Periasamy M, Nelson RJ. Acute dim light at night increases body mass, alters metabolism, and shifts core body temperature circadian rhythms. Chronobiol Int. 2014;31(8):917–25.
Vollmer C, Jankowski KS, Diaz-Morales JF, Itzek-Greulich H, Wust-Ackermann P, Randler C. Morningness-eveningness correlates with sleep time, quality, and hygiene in secondary school students: a multilevel analysis. Sleep Med. 2017;30:151–9.
Keller LK, Grunewald B, Vetter C, Roenneberg T, Schulte-Korne G. Not later, but longer: sleep, chronotype and light exposure in adolescents with remitted depression compared to healthy controls. Eur Child Adolesc Psychiatry. 2017;26(10):1233–44.
Zhang L, Evans DS, Raheja UK, Stephens SH, Stiller JW, Reeves GM, et al. Chronotype and seasonality: morningness is associated with lower seasonal mood and behavior changes in the Old Order Amish. J Affect Disord. 2015;174:209–14.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23(1–2):497–509.
Levandovski R, Dantas G, Fernandes LC, Caumo W, Torres I, Roenneberg T, et al. Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol Int. 2011;28(9):771–8.
Borisenkov MF, Petrova NB, Timonin VD, Fradkova LI, Kolomeichuk SN, Kosova AL, et al. Sleep characteristics, chronotype and winter depression in 10-20-year-olds in northern European Russia. J Sleep Res. 2015;24(3):288–95.
de Souza CM, Hidalgo MP. Midpoint of sleep on school days is associated with depression among adolescents. Chronobiol Int. 2014;31(2):199–205.
Knapen SE, Riemersma-van der Lek RF, Antypa N, Meesters Y, Penninx B, Schoevers RA. Social jetlag and depression status: results obtained from the Netherlands Study of Depression and Anxiety. Chronobiol Int 2018;35(1):1–7.
Lin WH, Yi CC. Unhealthy sleep practices, conduct problems, and daytime functioning during adolescence. J Youth Adolesc. 2015;44(2):431–46.
Randler C, Vollmer C. Aggression in young adults—a matter of short sleep and social jetlag? Psychol Rep. 2013;113(3):754–65.
McGowan NM, Voinescu BI, Coogan AN. Sleep quality, chronotype and social jetlag differentially associate with symptoms of attention deficit hyperactivity disorder in adults. Chronobiol Int. 2016;33(10):1433–43.
Horne CM, Norbury R. Late chronotype is associated with enhanced amygdala reactivity and reduced fronto-limbic functional connectivity to fearful versus happy facial expressions. NeuroImage. 2018;171:355–63.
Jensen JL, Jones CR, Kartsonaki C, Packer KA, Adler FR, Liou TG. Sleep phase delay in cystic fibrosis: a potential new manifestation of cystic fibrosis transmembrane regulator dysfunction. Chest. 2017;152(2):386–93.
Dutra SJ, Cunningham WA, Kober H, Gruber J. Elevated striatal reactivity across monetary and social rewards in bipolar I disorder. J Abnorm Psychol. 2015;124(4):890–904.
Byrd AL, Hawes SW, Burke JD, Loeber R, Pardini DA. Boys with conduct problems and callous-unemotional traits: neural response to reward and punishment and associations with treatment response. Dev Cogn Neurosci. 2017;30:51–9.
Tenenbaum RB, Musser ED, Raiker JS, Coles EK, Gnagy EM, Pelham WE, Jr. Specificity of reward sensitivity and parasympathetic-based regulation among children with attention-deficit/hyperactivity and disruptive behavior disorders. J Abnorm Child Psychol 2017.
Knutson B, Wimmer GE, Kuhnen CM, Winkielman P. Nucleus accumbens activation mediates the influence of reward cues on financial risk taking. Neuroreport. 2008;19(5):509–13.
Goldstein RZ, Parvaz MA, Maloney T, Alia-Klein N, Woicik PA, Telang F, et al. Compromised sensitivity to monetary reward in current cocaine users: an ERP study. Psychophysiology. 2008;45(5):705–13.
Stewart JL, Flagan TM, May AC, Reske M, Simmons AN, Paulus MP. Young adults at risk for stimulant dependence show reward dysfunction during reinforcement-based decision making. Biol Psychiatry. 2013;73(3):235–41.
Balodis IM, Kober H, Worhunsky PD, Stevens MC, Pearlson GD, Potenza MN. Diminished frontostriatal activity during processing of monetary rewards and losses in pathological gambling. Biol Psychiatry. 2012;71(8):749–57.
Oberg SA, Christie GJ, Tata MS. Problem gamblers exhibit reward hypersensitivity in medial frontal cortex during gambling. Neuropsychologia. 2011;49(13):3768–75.
