Abstract
Purpose of Review
Walking impairments are highly prevalent in persons with multiple sclerosis (PwMS) and are associated with reduced quality of life. Walking is traditionally quantified with various measures, including patient self-reports, clinical rating scales, performance measures, and advanced lab-based movement analysis techniques. Yet, the majority of these measures do not fully characterize walking (i.e., gait quality) nor adequately reflect walking in the real world (i.e., community ambulation) and have limited timescale (only measure walking at a single point in time). We discuss the potential of wearable sensors to provide sensitive, objective, and easy-to-use assessment of community ambulation in PwMS.
Recent Findings
Wearable technology has the ability to measure all aspects of gait in PwMS yet is under-studied in comparison with other populations (e.g., older adults). Within the studies focusing on PwMS, half that measure pace collected free-living data, while only one study explored gait variability in free-living conditions. No studies explore gait asymmetry or complexity in free-living conditions.
Summary
Wearable technology has the ability to provide objective, comprehensive, and sensitive measures of gait in PwMS. Future research should investigate this technology’s ability to accurately assess free-living measures of gait quality, specifically gait asymmetry and complexity.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Society NMS. What is MS? 2019 [cited 2019; Available from: https://www.nationalmssociety.org/What-is-MS. Accessed 11 June 2019.
Keegan BM, Noseworthy JH. Multiple sclerosis. Annu Rev Med. 2002;53:285–302.
Society NMS. What causes MS? 2019; Available from: https://www.nationalmssociety.org/What-is-MS/What-Causes-MS. Accessed 11 June 2019.
Cameron MH, Nilsagard Y. Balance, gait, and falls in multiple sclerosis. Handb Clin Neurol. 2018;159:237–50.
Motl RW, Learmonth YC. Neurological disability and its association with walking impairment in multiple sclerosis: brief review. Neurodegener Dis Manag. 2014;4(6):491–500.
VanSwearingen JM, Studenski SA. Aging, motor skill, and the energy cost of walking: implications for the prevention and treatment of mobility decline in older persons. J Gerontol A Biol Sci Med Sci. 2014;69(11):1429–36.
Capaday C. The special nature of human walking and its neural control. Trends Neurosci. 2002;25(7):370–6.
Lord S, Galna B, Rochester L. Moving forward on gait measurement: toward a more refined approach. Mov Disord. 2013;28(11):1534–43.
Lipsitz LA, Goldberger AL. Loss of ‘complexity’ and aging. Potential applications of fractals and chaos theory to senescence. JAMA. 1992;267(13):1806–9.
Goldberger AL, Peng CK, Lipsitz LA. What is physiologic complexity and how does it change with aging and disease? Neurobiol Aging. 2002;23(1):23–6.
Stergiou N, Decker LM. Human movement variability, nonlinear dynamics, and pathology: is there a connection? Hum Mov Sci. 2011;30(5):869–88.
•• Comber L, Galvin R, Coote S. Gait deficits in people with multiple sclerosis: a systematic review and meta-analysis. Gait Posture. 2017;51:25–35. A recent systematic review discussing the impact of multiple sclerosis on spatiotemporal parameters of gait in lab-based settings.
Givon U, Zeilig G, Achiron A. Gait analysis in multiple sclerosis: characterization of temporal-spatial parameters using GAITRite functional ambulation system. Gait Posture. 2009;29(1):138–42.
Moon Y, et al. Stride-time variability and fall risk in persons with multiple sclerosis. Mult Scler Int. 2015;2015:964790.
Kalron A. Gait variability across the disability spectrum in people with multiple sclerosis. J Neurol Sci. 2016;361:1–6.
Socie MJ, Motl RW, Pula JH, Sandroff BM, Sosnoff JJ. Gait variability and disability in multiple sclerosis. Gait Posture. 2013;38(1):51–5.
Larocca NG. Impact of walking impairment in multiple sclerosis: perspectives of patients and care partners. Patient. 2011;4(3):189–201.
Hobart J, et al. The multiple sclerosis impact scale (MSIS-29): a new patient-based outcome measure. Brain. 2001;124(Pt 5):962–73.
