Abstract
Purpose of Review
To systematically review recent findings on the role of immune cell activation in the pathogenesis of hypertension in people living with HIV (PLWH) and compare studies from Sub-Saharan Africa with what is reported in the USA and European literature according to guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Recent Findings
PLWH have an increased risk for development of hypertension and cardiovascular disease. Chronic immune activation contributes to hypertension but the inflammatory milieu that predisposes PLWH to hypertension is poorly understood. We identified 45 relevant studies from 13 unique African countries. The prevalence of hypertension in PLWH on antiretroviral therapy (ART) and the ART-naive PLWH ranged from 6 to 50% and 2 to 41%, respectively. Interleukin (IL)-17A, interferon (IFN)-γ, and higher CD4+ T cell counts were associated with hypertension in ART-treated participants.
Summary
Targeting adaptive immune activation could provide improved care for hypertensive PLWH. Further research is needed to characterize the inflammatory milieu contributing to hypertension in PLWH especially in African populations where the global burden of HIV is the highest.
Similar content being viewed by others
Introduction
The introduction of antiretroviral therapy (ART) has improved survival among people living with HIV (PLWH), but this success is accompanied by a high burden of cardiovascular disease [1,2,3,3]. Hypertension is a major risk factor to cardiovascular disease and its prevalence is higher in PLWH despite viral suppression by ART [4]. The mechanisms contributing to hypertension and cardiovascular disease in PLWH are not fully understood.
A heightened systemic inflammatory process including activation of the innate and adaptive immune systems contributes to the development of hypertension in the general population and in experimental animal studies [5,6,7]. However, it is unknown which innate and adaptive immune factors are most closely linked to hypertension in PLWH. At present, much of our understanding of the role of immune cell activation in the pathogenesis of hypertension comes from experimental animal and human studies in the HIV-negative context, but similar inflammatory biomarkers implicated in these HIV-negative studies have also been associated with hypertension in HIV infection. In this review, we present the current understanding on HIV, hypertension, and immune activation and how these may be related and highlight gaps and the need for further studies. We review studies conducted in Sub-Saharan Africa where the global HIV infection burden is the highest. We also performed a comparative analysis contrasting studies from Sub-Saharan Africa with what is reported in the USA and European literature.
The aim of our current study was to estimate the prevalence of hypertension in PLWH from African studies, identify inflammatory markers or markers of immune activation associated with hypertension in antiretroviral (ART)-treated HIV-positive individuals, and to explore the possible mechanistic interaction between immune activation, hypertension, and HIV in cohorts from Sub-Saharan Africa and contrast with European and US cohorts.
Methods
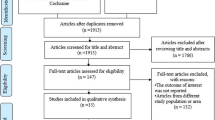
We followed guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [8, 9].
Eligibility Criteria for Studies Included in the Review
We considered studies on HIV-positive human subjects with or without the HIV-negative population as controls. For exposure and outcome variables, we considered HIV infection as the exposure and our outcome measures were hypertension or blood pressure, inflammation, and/or immune activation. Only published articles in peer-reviewed journals were considered. Articles in languages other than English were not considered. We only included studies from Sub-Saharan African, USA, and European HIV-positive populations that reported on hypertension and HIV excluding studies that did not report HIV at all. We also excluded studies reporting opportunistic infections and other coinfections to reduce bias when deducting on the contribution of HIV on hypertension. In case of duplicate publications, the article with more complete data was included. Extracted information focused on study design, population, sample size, country where study was conducted, and details of findings with conclusions. The source of research articles was derived from Pubmed, Medline, google scholar, and google search. Dates of coverage were not specified to filter studies addressing hypertension and inflammation or immune activation in HIV owing to the scarcity of published studies. Other articles were identified from reference lists of related studies from the included study. Search terms that were used in databases employed the use of Boolean operators “AND,” “OR,” and “NOT” to refine our search by combining or limiting terms. The key terms used to search for articles were “hypertension,” “blood pressure,” “immune activation,” “inflammation,” “Africa,” and “HIV.”
Studies were screened based on abstract information that reported HIV or/and inflammation or immune activation and hypertension or blood pressure. A full article was then obtained and screened to ensure eligibility. The PRISMA 2009 Flow Diagrams for article identification, screening, eligibility, and inclusion in Sub-Saharan African and the Western populations are shown in Supplementary Figures 1 and 2 found at the following link: https://figshare.com/s/38ff86137d00153423ac. For data extraction, we used a data collection form that identifies the author, study, population, sample size, methods, findings, and limitations.
Risk of bias was assessed by two reviewers. For the criteria used to assess internal validity of included studies, we made use of the Cochrane Risk of Bias tool, paying attention especially to parts such as completeness of outcome data, selective outcome reporting, reporting bias, and any other bias that may affect the exposure-outcome relationship. For any disagreements between the reviewers over the risk of bias in particular studies, this was resolved by discussion, with involvement of a third review author where necessary.
Data Synthesis
We did not conduct a meta-analysis. We only conducted a systematic thematic review due to the qualitative nature of our study and due to excessive heterogeneity of population, outcome, or methodology. To assist with the result and discussion write-ups, we constructed summary tables and provided a narrative synthesis (thematic or content analysis). This includes investigation of the similarities and the differences between the findings of different studies, as well as exploration of patterns in the data. Reasons for similarities and differences in the findings were also explored systematically. Studies were grouped based on reported parameters. We also considered how the results of studies might be affected by factors such as methodological differences, variable characteristics of the populations studied, or interventions investigated. Conceptual models were used to explore relationships and patterns from study findings and we related the findings to existing concepts from animal models to generate hypotheses and the need for further studies.