Parekh PK, McClung CA. Circadian mechanisms underlying reward-related neurophysiology and synaptic plasticity. Front Psychiatry. 2015;6:187.
Song J, Feng P, Zhao X, Xu W, Xiao L, Zhou J, et al. Chronotype regulates the neural basis of response inhibition during the daytime. Chronobiol Int. 2018;35(2):208–18.
Kang JI, Park CI, Sohn SY, Kim HW, Namkoong K, Kim SJ. Circadian preference and trait impulsivity, sensation-seeking and response inhibition in healthy young adults. Chronobiol Int. 2015;32(2):235–41.
Russo PM, Leone L, Penolazzi B, Natale V. Circadian preference and the big five: the role of impulsivity and sensation seeking. Chronobiol Int. 2012;29(8):1121–6.
Berdynaj D, Boudissa SN, Grieg MS, Hope C, Mahamed SH, Norbury R. Effect of chronotype on emotional processing and risk taking. Chronobiol Int. 2016;33(4):406–18.
Muller MJ, Olschinski C, Kundermann B, Cabanel N. Patterns of self-reported depressive symptoms in relation to morningness-eveningness in inpatients with a depressive disorder. Psychiatry Res. 2016;239:163–8.
Antypa N, Verkuil B, Molendijk M, Schoevers R, Penninx B, Van Der Does W. Associations between chronotypes and psychological vulnerability factors of depression. Chronobiol Int. 2017;34(8):1125–35.
Lester D. Morningness-eveningness, current depression, and past suicidality. Psychol Rep. 2015;116(2):331–6.
Pace-Schott EF, Rubin ZS, Tracy LE, Spencer RM, Orr SP, Verga PW. Emotional trait and memory associates of sleep timing and quality. Psychiatry Res. 2015;229(3):999–1010.
Sheaves B, Porcheret K, Tsanas A, Espie CA, Foster RG, Freeman D, et al. Insomnia, nightmares, and chronotype as markers of risk for severe mental illness: results from a student population. Sleep. 2016;39(1):173–81.
Jeong Jeong H, Moon E, Min Park J, Dae Lee B, Min Lee Y, Choi Y, et al. The relationship between chronotype and mood fluctuation in the general population. Psychiatry Res. 2015;229(3):867–71.
Park CI, An SK, Kim HW, Koh MJ, Namkoong K, Kang JI, et al. Relationships between chronotypes and affective temperaments in healthy young adults. J Affect Disord. 2015;175:256–9.
Watts AL, Norbury R. Reduced effective emotion regulation in night owls. J Biol Rhythm. 2017;32(4):369–75.
Taylor BJ, Bowman MA, Hasler BP, Brindle A, Roecklein KA, Krafty RT, et al. Is emotion regulation a mediator of the association between chronotype and alcohol use disorder severity in college students? Journal of biological rhythms. Under Rev.
Haraden DA, Mullin BC, Hankin BL. The relationship between depression and chronotype: a longitudinal assessment during childhood and adolescence. Depress Anxiety. 2017;34(10):967–76.
Roenneberg T, Merrow M. Entrainment of the human circadian clock. Cold Spring Harb Symp Quant Biol. 2007;72:293–9.
Ortiz A, Bradler K, Radu L, Alda M, Rusak B. Exponential state transition dynamics in the rest-activity architecture of patients with bipolar disorder. Bipolar Disord. 2016;18(2):116–23.
Merikanto I, Partonen T, Paunio T, Castaneda AE, Marttunen M, Urrila AS. Advanced phases and reduced amplitudes are suggested to characterize the daily rest-activity cycles in depressed adolescent boys. Chronobiol Int. 2017;34(7):967–76.
Swanson LM, Burgess HJ, Huntley ED, Bertram H, Mooney A, Zollars J, et al. Relationships between circadian measures, depression, and response to antidepressant treatment: a preliminary investigation. Psychiatry Res. 2017;252:262–9.
Murray JM, Sletten TL, Magee M, Gordon C, Lovato N, Bartlett DJ, et al. Prevalence of circadian misalignment and its association with depressive symptoms in delayed sleep phase disorder. Sleep 2017;40(1):zsw002.
Nováková M, Praško J, Látalová K, Sládek M, Sumová A. The circadian system of patients with bipolar disorder differs in episodes of mania and depression. Bipolar Disord. 2015;17(3):303–14.
Mongrain V, Carrier J, Dumont M. Circadian and homeostatic sleep regulation in morningness-eveningness. J Sleep Res. 2006;15(2):162–6.
Kerkhof GA. Inter-individual differences in the human circadian system: a review. Biol Psychol. 1985;20(2):83–112.
Adan A, Lachica J, Caci H, Natale V. Circadian typology and temperament and character personality dimensions. Chronobiol Int. 2010;27(1):181–93.