Martin CL, Phillips BA, Kilpatrick TJ, Butzkueven H, Tubridy N, McDonald E, et al. Gait and balance impairment in early multiple sclerosis in the absence of clinical disability. Mult Scler. 2006;12(5):620–8.
Solomon AJ, Jacobs JV, Lomond KV, Henry SM. Detection of postural sway abnormalities by wireless inertial sensors in minimally disabled patients with multiple sclerosis: a case-control study. J Neuroeng Rehabil. 2015;12:74.
Sosnoff JJ, Sandroff BM, Motl RW. Quantifying gait abnormalities in persons with multiple sclerosis with minimal disability. Gait Posture. 2012;36(1):154–6.
Goldman MD, Marrie RA, Cohen JA. Evaluation of the six-minute walk in multiple sclerosis subjects and healthy controls. Mult Scler. 2008;14(3):383–90.
Motl RW, Goldman MD, Benedict RH. Walking impairment in patients with multiple sclerosis: exercise training as a treatment option. Neuropsychiatr Dis Treat. 2010;6:767–74.
Goldman MD, Motl RW, Rudick RA. Possible clinical outcome measures for clinical trials in patients with multiple sclerosis. Ther Adv Neurol Disord. 2010;3(4):229–39.
Motl RW, Cohen JA, Benedict R, Phillips G, LaRocca N, Hudson LD, et al. Validity of the timed 25-foot walk as an ambulatory performance outcome measure for multiple sclerosis. Mult Scler. 2017;23(5):704–10.
Gijbels D, Dalgas U, Romberg A, de Groot V, Bethoux F, Vaney C, et al. Which walking capacity tests to use in multiple sclerosis? A multicentre study providing the basis for a core set. Mult Scler. 2012;18(3):364–71.
Hobart J, Blight AR, Goodman A, Lynn F, Putzki N. Timed 25-foot walk: direct evidence that improving 20% or greater is clinically meaningful in MS. Neurology. 2013;80(16):1509–17.
Kalron A, Aloni R. Contrasting relationship between depression, quantitative gait characteristics and self-report walking difficulties in people with multiple sclerosis. Mult Scler Relat Disord. 2018;19:1–5.
Bennett SE, Bromley LE, Fisher NM, Tomita MR, Niewczyk P. Validity and reliability of four clinical gait measures in patients with multiple sclerosis. Int J MS Care. 2017;19(5):247–52.
Cofre Lizama LE, et al. The use of laboratory gait analysis for understanding gait deterioration in people with multiple sclerosis. Mult Scler. 2016;22(14):1768–76.
Peebles AT, Reinholdt A, Bruetsch AP, Lynch SG, Huisinga JM. Dynamic margin of stability during gait is altered in persons with multiple sclerosis. J Biomech. 2016;49(16):3949–55.
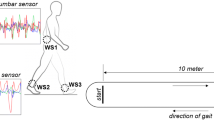
•• Moon Y, et al. Monitoring gait in multiple sclerosis with novel wearable motion sensors. PLoS One. 2017;12(2):e0171346. This article provides detailed descriptions of validity of flexible adherable sensors to quantify gait quality including rhythm across a range of disability in PwMS. This suggests that sensor-based assessment is able to distinguish levels of disability.
•• McGinnis RS, et al. A machine learning approach for gait speed estimation using skin-mounted wearable sensors: from healthy controls to individuals with multiple sclerosis. PLoS One. 2017;12(6). This article provides a major advancement by showing that machine learning algorithms can be used to accurately measure gait speed using wearable conformal sensors and that gait speed is correlated to EDSS in PwMS. This suggests the feasibility of measuring parameters such as gait speed in the home environment to characterize mobility impairment and its fluctuations.
Spain RI, St. George RJ, Salarian A, Mancini M, Wagner JM, Horak FB, et al. Body-worn motion sensors detect balance and gait deficits in people with multiple sclerosis who have normal walking speed. Gait Posture. 2012;35(4):573–8.
Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18(7):914–24.
• Takayanagi N, et al. Relationship between daily and in-laboratory gait speed among healthy community-dwelling older adults. Sci Rep. 2019;9(1):3496. An investigation detailing the disassociation between lab-based measures of gait speed and free-living gait speed in older adults. The observations highlight the need for both lab-based and free-living assessments of gait in older adults and suggest this multidimensional approach for other clinical populations.
