Abstract
Purpose of Review
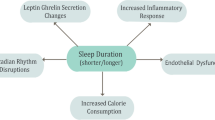
Night-to-night variability in sleep patterns leads to circadian disruption and, consequently, could increase cardiometabolic risk. The purpose of this review is to summarize findings from studies published between 2015 and 2020 examining various measures of night-to-night variability in sleep in relation to metabolic syndrome (MetS), type 2 diabetes (T2D), and their risk factors. We illustrate a potential causal pathway between irregular sleep patterns and T2D, highlighting knowledge gaps along the way.
Recent Findings
Across different measures of sleep variability, irregular sleep patterns were associated with poorer cardiometabolic outcomes. Higher standard deviations (SD) across nights of sleep duration and onset or midpoint of sleep were associated with increased odds of having MetS and clusters of metabolic abnormalities as well as greater adiposity and poorer glycemic control. Conversely, greater regularity of rest-activity patterns related to lower risk for T2D. Social jetlag was associated with glycemic dysregulation, adiposity, T2D, and MetS. These associations are often observed in both metabolically healthy and unhealthy individuals; both higher SD of sleep duration and social jetlag relate to poorer glucose regulation in individuals with diabetes.
Summary
There is consistent evidence of associations of sleep variability with increased risk for adiposity, glucose dysregulation, T2D, and MetS. Although experimental evidence is needed to determine causation, there is support to recommend stabilizing sleep patterns for cardiometabolic risk prevention.

Similar content being viewed by others
References
Linton SJ, Kecklund G, Franklin KA, Leissner LC, Sivertsen B, Lindberg E, et al. The effect of the work environment on future sleep disturbances: a systematic review. Sleep Med Rev. 2015 Oct 1;23:10–9.
Division of Sleep Medicine H. External factors that influence sleep | Healthy Sleep. [cited 2020 Feb 17]. Available from: http://healthysleep.med.harvard.edu/healthy/science/how/external-factors.
Dillon HR, Lichstein KL, Dautovich ND, Taylor DJ, Riedel BW, Bush AJ. Variability in self-reported normal sleep across the adult age span. J Gerontol Ser B. 2015 [cited 2020 Feb 22];70(1):46–56. Available from: https://academic.oup.com/psychsocgerontology/article/68/4/540/569189.
Tworoger SS, Davis S, Vitiello MV, Lentz MJ, McTiernan A. Factors associated with objective (actigraphic) and subjective sleep quality in young adult women. J Psychosom Res. 2005;59(1):11–9.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;497–509.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C. Social jetlag and obesity. Curr Biol. 2012;22(10):939–43.
Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: the multi-ethnic study of atherosclerosis. J Am Coll Cardiol. 2020;75(9):991–9.
Kecklund G, Axelsson J. Health consequences of shift work and insufficient sleep. Vol. 355, BMJ (Online). BMJ Publishing Group; 2016.
Wang F, Zhang L, Zhang Y, Zhang B, He Y, Xie S, et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obes Rev. 2014;15(9):709–20.
Phillips AJK, Clerx WM, O’Brien CS, Sano A, Barger LK, Picard RW, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017;1:7(1).
Huang T, Redline S. Cross-sectional and prospective associations of actigraphy-assessed sleep regularity with metabolic abnormalities: the multi-ethnic study of atherosclerosis. Diabetes Care. 2019 [cited 2019 Jun 25];dc190596. Available from: http://www.ncbi.nlm.nih.gov/pubmed/31167888.
Ogilvie RP, Redline S, Bertoni AG, Chen X, Ouyang P, Szklo M, et al. Actigraphy measured sleep indices and adiposity: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2016 Sep 1 [cited 2020 Feb 17];39(9):1701–8. Available from: https://academic.oup.com/sleep/article/39/9/1701/2708329.
Kim M, Sasai H, Kojima N, Kim H. Objectively measured night-to-night sleep variations are associated with body composition in very elderly women. J Sleep Res. 2015 [cited 2020 Feb 17];24(6):639–47. Available from: http://doi.wiley.com/10.1111/jsr.12326
Rosique-Esteban N, Papandreou C, Romaguera D, Warnberg J, Corella D, Martínez-González MÁ, et al. Cross-sectional associations of objectively-measured sleep characteristics with obesity and type 2 diabetes in the PREDIMED-Plus trial. Sleep. 2018 [cited 2020 Feb 17];41(12). Available from: https://academic.oup.com/sleep/article/doi/10.1093/sleep/zsy190/5115226.