Results
Characteristics of the Studies
We performed a systematic review of studies on HIV, hypertension, and immunity from countries in Sub-Saharan Africa, USA, and Europe. For Sub-Saharan Africa studies shown in Table 1, we included 45 studies from 13 countries. Of the 45 studies, 27 were cross-sectional, 15 were prospective, and three were retrospective. Most of the studies (35) reported on both hypertension and HIV. The prevalence of hypertension was highest in the HIV-positive group on ART (ranging from 6.4 to 50.2%) followed by HIV-negative controls (13.7 to 44%). ART-naive patients recorded the lowest prevalence ranging from 2 to 41% by group comparisons. The prevalence differences of groups within studies were highest between ART treated and ART-naive HIV-positive groups (35.7) followed by ART treated and HIV-negative group (18.7) with the least difference in magnitude between HIV negative and ART-naive groups.
When we included USA and European studies, shown in Supplementary Table 1 found at the following link: https://figshare.com/s/38ff86137d00153423ac, the global prevalence of hypertension in PLWH ranged from 4 to 57% (van Ziest et al. 2017) [10]. Hypertension was more prevalent in HIV uninfected (71%) versus HIV infected (57%) in a large longitudinal study by Armah et al. [11]. HIV-infected veterans with HIV-1 RNA ≥ 500 copies/mL or CD4 count < 200 cells/μL had a significantly higher prevalence of elevated IL-6 and D-dimer after adjusting for comorbidities and had significantly higher prevalence of elevated sCD14 compared to uninfected veterans. Manner et al. [12] reported prevalence of 35% hypertension in HIV-infected individuals and the prevalence did not change during the follow-up time (3.4 ± 0.8 years). CD4 T cell count < 50 cells/μL and increased duration of ART were independent predictors of sustained hypertension throughout the study period. Older age, male gender, BMI > 25 kg/m2, and baseline CD4 cell count ≥ 200 cells/μL were also independent predictors of sustained hypertension. Markers of microbial translocation predicted hypertension in HIV-infected individuals. Manner et al. found that both LPS and sCD14 independently predicted subsequent blood pressure levels after adjustment for age and gender [12]. These results suggest that ART may act as a contributing factor to inflammation and the increased prevalence of hypertension in the PLWH.
Higher Levels of IL-17A, IFN-γ, and CD4+ T Cells Are Associated with Hypertension in HIV
We found that among studies reporting on both inflammation, immunity, and hypertension in HIV (Table 2), higher levels of IL-17A, IFN-γ, [13••], and CD4+ T cell count (Peck et al.) [4] were significantly associated with hypertension in ART treated HIV-positive individuals. The cross-section study by Chepchirchir et al. reported that females were more likely to have higher IL-17A levels than males and IL-17A was affected by BMI but not stress levels, ART, World Health Organization (WHO) stage, and CD4+ count [13••]. However, inflammatory cytokines IL-2, IL-6, IL-8, tumor necrosis factor alpha (TNF-α), and anti-inflammatory cytokines IL-4 and IL-10 were not associated with hypertension. The cross-section study by Peck et al. reported higher cases of hypertension among PLWH on ART [28.7% (43/150)] compared to ART-naive participants [5.3% (8/151)]; however, the prevalence was higher in HIV-negative patients [16.3% (25/153)] compared to ART-naive HIV-positive patients. The inflammatory markers, C-reactive protein (CRP), and IL-6 in the prospective study by Fourie et al. where the three participant groups had comparable blood pressures did not differ between HIV positive on ART, ART naive, and HIV-negative groups. In another prospective study by Okello et al., blood pressure increases were reported in the first 6 months of ART initiation then plateaued. Traditional risk factors including older age, male gender, African-American, higher body mass index (BMI), central obesity, previous cardiovascular events, chronic kidney disease, family history of hypertension and cardiovascular disease, diabetes, and dyslipidemia rather than immune activation were associated with incident hypertension in this study. Borkum et al. reported high levels of inflammation and non-dipping blood pressure [14••].
Prevalence of Hypertension Is Higher in ART-Treated PLWH
As shown in Table 3, hypertension prevalence was mostly higher in men than women [15,16,17] and higher among ART treated versus ART naive (28.7% vs 5.3%; 17% vs 2%; 30 vs 21.9% and 38% vs 19%, respectively) [17, 18]. However, one study [22] reported contradictory findings (ART vs ART naive, 12.3 vs 19%). In another study, [17] reported higher prevalence of hypertension in ART treated group (28.7%) compared to the HIV-negative controls (16.3%) but two studies [22, 25] reported the opposite (41% vs 44% and 12.3% vs 13.7%, respectively). Peck et al. reported higher prevalence of hypertension in HIV negative vs ART-naive HIV-positive group (16.3% vs 5.3%) [17]. On the contrary, Ogunmola et al. reported lower prevalence of hypertension in HIV negative vs ART-naive HIV-positive group (13.7% vs 19%, respectively). Association between hypertension and traditional risk factors including specific ART regimens varied between studies.
ART Treatment in PLWH Is Associated with Higher Inflammation
As shown in Table 4, we found that PLWH on ART had higher inflammatory markers including IL-6, CRP, intracellular adhesion molecule 1 (ICAM-1), and vascular adhesion molecule 1 (VCAM-1) compared with HIV-negative individuals (Fourie et al.) [55]. Intermediate monocytes (CD14+16+) increased with viremia in immune-compromised patients and microbial translocation was a major force driving chronic systemic inflammation in HIV-positive individuals on ART.