• Van Ancum JM, et al. Gait speed assessed by a 4-m walk test is not representative of daily-life gait speed in community-dwelling adults. Maturitas. 2019;121:28–34. An investigation highlighting that clinical gait assessments do not directly map to free-living gait speed in community-dwelling older adults. The observations highlight the need for both lab-based and free-living assessments of gait in clinical populations.
Feys P, Gijbels D, Romberg A, Santoyo C, Gebara B, de Noordhout BM, et al. Effect of time of day on walking capacity and self-reported fatigue in persons with multiple sclerosis: a multi-center trial. Mult Scler. 2012;18(3):351–7.
Powell DJH, Liossi C, Schlotz W, Moss-Morris R. Tracking daily fatigue fluctuations in multiple sclerosis: ecological momentary assessment provides unique insights. J Behav Med. 2017;40(5):772–83.
Dickinson MH, et al. How animals move: an integrative view. Science. 2000;288(5463):100–6.
Pau M, Corona F, Pilloni G, Porta M, Coghe G, Cocco E. Texting while walking differently alters gait patterns in people with multiple sclerosis and healthy individuals. Mult Scler Relat Disord. 2018;19:129–33.
Hillel I, Gazit E, Nieuwboer A, Avanzino L, Rochester L, Cereatti A, et al. Is every-day walking in older adults more analogous to dual-task walking or to usual walking? Elucidating the gaps between gait performance in the lab and during 24/7 monitoring. Eur Rev Aging Phys Act. 2019;16:6.
Motl RW, Sandroff BM, Sosnoff JJ. Commercially available accelerometry as an ecologically valid measure of ambulation in individuals with multiple sclerosis. Expert Rev Neurother. 2012;12(9):1079–88.
Sasaki JE, Sandroff B, Bamman M, Motl RW. Motion sensors in multiple sclerosis: narrative review and update of applications. Expert Rev Med Dev. 2017;14(11):891–900.
Uszynski MK, Herring MP, Casey B, Hayes S, Gallagher S, Motl RW, et al. Sources of variability in physical activity among inactive people with multiple sclerosis. Int J Behav Med. 2018;25(2):259–64.
• Supratak A, et al. Remote monitoring in the home validates clinical gait measures for multiple sclerosis. Front Neurol. 2018;9:561. This article demonstrates the ability to accurately measure gait speed in the home environment, providing the ability to track impairment in daily life. A strong association between the T25W gait speed and the max sustained gait speed at home was also observed. However, these results were achieved with subject-specific models, limiting their ecological value.
Shammas L, Zentek T, von Haaren B, Schlesinger S, Hey S, Rashid A. Home-based system for physical activity monitoring in patients with multiple sclerosis (pilot study). Biomed Eng Online. 2014;13:10.
Sosnoff JJ, Socie MJ, Boes MK, Sandroff BM, Motl RW. Does a waist-worn ActiGraph accelerometer quantify community ambulation in persons with multiple sclerosis? J Rehabil Res Dev. 2012;49(9):1405–10.
Motl RW, Weikert M, Suh Y, Sosnoff JJ, Pula J, Soaz C, et al. Accuracy of the actibelt(®) accelerometer for measuring walking speed in a controlled environment among persons with multiple sclerosis. Gait Posture. 2012;35(2):192–6.
Dugan EL, Combs-Miller SA. Physiological complexity of gait is decreased in individuals with chronic stroke. Comput Methods Biomech Biomed Engin. 2019;22(6):658–63.
Del Din S, et al. Free-living gait characteristics in ageing and Parkinson’s disease: impact of environment and ambulatory bout length. J Neuroeng Rehabil. 2016;13(1):46.
Mitchell T, Conradsson D, Paquette C. Gait and trunk kinematics during prolonged turning in Parkinson’s disease with freezing of gait. Parkinsonism Relat Disord. 2019.
Nero H, Benka Wallén M, Franzén E, Ståhle A, Hagströmer M. Accelerometer cut points for physical activity assessment of older adults with Parkinson’s disease. PLoS One. 2015;10(9):e0135899.