Baron KG, Reid KJ, Malkani RG, Kang J, Zee PC. Sleep variability among older adults with insomnia: associations with sleep quality and cardiometabolic disease risk. Behav Sleep Med. 2017;15(2):144–57.
Brouwer A, Van Raalte DH, Rutters F, Elders PJM, Snoek FJ, Beekman ATF, et al. Sleep and HbA1c in patients with type 2 diabetes: which sleep characteristics matter most? Diabetes Care. 2020;43(1):235–43.
Whitaker KM, Lutsey PL, Ogilvie RP, Pankow JS, Bertoni A, Michos ED, et al. Associations between polysomnography and actigraphy-based sleep indices and glycemic control among those with and without type 2 diabetes: the multi-ethnic study of atherosclerosis. SLEEPJ [Internet]. 2018 [cited 2020 Apr 13];1–10. Available from: https://academic.oup.com/sleep/article-abstract/41/11/zsy172/5089925.
Chontong S, Saetung S, Reutrakul S. Higher sleep variability is associated with poorer glycaemic control in patients with type 1 diabetes. J Sleep Res. 2016 [cited 2020 Feb 16];25(4):438–44. Available from: http://doi.wiley.com/10.1111/jsr.12393
Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000 Aug 15;106(4):473–81.
Leblanc ES, Smith NX, Nichols GA, Allison MJ, Clarke GN. Insomnia is associated with an increased risk of type 2 diabetes in the clinical setting. BMJ Open Diab Res Care. 2018 [cited 2020 Apr 13];6:604. Available from: http://drc.bmj.com/
Javaheri S, Redline S. Insomnia and risk of cardiovascular disease. Chest. 2017;152(2):435–44.
Sánchez-Ortuño MM, Carney CE, Edinger JD, Wyatt JK, Harris A. Moving beyond average values: assessing the night-to-night instability of sleep and arousal in DSM-IV-TR insomnia subtypes. Sleep. 2011;34(4):531–9.
Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014;383(9911):69–82.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Validation of the sleep regularity index in older adults and associations with cardiometabolic risk. Sci Rep. 2018;1:8(1).
Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. 2015;100(12):4612–20.
Islam Z, Akter S, Kochi T, Hu H, Eguchi M, Yamaguchi M, et al. Association of social jetlag with metabolic syndrome among Japanese working population: the Furukawa nutrition and health study. Sleep Med. 2018;51:53–8.
Koopman ADM, Rauh SP, Van’t Riet E, Groeneveld L, Van Der Heijden AA, Elders PJ, et al. The association between social jetlag, the metabolic syndrome, and type 2 diabetes mellitus in the general population: the new Hoorn study. J Biol Rhythm. 2017;32(4):359–68.
Cespedes Feliciano EM, Rifas-Shiman SL, Quante M, Redline S, Oken E, Taveras EM. Chronotype, social jet lag, and cardiometabolic risk factors in early adolescence. JAMA Pediatr. 2019;173(11):1049–57.
Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes. 2015;39(5):842–8.
Mota MC, Silva CM, Balieiro LCT, Fahmy WM, Crispim CA. Social jetlag and metabolic control in non-communicable chronic diseases: a study addressing different obesity statuses. Sci Rep. 2017;7(1).
Kelly RM, Finn J, Healy U, Gallen D, Sreenan S, McDermott JH, et al. Greater social jetlag associates with higher HbA1c in adults with type 2 diabetes: a cross sectional study. Sleep Med. 2020;66:1–9.
Rusu A, Ciobanu D, Bala C, Cerghizan A, Roman G. Social jetlag, sleep-related parameters, and glycemic control in adults with type 1 diabetes: results of a cross-sectional study. J Diabetes. 2019;11(5):394–401.
McMahon DM, Burch JB, Youngstedt SD, Wirth MD, Hardin JW, Hurley TG, et al. Relationships between chronotype, social jetlag, sleep, obesity and blood pressure in healthy young adults. Chronobiol Int. 2019;36(4):493–509.
Rugerio Z, Cambras IP. Social jet lag associates negatively with the adherence to the Mediterranean diet and body mass index among young adults. Nutrients. 2019 [cited 2020 Feb 17];11(8):1756. Available from: https://www.mdpi.com/2072-6643/11/8/1756
Sohail S, Yu L, Bennett DA, Buchman AS, Lim ASP. Irregular 24-hour activity rhythms and the metabolic syndrome in older adults. Chronobiol Int. 2015;32(6):802–13.