Discussion
In the current study, we found that the prevalence of hypertension in PLWH in Sub-Saharan African countries ranged from 2.0 to 50.2% with most cases among those receiving ART. Besides traditional risk factors and the effect of ART on blood pressure, IL-17A, IFN-γ, and CD4+ T cells were among the inflammatory parameters associated with hypertension in ART treated PLWH [13••, 56]. The mechanism of interaction between immune activation or inflammation and hypertension in HIV remains elusive and warrants further studies. Our findings and conceptual hypothesis of how immune activation may contribute to hypertension in HIV is shown in Fig. 1. We propose that HIV viral protein and ART interacts with components of the immune system to synergistically induce kidney damage, vascular dysfunction, alterations in sympathetic nervous outflow and lead to hypertension. This process is exacerbated by presence of traditional risk factors exacerbates including obesity, excess dietary salt intake, smoking, and genetic predisposition.
Conceptual schematic of the effect of HIV infection and treatment can activate the immune system leading to hypertension. Viral proteins and/or antiretroviral therapy (ART) activates antigen presenting and T cells which infiltrate the vasculature and the kidneys and release cytokines IL-6, IL-17A, and IFN-γ which promote vascular dysfunction, retention of sodium, and water, leading to hypertension
Prevalence of Hypertension in HIV
The prevalence of hypertension in PLWH varies by population and subgroups even within the same countries. Similar to our findings, Martin-Iguacel et al. and Nguyen et al. reported prevalence ranging from 4 to 54% [57••] and 8.7 to 45.9% among PLWH in low- and middle-income countries [58]. However, in our study, we further segregated prevalence by HIV infection and ART treatment and report magnitude of differences between the groups (Table 1). Higher hypertension prevalence was reported in ART treated PLWH compared with ART-naive participants except in the study by Ogunmola et al. who reported the opposite [22]. This contradictory finding is likely due to differential effects of specific ART regimens and other traditional risk factors differing between study populations. The effect of specific regimens on blood pressure has not yet been well established except for the low to moderate increase attributed to non-nucleoside reverse transcriptase inhibitors (NNRTI’s) and protease inhibitors (PIs) [59, 60]. Prior studies have shown that patients become hypertensive in most cases at least after 2 years of ART and systolic pressure increases further after 5 years of ART [60], and that there is no association between HIV status, ART, and hypertension following short-term follow-up of less than 2 years [22, 61].
Markers of Immune Activation or Inflammation Associated with Hypertension in HIV
Traditional risk factors associated with hypertension in HIV such as older age, male gender, African-American, higher BMI, central obesity, previous CV events, chronic kidney disease, family history of hypertension and CVD, diabetes, and dyslipidemia have been well studied [57••, 58]. It is also well established that HIV infection and exposure to ART (more than 2 years), through metabolic disturbances and endothelial dysfunction, might have an additional role in the development of hypertension in HIV patients [57••, 58]. However, little is known about the contribution of the innate and adaptive immune system in the development or propagation of hypertension in HIV.
In our systematic review, we found that an improved immune status as determined by higher CD4 T cells was associated with higher hypertension prevalence [17]. However, one study be Okello et al. found that CD4 T cell count of less than 100 was associated with incident hypertension [61]. Martin-Iguacel et al. and Nguyen et al. also reported similar findings [57••, 58]. We found that T cell-derived cytokines IL-17A and IFN-γ were associated with hypertension in ART treated PLWH as reported by Chepchirchir et al. [13••]. These cytokines have been reported to contribute to the genesis of hypertension in the HIV-negative general population and experimental animal studies [6]. Further studies are needed to ascertain the contribution of CD4 T cells and their cytokines IL-17 and IFN-γ in concert with existing traditional risk factors on blood pressure elevation in HIV.
Immune Activation, Inflammation, and Hypertension
The role of innate and adaptive immunity including specific cell types and cytokines in the development and maintenance of hypertension has been extensively studied in humans and animal models elsewhere [6, 7, 62•, 63,64,65]. Using multiple experimental animal models, studies have shown that hypertensive stimuli including angiotensin II, aldosterone, endothelin-1, and salt induce activation of immune cells, which infiltrate the vasculature and the kidneys, and release cytokines that induce increased salt and water retention leading to hypertension [6]. This process is mediated in part by increases oxidative stress leading to oxidation of fatty acids and formation of isolevuglandins (IsoLGs) in antigen-presenting cells. IsoLGs activate these cells to produce pro-inflammatory cytokines IL-6, IL-1β, and IL-23, express costimulatory proteins CD80 and CD86, and activate T cells to produce pro-hypertensive cytokines IFN-γ and IL-17A [7]. In humans, plasma isoprostanes, which are produced in concert with IsoLGs, are elevated in hypertension and markedly elevated in patients with resistant hypertension, and IsoLGs are markedly elevated in circulating monocytes of hypertensive patients [7]. IL-17A and IFN-γ have been implicated in the genesis and maintenance of hypertension due in part to their direct effect in causing endothelial dysfunction and renal damage [6, 66]. Thus, similar immuno-pathophysiological mechanisms underlying hypertension in the general population may also contribute to elevated blood pressure in PLWH.