Duggan KA, Friedman HS, McDevitt EA, Mednick SC. Personality and healthy sleep: the importance of conscientiousness and neuroticism. PLoS One. 2014;9(3):e90628.
Hampson SE, Goldberg LR. A first large cohort study of personality trait stability over the 40 years between elementary school and midlife. J Pers Soc Psychol. 2006;91(4):763–79.
Hasler BP, Buysse DJ, Germain A. Shifts toward morningness during behavioral sleep interventions are associated with improvements in depression, positive affect, and sleep quality. Behav Sleep Med. 2016;14(6):624–35.
Corruble E, Frank E, Gressier F, Courtet P, Bayle F, Llorca PM, et al. Morningness-eveningness and treatment response in major depressive disorder. Chronobiol Int. 2014;31(2):283–9.
Bogen S, Legenbauer T, Gest S, Holtmann M. Morning bright light therapy: a helpful tool for reducing comorbid symptoms of affective and behavioral dysregulation in juvenile depressed inpatients? A pilot trial. Z Kinder Jugendpsychiatr Psychother. 2017;45(1):34–41.
Muller MJ, Cabanel N, Olschinski C, Jochim D, Kundermann B. Chronotypes in patients with nonseasonal depressive disorder: distribution, stability and association with clinical variables. Chronobiol Int. 2015;32(10):1343–51.
Caci H, Mattei V, Bayle FJ, Nadalet L, Dossios C, Robert P, et al. Impulsivity but not venturesomeness is related to morningness. Psychiatry Res. 2005;134(3):259–65.
Di Milia L, Smolensky MH, Costa G, Howarth HD, Ohayon MM, Philip P. Demographic factors, fatigue, and driving accidents: an examination of the published literature. Accid Anal Prev. 2011;43(2):516–32.
Urban R, Magyarodi T, Rigo A. Morningness-eveningness, chronotypes and health-impairing behaviors in adolescents. Chronobiol Int. 2011;28(3):238–47.
Konttinen H, Kronholm E, Partonen T, Kanerva N, Mannisto S, Haukkala A. Morningness-eveningness, depressive symptoms, and emotional eating: a population-based study. Chronobiol Int. 2014;31(4):554–63.
Jankowski KS. Morningness-eveningness and depressive symptoms: test on the components level with CES-D in Polish students. J Affect Disord. 2016;196:47–53.
Putilov AA. State- and trait-like variation in morning and evening components of morningness-eveningness in winter depression. Nordic J Psychiatry. 2017;71(8):561–9.
Randler C. Association between morningness-eveningness and mental and physical health in adolescents. Psychol, Health Med. 2011;16(1):29–38.
Kessler RC. The global burden of anxiety and mood disorders: putting the European Study of the Epidemiology of Mental Disorders (ESEMeD) findings into perspective. J Clin Psychiatry. 2007;68(Suppl 2):10–9.
Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–91.
Randler C, Bilger S. Associations among sleep, chronotype, parental monitoring, and pubertal development among German adolescents. J Psychol. 2009;143(5):509–20.
Crowley SJ, Van Reen E, LeBourgeois MK, Acebo C, Tarokh L, Seifer R, et al. A longitudinal assessment of sleep timing, circadian phase, and phase angle of entrainment across human adolescence. PLoS One. 2014;9(11):e112199.
Melke J, Goubran Botros H, Chaste P, Betancur C, Nygren G, Anckarsater H, et al. Abnormal melatonin synthesis in autism spectrum disorders. Mol Psychiatry. 2008;13(1):90–8.
Tordjman S, Anderson GM, Kermarrec S, Bonnot O, Geoffray MM, Brailly-Tabard S, et al. Altered circadian patterns of salivary cortisol in low-functioning children and adolescents with autism. Psychoneuroendocrinology. 2014;50:227–45.
Yang Z, Matsumoto A, Nakayama K, Jimbo EF, Kojima K, Nagata K, et al. Circadian-relevant genes are highly polymorphic in autism spectrum disorder patients. Brain Dev. 2016;38(1):91–9.
Goldman SE, Surdyka K, Cuevas R, Adkins K, Wang L, Malow BA. Defining the sleep phenotype in children with autism. Dev Neuropsychol. 2009;34(5):560–73.
Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, et al. Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. J Autism Dev Disord. 2006;36(7):849–61.
Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):e1203–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Sleep Disorders
Rights and permissions
About this article
Cite this article
Taylor, B.J., Hasler, B.P. Chronotype and Mental Health: Recent Advances. Curr Psychiatry Rep 20, 59 (2018). https://doi.org/10.1007/s11920-018-0925-8
Published:
DOI: https://doi.org/10.1007/s11920-018-0925-8