Cespedes Feliciano EM, Quante M, Weng J, Mitchell JA, James P, Marinac CR, et al. Actigraphy-derived daily rest–activity patterns and body mass index in community-dwelling adults. Sleep. 2017 [cited 2020 Feb 17];40(12). Available from: https://academic.oup.com/sleep/article/doi/10.1093/sleep/zsx168/4344553.
Cavalcanti-Ferreira P, Berk L, Daher N, Campus T, Araujo J, Petrofsky J, et al. A nonparametric methodological analysis of rest-activity rhythm in type 2 diabetes. Sleep Sci. 2018;11(4):281–9.
St-Onge M, Campbell A, Zuraikat FM, Cheng B, Shah R, Berger J, et al. Impact of change in bedtime variability on body composition and inflammation: secondary findings from the Go Red for Women Strategically Focused Research Network. Int J Obes. 2020.
Morris CJ, Yang JN, Garcia JI, Myers S, Bozzi I, Wang W, et al. Endogenous circadian system and circadian misalignment impact glucose tolerance via separate mechanisms in humans. Proc Natl Acad Sci U S A. 2015;112(17):E2225–34.
Morris CJ, Purvis TE, Mistretta J, Scheer FAJL. Effects of the internal circadian system and circadian misalignment on glucose tolerance in chronic shift workers. J Clin Endocrinol Metab. 2016 [cited 2020 Apr 13];101(3):1066–74. Available from: https://academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2015-3924.
Owino S, Buonfiglio DDC, Tchio C, Tosini G. Melatonin signaling a key regulator of glucose homeostasis and energy metabolism. Front Endocrinol (Lausanne). 2019;10:488.
Kim TW, Jeong JH, Hong SC. The impact of sleep and circadian disturbance on hormones and metabolism. Int J Endocrinol. 2015;2015:1–9.
He F, Bixler EO, Berg A, Imamura Kawasawa Y, Vgontzas AN, Fernandez-Mendoza J, et al. Habitual sleep variability, not sleep duration, is associated with caloric intake in adolescents. Sleep Med. 2015 [cited 2019 Jun 25];16(7):856–61. Available from: https://www.sciencedirect.com/science/article/pii/S1389945715006772?via%3Dihub.
He F, Bixler EO, Liao J, Berg A, Imamura Kawasawa Y, Fernandez-Mendoza J, et al. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015 [cited 2019 Jun 25];16(12):1489–94. Available from: https://www.sciencedirect.com/science/article/pii/S1389945715009235?via%3Dihub.
Morris CJ, Aeschbach D, Scheer FAJL. Circadian system, sleep and endocrinology. Mol Cell Endocrinol. 2012;349(1):91–104.
Cipolla-Neto J, Amaral FG, Afeche SC, Tan DX, Reiter RJ. Melatonin, energy metabolism, and obesity: a review. J Pineal Res. 2014 May 1 [cited 2020 May 11];56(4):371–81. Available from: http://doi.wiley.com/10.1111/jpi.12137
Funding
Dr. St-Onge is funded by NIH Grants R01 HL128226 and R01 HL142648 and an AHA Go Red for Women Grant 16SFRN27950012. Dr. Zuraikat is a Berrie Fellow in Diabetes Research and is supported by NIH Grant T32 HL007343. Dr. Makarem is supported by a NIH K99/R00 Pathway to Independence Award from NHLBI (Grant # K99 HL148511). Dr. Redline is supported by NIH Grant R35 HL135818. Dr. Aggarwal is funded by an AHA Go Red for Women Grant 16SFRN27960011. Dr. Jelic is funded by NIH grants R01 HL106041 and R01 HL137234 as well as by an AHA Go Red for Women Grant 16SFRN29050000.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and compiled with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Obesity
Rights and permissions
About this article
Cite this article
Zuraikat, F.M., Makarem, N., Redline, S. et al. Sleep Regularity and Cardiometabolic Heath: Is Variability in Sleep Patterns a Risk Factor for Excess Adiposity and Glycemic Dysregulation?. Curr Diab Rep 20, 38 (2020). https://doi.org/10.1007/s11892-020-01324-w
Published:
DOI: https://doi.org/10.1007/s11892-020-01324-w