Potential Mechanisms Leading to Inflammation in HIV
The pathophysiology of HIV-related hypertension seems to emerge from three factors: HIV-related inflammation, HIV-related proteins, and genetic predisposition [59]. It is believed that the HIV viral proteins (negative factor (Nef), transcription proteins (Tat) and glycoprotein 120 (gp-120)) induce hypertension through vascular oxidative stress, smooth myocyte proliferation and migration, and endothelial dysfunction especially in patients with high HIV viral load [59]. Tat, a transactivator protein for HIV replication, is known to be secreted extracellularly by infected cells and has been shown to activate endothelial cells by increasing expression of endothelial-leukocyte adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), and E-selectin which induce initial binding of leukocytes to the blood vessel wall [67]. The levels of soluble ICAM-1 concentration correlate with HIV disease as well as reduction in CD4 count. Tat also induces IL-6 production which increases endothelial permeability [67]. Tat can also suppress the bone morphogenic protein receptor 2 (BMPR-2) responsible for regulating endothelial cell proliferation and survival. This results in increased vascular smooth muscle proliferation and activation of endothelial cells leading to pulmonary arterial hypertension (PAH) [68]. In HIV-positive patients, Tat has been shown to increase the transcription of IL-17 and secretion by T cells causing a pro-inflammatory milieu and has been associated with a devastating immune reconstitution inflammatory syndrome (IRIS) in the brain [69]. The HIV Gp120 is found on the surface of the HIV envelope and can also be found in circulation from viral turn over [70]. Gp120 stimulates monocytes and macrophages to release pro-inflammatory cytokines, promotes an increase in markers of apoptosis, and stimulates the secretion of endothelin-1, a potent vasoconstrictor [68]. It induces endothelial apoptosis by interacting with CXCR4 also expressed on endothelial cells [70]. Gp120 and TNF-α synergistically decrease eNOS and NO in human coronary artery endothelial cells [70].
DCs, the most potent antigen-presenting cells of the innate immune system, have been shown to interact with components of HIV-1 both intrinsically (following fusion of cellular and viral membrane) and extrinsically (prior to being infected) through pathogen recognition receptors (PRRs) resulting in activation of the adaptive immune system [71]. Through their CD28/B7 ligands CD80 and CD86 (also expressed on monocytes and B cells), DCs provide a costimulatory signal necessary for T cell activation and survival. In hypertension, there is an increase in B7 ligand expression leading to T cell activation [5, 72]. An important element in the activation of T cells by DCs and other cells in hypertension is antigen presentation. It is unclear what antigens are presented to T cells in HIV and it is not known if IsoLG-adducted peptides might play a role in hypertension associated with HIV.
Monocyte activation has an important role in HIV-infected persons on ART. Monocytes are chronically activated during HIV infection and it is now evident that inflammatory mediators produced by monocytes (especially IL-6), independent of T cell activation, also predict serious non-AIDS events (SNAEs) in virologically suppressed HIV-infected persons treated with ART [73]. IL-6 production was higher in monocytes than other cells and was associated with increased odds of SNAE and mortality but not the percentage of activated CD4 and CD8 T cells (those expressing CD38 or CD38 and HLA-DR) [73]. Infected monocytes, especially intermediate monocytes expressing CD14+ and CD16+, produce more pro-inflammatory cytokines as compared to their counterpart. They adhere to endothelial cells and transmigrate into the sub endothelial area where their pro-inflammatory activity is increased. It is evident that in HIV, monocytes and macrophages have a reduced phagocytic activity and they age prematurely [70]. Monocytes/macrophages have been implicated in the pathogenesis of hypertension in the general population and experimental animal models [5].
Several mechanisms of immune cell activation have been reported in HIV. First, there is direct binding of the HIV envelope protein gp120/160 to CD4 and/or C-C chemokine receptor type 5 (CCR5) which down-modulates the expression of CD3+ T cell receptor in infected cells resulting in cell death; second, there is an interaction between HIV viral particles and plasmacytoid dendritic cells (DCs) through Toll like receptor (TLR) stimulation which activates CD8+ cytotoxic cells; third, there is microbial translocation from a leaky gut into the circulation leading to a generalized systemic inflammatory process [74]. Also important is the dysfunction of T regulatory cells and immune-senescence resulting in an uncontrolled over activation of immune cells in HIV [74]. The resultant low-grade chronic inflammation which persists even after initiation of ART is associated with hypertension and cardiovascular disease [75, 76].
IL-6 production by monocytes and macrophages is increased following HIV infection and is a valuable prognostic marker for disease progression [77, 78]. Soluble CD14 (sCD14) produced from monocytes and macrophages is also elevated in HIV-infected persons regardless of treatment status and is an independent predictor of mortality [73]. Anzinger et al. reported that increased microbial translocation from the gut resulting from depletion of CD4+ T cells in acute HIV infection results in monocyte activation and higher sCD14 [73]. The expression of programmed death-1 (PD-1), a member of the B7:28 inhibitory molecules, is rapidly increased on CD4+ and CD8+ T cells, B cells, natural killer cells, and monocytes as they interact with PD-L1, its ligand on antigen-presenting cells such that engagement on virus-infected cells leads to impaired generation of effector T cell responses [74]. Other markers which have been associated with immune activation in HIV include increased expression of CD28−, CD57+ and reduced expression of CD127 on CD4+ and CD8+ T cells [79, 80].
In our analysis, we found HIV infection alone is associated with an inflammatory milieu involving higher levels of IL-6, CRP, VCAM-1 ICAM-1, and intermediate monocytes (CD14+16+) among studies conducted in Sub-Saharan African cohorts [17, 55]. There is a generalized systemic immune activation following HIV infection which subsides but still persists at low-grade or subclinical following initiation of ART involving activation of both CD4+ and CD8+ T cells expressing high levels of CD38 [74]. Other T cell activation markers such as human leukocyte antigen–antigen D related (HLA-DR) as well as increases in pro-inflammatory cytokines tumor necrosis factor alpha (TNF-α), interleukin 6 (IL-6), and interleukin 1 beta (IL-1β) have been reported in PLWH in the western countries [74]. Increased expression of CD38 alone or in concert with HLA-DR+ in T cells is a marker of disease progression and mortality in some cases correlating directly with HIV viral load and indirectly with CD4+ count [74]. This continuous immune activation and inflammation has been proposed to contribute to endothelial dysfunction, hypertension, and cardiovascular disease [81].