Raccagni C, Gaßner H, Eschlboeck S, Boesch S, Krismer F, Seppi K, et al. Sensor-based gait analysis in atypical parkinsonian disorders. Brain Behav. 2018;8(6):e00977.
Moore SA, Hickey A, Lord S, del Din S, Godfrey A, Rochester L. Comprehensive measurement of stroke gait characteristics with a single accelerometer in the laboratory and community: a feasibility, validity and reliability study. J Neuroeng Rehabil. 2017;14(1):130.
Yang S, Zhang JT, Novak AC, Brouwer B, Li Q. Estimation of spatio-temporal parameters for post-stroke hemiparetic gait using inertial sensors. Gait Posture. 2013;37(3):354–8.
Meijer R, Plotnik M, Zwaaftink E, van Lummel RC, Ainsworth E, Martina JD, et al. Markedly impaired bilateral coordination of gait in post-stroke patients: is this deficit distinct from asymmetry? A cohort study. J Neuroeng Rehabil. 2011;8:23.
Taylor-Piliae RE, Mohler MJ, Najafi B, Coull BM. Objective fall risk detection in stroke survivors using wearable sensor technology: a feasibility study. Top Stroke Rehabil. 2016;23(6):393–9.
Sanchez MC, et al. Accelerometric assessment of different dimensions of natural walking during the first year after stroke: recovery of amount, distribution, quality and speed of walking. J Rehabil Med. 2015;47(8):714–21.
• Pau M, et al. Clinical assessment of gait in individuals with multiple sclerosis using wearable inertial sensors: Comparison with patient-based measure. Mult Scler Relat Disord. 2016;10:187–91. This article highlights the potential of wearable accelerometers to quantify pace and rhythm during clinical assessment in PwMS with mild to moderate disability. This eobservation further indicates the clinical utility of sensor based gait assessment.
Pau M, Mandaresu S, Pilloni G, Porta M, Coghe G, Marrosu MG, et al. Smoothness of gait detects early alterations of walking in persons with multiple sclerosis without disability. Gait Posture. 2017;58:307–9.
Storm FA, Nair KPS, Clarke AJ, van der Meulen JM, Mazzà C. Free-living and laboratory gait characteristics in patients with multiple sclerosis. PLoS One. 2018;13(5):e0196463.
Del Din S, Godfrey A, Rochester L. Validation of an accelerometer to quantify a comprehensive battery of gait characteristics in healthy older adults and Parkinson’s disease: toward clinical and at home use. IEEE J Biomed Health Inform. 2016;20(3):838–47.
Ellis RJ, Ng YS, Zhu S, Tan DM, Anderson B, Schlaug G, et al. A validated smartphone-based assessment of gait and gait variability in Parkinson’s disease. PLoS One. 2015;10(10):e0141694.
Schwenk M, Sabbagh M, Lin I, Morgan P, Grewal GS, Mohler J, et al. Sensor-based balance training with motion feedback in people with mild cognitive impairment. J Rehabil Res Dev. 2016;53(6):945–58.
Ijmker T, Lamoth CJ. Gait and cognition: the relationship between gait stability and variability with executive function in persons with and without dementia. Gait Posture. 2012;35(1):126–30.
Brodie MA, Psarakis M, Hoang P. Gyroscopic corrections improve wearable sensor data prior to measuring dynamic sway in the gait of people with multiple sclerosis. Comput Methods Biomech Biomed Engin. 2016;19(12):1339–46.
Hickey A, Gunn E, Alcock L, del Din S, Godfrey A, Rochester L, et al. Validity of a wearable accelerometer to quantify gait in spinocerebellar ataxia type 6. Physiol Meas. 2016;37(11):N105–17.
Urbanek JK, Harezlak J, Glynn NW, Harris T, Crainiceanu C, Zipunnikov V. Stride variability measures derived from wrist- and hip-worn accelerometers. Gait Posture. 2017;52:217–23.
Wang K, Delbaere K, Brodie MAD, Lovell NH, Kark L, Lord SR, et al. Differences between gait on stairs and flat surfaces in relation to fall risk and future falls. IEEE J Biomed Health Inform. 2017;21(6):1479–86.