Limitations, Conclusion, and Future Perspectives
Almost all studies except one [13••] were not designed to compare blood pressure or hypertension and inflammation in PLWH as the primary outcomes. There is need for additional prospective and mechanistic studies to establish the relationship between inflammation and hypertension in HIV infection, and ART. Most studies addressing the mechanistic role of inflammation in the genesis and progression of hypertension have been conducted in murine models and humans in the HIV-negative context. The inflammatory milieu in HIV infection is obviously complex and very different from the general population and further studies are needed to determine the specific contribution of the various attributes in HIV including the viral proteins and ART on inducing inflammation associated with hypertension.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Currier JS, Taylor A, Boyd F, Dezii CM, Kawabata H, Burtcel B, et al. Coronary heart disease in HIV-infected individuals. J Acquir Immune Defic Syndr. 2003;33:506–12.
Triant VA, Lee H, Hadigan C, Grinspoon SK. Increased acute myocardial infarction rates and cardiovascular risk factors among patients with human immunodeficiency virus disease. J Clin Endocrinol Metab. 2007;92:2506–12.
Cruse B, Cysique LA, Markus R, Brew BJ. Cerebrovascular disease in HIV-infected individuals in the era of highly active antiretroviral therapy. J Neuro-Oncol. 2012;18:264–76.
Freiberg MS, Chang CC, Kuller LH, Skanderson M, Lowy E, Kraemer KL, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173:614–22.
Mian MOR, Paradis P, Schiffrin EL. Innate immunity in hypertension. Curr Hypertens Rep. 2014;16:413.
McMaster WG, Kirabo A, Madhur MS, Harrison DG. Inflammation, immunity, and hypertensive end-organ damage. Circ Res. 2015;116:1022–33.
Kirabo A, Fontana V, de Faria AP, Loperena R, Galindo CL, Wu J, et al. DC isoketal-modified proteins activate T cells and promote hypertension. J Clin Invest. 2014;124:4642–56.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
van Zoest RA, van den Born BH, Reiss P. Hypertension in people living with HIV. Curr Opin HIV AIDS. 2017;12:513–22.
Armah KA, McGinnis K, Baker J, Gibert C, Butt AA, Bryant KJ, et al. HIV status, burden of comorbid disease, and biomarkers of inflammation, altered coagulation, and monocyte activation. Clin Infect Dis. 2012;55:126–36.
Manner IW, Baekken M, Oektedalen O, Os I. Hypertension and antihypertensive treatment in HIV-infected individuals. A longitudinal cohort study. Blood Press. 2012;21:311–9.
•• Chepchirchir A, Nyagol J, Jaoko W. Cytokine expression and hypertension comorbidity in HIV/AIDS patients at Kenyatta National Hospital HIV Care Centre, Nairobi, Kenya. Int J Cardiovasc Res 2018;7:2 This recent manuscript found that IL-17 and IFN-γ are associated with hypertension in HIV.
•• Peck RN, Shedafa R, Kalluvya S, Downs JA, Todd J, Suthanthiran M, et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: a cross-sectional study. BMC Med. 2014;12:125 This work found that hypertension and kidney disease were associated with HIV and ART. The study also found that CD4 T cell counts are associated with hypertension in HIV.
Fourie CMT, Schutte AE, Smith W, Kruger A, van Rooyen JM. Endothelial activation and cardiometabolic profiles of treated and never-treated HIV infected Africans. Atherosclerosis. 2015;240:154–60.
Okello S, Asiimwe SB, Kanyesigye M, Muyindike WR, Boum Y, Mwebesa BB, et al. D-dimer levels and traditional risk factors are associated with incident hypertension among HIV-infected individuals initiating antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2016;73:4:396–402
Borkum MS, Heckmann JM, Manning K, Dave JA, Levitt NS, Rayner BL, et al. High prevalence of “non-dipping” blood pressure and vascular stiffness in HIV-infected South Africans on antiretrovirals. PLoS One. 2017;12:9: e0185003.
Bloomfield GS, Hogan JW, Keter A, Sang E, Carter EJ, Velazquez EJ, et al. Hypertension and obesity as cardiovascular risk factors among HIV seropositive patients in Western Kenya. PLoS One. 2011;6:7:e22288
Julius H, Basu D, Ricci E, Wing J, Basu JK, Pocaterra D, et al. The burden of metabolic diseases amongst HIV positive patients on HAART attending The Johannesburg Hospital. Curr HIV Res. 2011;9:247–52.
Diouf A, Cournil A, Ba-Fall K, Ngom-Guèye NF, Eymard-Duvernay S, Ndiaye I, et al. Diabetes and hypertension among patients receiving antiretroviral treatment since 1998 in Senegal: prevalence and associated factors. Isrn Aids. 2012;2012:621565.
Ngatchou W, Lemogoum D, Ndobo P, Yiagnigni E, Tiogou E, Nga E, et al. Effects of antiretroviral therapy on arterial stiffness in Cameroonian HIV-infected patients. Blood Press Monit. 2013;18:247–51.
Parikh SM, Obuku EA, Walker SA, Semeere AS, Auerbach BJ, Hakim JG, et al. Clinical differences between younger and older adults with HIV/AIDS starting antiretroviral therapy in Uganda and Zimbabwe: a secondary analysis of the DART trial. PloS One. 2013;8:e76158.
Ekali LG, Johnstone LK, Echouffo-Tcheugui JB, Kouanfack C, Dehayem MY, Fezeu L, et al. Fasting blood glucose and insulin sensitivity are unaffected by HAART duration in Cameroonians receiving first-line antiretroviral treatment. Diabetes Metab. 2013;39:71–7.
Muhammad S, Sani MU, Okeahialam BN. Cardiovascular disease risk factors among HIV-infected Nigerians receiving highly active antiretroviral therapy. Niger Med J 2013;54:185–90
Mateen FJ, Kanters S, Kalyesubula R, Mukasa B, Kawuma E, Kengne AP, et al. Hypertension prevalence and Framingham risk score stratification in a large HIV-positive cohort in Uganda. J Hypertens. 2013;31:1372–8 discussion 1378.
Botha S, Fourie CMT, van Rooyen JM, Kruger A, Schutte AE. Cardiometabolic changes in treated versus never treated HIV-infected black South Africans: the PURE study. Heart Lung Circ. 2014;23:119–26.
Ogunmola OJ, Oladosu OY, Olamoyegun AM. Association of hypertension and obesity with HIV and antiretroviral therapy in a rural tertiary health center in Nigeria: a cross-sectional cohort study. Vasc Health Risk Manag. 2014;10:129–37.
Shaffer D, Hughes MD, Sawe F, Bao Y, Moses A, Hogg E, et al. Cardiovascular disease risk factors in HIV-infected women after initiation of lopinavir/ritonavir- and nevirapine-based antiretroviral therapy in Sub-Saharan Africa: A5208 (OCTANE). J Acquir Immune Defic Syndr 1999. 2014;66:155–63.
Sawadogo A, Sanou S, Hema A, Kamboule BE, Kabore NF, Sore I, et al. Metabolic syndrome and cardiovascular risk patients under antiretrovirals in a day hospital at Bobo-Dioulasso (Burkina Faso). Bull Soc Pathol Exot 1990. 2014;107:151–8.
Kagaruki GB, Mayige MT, Ngadaya ES, Kimaro GD, Kalinga AK, Kilale AM, et al. Magnitude and risk factors of non-communicable diseases among people living with HIV in Tanzania: a cross sectional study from Mbeya and Dar es Salaam regions. BMC Public Health. 2014;14:904.
Abrahams Z, Dave JA, Maartens G, Levitt NS. Changes in blood pressure, glucose levels, insulin secretion and anthropometry after long term exposure to antiretroviral therapy in South African women. AIDS Res Ther. 2015;12:24.
Okello S, Kanyesigye M, Muyindike WR, Annex BH, Hunt PW, Haneuse S, et al. Incidence and predictors of hypertension in adults with HIV initiating antiretroviral therapy in southwestern Uganda. J Hypertens. 2015;33:2039–45.
Dimala CA, Atashili J, Mbuagbaw JC, Wilfred A, Monekosso GL. Prevalence of hypertension in HIV/AIDS patients on Highly Active Antiretroviral Therapy (HAART) compared with HAART-naïve patients at the Limbe Regional Hospital, Cameroon. PloS One. 2016;11:e0148100.
Feigl AB, Bloom DE, Danaei G, Pillay D, Salomon JA, Tanser F, et al. The effect of HIV and the modifying effect of Anti-Retroviral Therapy (ART) on Body Mass Index (BMI) and Blood Pressure Levels in Rural South Africa. PloS One. 2016;11:e0158264.
Kalyesubula R, Kayongo A, Semitala FC, Muhanguzi A, Katantazi N, Ayers D, et al. Trends and level of control of hypertension among adults attending an ambulatory HIV clinic in Kampala, Uganda: a retrospective study. BMJ Glob Health. 2016;1:e000055.
Kwarisiima D, Balzer L, Heller D, Kotwani P, Chamie G, Clark T, et al. Population-based assessment of hypertension epidemiology and risk factors among HIV-Positive and General Populations in Rural Uganda. PloS One. 2016;11:e0156309.
Njelekela M, Muhihi A, Aveika A, Spiegelman D, Hawkins C, Armstrong C, et al. Prevalence of hypertension and its associated risk factors among 34,111 HAART Naïve HIV-infected adults in Dar es Salaam, Tanzania. Int J Hypertens. 2016;2016:5958382.
Osegbe ID, Soriyan OO, Ogbenna AA, Okpara HC, Azinge EC. Risk factors and assessment for cardiovascular disease among HIV-positive patients attending a Nigerian tertiary hospital. Pan Afr Med J. 2016;23:206.
Divala OH, Amberbir A, Ismail Z, Beyene T, Garone D, Pfaff C, et al. The burden of hypertension, diabetes mellitus, and cardiovascular risk factors among adult Malawians in HIV care: consequences for integrated services. BMC Public Health. 2016;16:1243.
Magodoro IM, Esterhuizen TM, Chivese T. A cross-sectional, facility based study of comorbid non-communicable diseases among adults living with HIV infection in Zimbabwe. BMC Res Notes. 2016;9:379.
Nduka CU, Stranges S, Bloomfield GS, Kimani PK, Achinge G, Malu AO, et al. A plausible causal link between antiretroviral therapy and increased blood pressure in a sub-Saharan African setting: a propensity score-matched analysis. Int J Cardiol. 2016;220:400–7.