Grimpampi E, Oesen S, Halper B, Hofmann M, Wessner B, Mazzà C. Reliability of gait variability assessment in older individuals during a six-minute walk test. J Biomech. 2015;48(15):4185–9.
Howcroft J, Kofman J, Lemaire ED, McIlroy WE. Analysis of dual-task elderly gait in fallers and non-fallers using wearable sensors. J Biomech. 2016;49(7):992–1001.
• Psarakis M, et al. Wearable technology reveals gait compensations, unstable walking patterns and fatigue in people with multiple sclerosis. Physiol Meas. 2018;39(7):075004. The first study to develop a method based on accelerometry to objectively quantify asymmetries in limb-specific spatial trajectories during individual gait strides in PwMS and healthy controls.
Sant’Anna A, Salarian A, Wickstrom N. A new measure of movement symmetry in early Parkinson’s disease patients using symbolic processing of inertial sensor data. IEEE Trans Biomed Eng. 2011;58(7):2127–35.
Prajapati SK, Gage WH, Brooks D, Black SE, McIlroy WE. A novel approach to ambulatory monitoring: investigation into the quantity and control of everyday walking in patients with subacute stroke. Neurorehabil Neural Repair. 2011;25(1):6–14.
Lien WC, Cheng YH, Kuan TS, Zheng YL, Hsieh CH, Wang WF. Comparison of gait symmetry between poststroke fallers and nonfallers during level walking using triaxial accelerometry: a STROBE-compliant cross-sectional study. Medicine (Baltimore). 2017;96(9):e5990.
Oyake K, Yamaguchi T, Sugasawa M, Oda C, Tanabe S, Kondo K, et al. Validity of gait asymmetry estimation by using an accelerometer in individuals with hemiparetic stroke. J Phys Ther Sci. 2017;29(2):307–11.
Wang L, Sun Y, Li Q, Liu T. Estimation of step length and gait asymmetry using wearable inertial sensors. IEEE Sens J. 2018;18(9):3844–51.
Zhang W, et al. Gait symmetry assessment with a low back 3D accelerometer in post-stroke patients. Sensors (Basel). 2018;18(10).
Qiu S, Liu L, Wang Z, Li S, Zhao H, Wang J, et al. Body sensor network-based gait quality assessment for clinical decision-support via multi-sensor fusion. IEEE Access. 2019;7:59884–94.
Craig JJ, Bruetsch AP, Lynch SG, Huisinga JM. Altered visual and somatosensory feedback affects gait stability in persons with multiple sclerosis. Hum Mov Sci. 2019;66:355–62.
Craig JJ, et al. The relationship between trunk and foot acceleration variability during walking shows minor changes in persons with multiple sclerosis. Clin Biomech (Bristol, Avon). 2017;49:16–21.
Huisinga JM, Mancini M, St. George RJ, Horak FB. Accelerometry reveals differences in gait variability between patients with multiple sclerosis and healthy controls. Ann Biomed Eng. 2013;41(8):1670–9.
•• Peebles AT, et al. Dynamic balance in persons with multiple sclerosis who have a falls history is altered compared to non-fallers and to healthy controls. J Biomech. 2017; This investigation utilized accelerometry-based assessment of gait and quantified various gait quality parameters including variability and complexity. It was observed that fallers with MS walked with less complexity and increased the variability of step length, stride time, and both anterior-posterior and mediolateral margin of stability compared with non-fallers and healthy controls. This provides evidence of the clinical import of these gait quality metrics.
Afsar O, Tirnakli U, Kurths J. Entropy-based complexity measures for gait data of patients with Parkinson’s disease. Chaos. 2016;26(2):023115.
Warlop T, Detrembleur C, Stoquart G, Lejeune T, Jeanjean A. Gait complexity and regularity are differently modulated by treadmill walking in Parkinson’s disease and healthy population. Front Physiol. 2018;9:68.
Combs-Miller SA, et al. Physiological complexity of gait between regular and non-exercisers with Parkinson’s disease. Clin Biomech (Bristol, Avon). 2019;68:23–8.
Jehu D, Nantel J. Fallers with Parkinson’s disease exhibit restrictive trunk control during walking. Gait Posture. 2018;65:246–50.