Bauer S, Wa Mwanza M, Chilengi R, Holmes CB, Zyambo Z, Furrer H, et al. Awareness and management of elevated blood pressure among human immunodeficiency virus-infected adults receiving antiretroviral therapy in urban Zambia: a call to action. Glob Health Action. 2017;10:1359923.
Kazooba P, Kasamba I, Mayanja BN, Lutaakome J, Namakoola I, Salome T, et al. Cardiometabolic risk among HIVPOSITIVE Ugandan adults: prevalence, predictors and effect of long-term antiretroviral therapy. Pan Afr Med J. 2017;27:40.
Mayanja BN, Kasamba I, Levin J, Namakoola I, Kazooba P, Were J, et al. COHORT PROFILE: The Complications of Long-Term Antiretroviral Therapy study in Uganda (CoLTART), a prospective clinical cohort. AIDS Res Ther. 2017;14:26.
Okpa HO, Bisong EM, Enang OE, Monjok E, Essien EJ. Predictors of hypertension in an urban HIV-infected population at the University of Calabar Teaching Hospital, Calabar, Nigeria. HIVAIDS Auckl NZ. 2017;9:19–24.
Rodríguez-Arbolí E, Mwamelo K, Kalinjuma AV, Furrer H, Hatz C, Tanner M, et al. Incidence and risk factors for hypertension among HIV patients in rural Tanzania - a prospective cohort study. PloS One. 2017;12:e0172089.
Isa SE, Kang’ombe AR, Simji GS, Shehu NY, Oche AO, Idoko JA, et al. Hypertension in treated and untreated patients with HIV: a study from 2011 to 2013 at the Jos University Teaching Hospital, Nigeria. Trans R Soc Trop Med Hyg. 2017;111:172–7.
Magande PN, Chirundu D, Gombe NT, Mungati M, Tshimanga M. Determinants of uncontrolled hypertension among clients on anti-retroviral therapy in Kadoma City, Zimbabwe, 2016. Clin Hypertens [Internet]. 2017;23. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5496338/.
Okello S, Ueda P, Kanyesigye M, Byaruhanga E, Kiyimba A, Amanyire G, et al. Association between HIV and blood pressure in adults and role of body weight as a mediator: Cross-sectional study in Uganda. J Clin Hypertens Greenwich Conn. 2017;19:1181–91.
Mukeba-Tshialala D, Nachega JB, Mutombo-Tshingwali M, Arendt V, Gilson G, Moutschen M. Obesity, high blood pressure, hypercholesterolaemia, and untreated diabetes in HIV-infected and HIV-uninfected adults in Mbuji-Mayi (Democratic republic of congo). Bull Soc Pathol Exot 1990. 2017;110:301–9.
Mathabire Rücker SC, Tayea A, Bitilinyu-Bangoh J, Bermúdez-Aza EH, Salumu L, Quiles IA, et al. High rates of hypertension, diabetes, elevated low-density lipoprotein cholesterol, and cardiovascular disease risk factors in HIVinfected patients in Malawi. AIDS Lond Engl. 2018;32:253–60.
Fourie C, van Rooyen J, Pieters M, Conradie K, Hoekstra T, Schutte A. Is HIV-1 infection associated with endothelial dysfunction in a population of African ancestry in South Africa? Cardiovasc J Afr. 2011;22:134–40.
Cassol E, Malfeld S, Mahasha P, van der Merwe S, Cassol S, Seebregts C, et al. Persistent microbial translocation and immune activation in HIV-1-infected South Africans receiving combination antiretroviral therapy. J Infect Dis. 2010;202:723–33.
Canipe A, Chidumayo T, Blevins M, Bestawros M, Bala J, Kelly P, et al. A 12 week longitudinal study of microbial translocation and systemic inflammation in undernourished HIV-infected Zambians initiating antiretroviral therapy. BMC Infect Dis. 2014;14:521.
Siedner MJ, Kim J-H, Nakku RS, Bibangambah P, Hemphill L, Triant VA, et al. Persistent immune activation and carotid atherosclerosis in HIV-Infected Ugandans Receiving Antiretroviral Therapy. J Infect Dis. 2016;213:370–8.
Peck R, Mghamba J, Vanobberghen F, Kavishe B, Rugarabamu V, Smeeth L, et al. Preparedness of Tanzanian health facilities for outpatient primary care of hypertension and diabetes: a cross-sectional survey. Lancet Glob Health. 2014;2:e285–92.
•• Martin-Iguacel R, Negredo E, Peck R, Friis-Møller N. Hypertension is a key feature of the metabolic syndrome in subjects aging with HIV. Curr Hypertens Rep. 2016;18:46 This review highlighed how HIV infection contributest to metabolic syndrome and emphazised the importance of cardiovascuscular risk screaning among people aging with HIV.
Nguyen KA, Peer N, Mills EJ, Kengne AP. Burden, determinants, and pharmacological management of hypertension in HIV-positive patients and populations: a systematic narrative review. AIDS Rev. 2015;17:83–95.
Bigna JJR, Nansseu JRN, Um LN, Noumegni SRN, Simé PSD, Aminde LN, et al. Prevalence and incidence of pulmonary hypertension among HIV-infected people in Africa: a systematic review and meta-analysis. BMJ Open. 2016;6:e011921.
Calò LA, Caielli P, Maiolino G, Rossi G. Arterial hypertension and cardiovascular risk in HIV-infected patients. J Cardiovas Med. 2013;14:553–8.
Okello S, Asiimwe SB, Kanyesigye M, Muyindike WR, Boum Y, Mwebesa BB, et al. D-dimer levels and traditional risk factors are associated with incident hypertension among HIV-infected individuals initiating antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2016;73:4:396–402.
• Caillon A, Schiffrin EL. Role of inflammation and immunity in hypertension: recent epidemiological, laboratory, and clinical evidence. Curr Hypertens Rep. 2016;18:21 This review comprehensively outlines the recent findings on immunity and its links to hypertension.
Dinh QN, Drummond GR, Sobey CG, Chrissobolis S. Roles of inflammation, oxidative stress, and vascular dysfunction in hypertension. Biomed Res Int. 2014;2014:1–11.
Nguyen H, Chiasson VL, Chatterjee P, Kopriva SE, Young KJ, Mitchell BM. Interleukin-17 causes rho-kinase-mediated endothelial dysfunction and hypertension. Cardiovasc Res. 2013;97:696–704.
Wade B, Abais-Battad JM, Mattson DL. Role of immune cells in salt-sensitive hypertension and renal injury. Curr Opin Nephrol Hypertens. 2016;25:22–7.
Schiffrin EL. Immune mechanisms in hypertension and vascular injury. Clin Sci (London, England: 1979). 2014;126:267–74.
Hofman FM, Wright AD, Dohadwala MM, Wong-Staal F, Walker SM. Exogenous tat protein activates human endothelial cells. [see comments]. Blood. 1993;82:2774–80.
Correale M, Palmiotti GA, Lo Storto MM, Montrone D, Foschino Barbaro MP, Di Biase M, et al. HIV-associated pulmonary arterial hypertension: from bedside to the future. Eur J Clin Investig. 2015;45:515–28.
Johnson TP, Patel K, Johnson KR, Maric D, Calabresi PA, Hasbun R, et al. Induction of IL-17 and nonclassical T-cell activation by HIV-Tat protein. Proc Natl Acad Sci U S A. 2013;110:13588–93.
Shahbaz S, Manicardi M, Guaraldi G, Raggi P. Cardiovascular disease in human immunodeficiency virus infected patients: a true or perceived risk? World J Cardiol. 2015;7:633–44.
Iwasaki A, Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science (New York, NY). 2010;327:291–5.
Vinh A, Chen W, Blinder Y, Weiss D, Taylor WR, Goronzy JJ, et al. Inhibition and genetic ablation of the B7/CD28 T-cell costimulation axis prevents experimental hypertension. Circulation. 2010;122:2529–37.
Anzinger JJ, Butterfield TR, Angelovich TA, Crowe SM, Palmer CS. Monocytes as regulators of inflammation and HIV-related comorbidities during cART. J Immunol Res. 2014;2014:1–11.
Mohan T, Bhatnagar S, Gupta DL, Rao DN. Current understanding of HIV-1 and T-cell adaptive immunity: progress to date. Microb Pathog. 2014;73:60–9.
D'Abramo A, Zingaropoli MA, Oliva A, D'Agostino C, Al Moghazi S, De Luca G, et al. Immune activation, immunosenescence, and osteoprotegerin as markers of endothelial dysfunction in subclinical HIV-associated atherosclerosis. Mediat Inflamm. 2014;2014:192594.
Tsoukas C. Immunosenescence and aging in HIV. Curr Opin HIV AIDS. 2014;9:398–404.
Borges ÁH, O'Connor JL, Phillips AN, Rönsholt FF, Pett S, Vjecha MJ, et al. Factors associated with plasma IL-6 levels during HIV infection. J Infect Dis. 2015;212:585–95.
Nixon DE, Landay AL. Biomarkers of immune dysfunction in HIV. Curr Opin HIV AIDS. 2010;5:498–503.
Aberg JA. Aging, inflammation, and HIV infection. Top Antivir Med. 2012;20:3:101–5
Mojumdar K, Vajpayee M, Chauhan NK, Singh A, Singh R, Kurapati S. Loss of CD127 & increased immunosenescence of T cell subsets in HIV infected individuals. Indian J Med Res. 2011;134:972–81.
Nemeth CL, Bekhbat M, Neigh GN. Neural effects of inflammation, cardiovascular disease, and HIV: parallel, perpendicular, or progressive? Neuroscience. 2015;302:165–73.
Acknowledgments
Graphics were produced using the online ePath3D toll (Protein Lounge, Inc.).
Funding
This work was supported by the Fogarty International Center of the National Institutes of Health under the Award Number D43 TW009744, NIAID Grant K23 AI100700, the NIH-funded Vanderbilt Clinical and Translational Science award from NCRR/NIH Grant UL1 RR024975, the NIH-funded Tennessee Center for AIDS Research Grant P30 AI110527, and National Institutes of Health grant K01HL130497. This work was also supported by NIAID grant K23 100700, the NIH-funded Vanderbilt Clinical and Translational Science award from NCRR/NIH grant UL1 RR024975, and the NIH-funded Tennessee Center for AIDS Research grant P30 AI110527. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SKM and AK conceived the study. SKM, AK conducted the data collection. SKM, BMH, SN, DH, JRK, GK, WM, SM, and AK conducted article reviews and led the writing of the manuscript. All authors read, provided feedback, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Inflammation and Cardiovascular Diseases
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Masenga, S.K., Hamooya, B.M., Nzala, S. et al. Patho-immune Mechanisms of Hypertension in HIV: a Systematic and Thematic Review. Curr Hypertens Rep 21, 56 (2019). https://doi.org/10.1007/s11906-019-0956-5
Published:
DOI: https://doi.org/10.1007/s11906-019-0956-5