Liao F, Wang J, He P. Multi-resolution entropy analysis of gait symmetry in neurological degenerative diseases and amyotrophic lateral sclerosis. Med Eng Phys. 2008;30(3):299–310.
Tamburini P, Mazzoli D, Stagni R. Towards an objective assessment of motor function in sub-acute stroke patients: relationship between clinical rating scales and instrumental gait stability indexes. Gait Posture. 2018;59:58–64.
Kasser SL, Goldstein A, Wood PK, Sibold J. Symptom variability, affect and physical activity in ambulatory persons with multiple sclerosis: understanding patterns and time-bound relationships. Disabil Health J. 2017;10(2):207–13.
Patel S, et al. A wearable computing platform for developing cloud-based machine learning models for health monitoring applications. in 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); 2016.
Gurchiek RD, et al. Remote gait analysis using wearable sensors detects asymmetric gait patterns in patients recovering from ACL reconstruction. in 2019 IEEE International Conference on Body Sensor Networks (BSN); 2019.
Liu Q, Williamson J, Li K, Mohrman W, Lv Q, Dick RP, et al. Gazelle: energy-efficient wearable analysis for running. IEEE Trans Mob Comput. 2017;16(9):2531–44.
Sun R, Moon Y, McGinnis RS, Seagers K, Motl RW, Sheth N, et al. Assessment of postural sway in individuals with multiple sclerosis using a novel wearable inertial sensor. Digital Biomarkers. 2018;2(1):1–10.
Sen-Gupta E, Wright DE, Caccese JW, Wright Jr JA, Jortberg E, Bhatkar V, et al. A pivotal study to validate the performance of a novel wearable sensor and system for biometric monitoring in clinical and remote environments. Digital Biomarkers. 2019;3(1):1–13.
McGinnis RS, et al. Skin mounted accelerometer system for measuring knee range of motion. in 2016 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 2016.
Fasel B, Duc C, Dadashi F, Bardyn F, Savary M, Farine PA, et al. A wrist sensor and algorithm to determine instantaneous walking cadence and speed in daily life walking. Med Biol Eng Comput. 2017;55(10):1773–85.
Soltani A, Dejnabadi H, Savary M, Aminian K. Real-world gait speed estimation using wrist sensor: a personalized approach. IEEE J Biomed Health Inform. 2019:1–1.
M-Sense Research Group. GitHub. https://github.com/search?l=Text&q=M-Sense+Research+Group&type=Code.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mikaela L. Frechette, Brett Meyer, Lindsey Tulipani, and Reed D. Gurchiek each declare no potential conflicts of interest.
Jacob J. Sosnoff reports personal fees from Abbvie, Inc. and grants from Permobile, Inc., National Multiple Sclerosis Society, National Institute of Health, National Institute on Disability, Independent Living, and Rehabilitation Research, outside the submitted work.
Ryan S. McGinnis reports other from Impellia, Inc. (Scientific advisor, consultant) and other from MC10, Inc. (Own stock, consultant), outside the submitted work; in addition, Dr. McGinnis has a patent METHODS AND APPARATUS FOR PROVIDING PERSONALIZED BIOFEEDBACK FOR THE TREATMENT OF PANIC ATTACKS pending (Claims and description include language about providing personalized biofeedback for preventing falls), a patent Method and System for Neuromodulation and Stimulation pending, a patent Method and System for Crowd-Sourced Algorithm Development pending, a patent Automated detection and configuration of wearable devices based on on-body status, location, and/or orientation pending, a patent Athlete Speed Prediction Method Using Data from Attached Inertial Measurement Unit issued, and a patent Apparatus and Methods for Employing Miniature IMU’s for Deducing Forces and Moments on Bodies pending.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Demyelinating Disorders
Rights and permissions
About this article
Cite this article
Frechette, M.L., Meyer, B.M., Tulipani, L.J. et al. Next Steps in Wearable Technology and Community Ambulation in Multiple Sclerosis. Curr Neurol Neurosci Rep 19, 80 (2019). https://doi.org/10.1007/s11910-019-0997-9
Published:
DOI: https://doi.org/10.1007/s11910-019-0997-9