Abstract
Purpose
Breast cancer continues to be the most commonly diagnosed cancer among Canadian women, with as many as 25–60% of women suffering from chronic neuropathic pain (CNP) as a pervasive consequence of treatment. While pharmacological interventions have shown limited efficacy for the management of CNP to date, psychological interventions, such as mindfulness-based stress reduction (MBSR), may be a promising alterative for improving pain-related problems. The purpose of this study was to use brain imaging methods to investigate this potential.
Methods
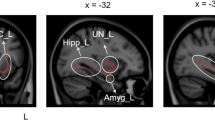
Resting-state fMRI was used in female breast cancer survivors with CNP before and after an 8-week MBSR course (n = 13) and compared with a waitlist control group (n = 10).
Results
Focusing on the default mode network, the most significant results show greater posterior cingulate connectivity with medial prefrontal regions post-MBSR intervention. Moreover, this change in connectivity correlated with reduced pain severity for the MBSR group.
Conclusions
These results provide empirical evidence of a change in the brain following MBSR intervention associated with changes in the subjective experience of pain.
Implications for Cancer Survivors
This study gives hope for a non-invasive method of easing the struggle of CNP in women following breast cancer treatment.




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Brenner DR, Weir HK, Demers AA, Ellison LF, Louzado C, Shaw A, et al. Projected estimates of cancer in Canada in 2020. Can Med Assoc J. 2020;192(9):E199–205.
Jung BF, Ahrendt GM, Oaklander AL, Dworkin RH. Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain. 2003;104:1–13.
Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology. 2008;70(18):1630–5.
Bredal IS, Smeby NA, Ottesen S, Warncke T, Schlichting E. Chronic pain in breast cancer survivors: comparison of psychosocial, surgical, and medical characteristics between survivors with and without pain. J Pain Symptom Manag. 2014;48(5):852–62.
Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, et al. Neuropathic pain. Nature Reviews Disease Primers. 2017;3:17002.
Bokhari F, Sawatzky JAV. Chronic neuropathic pain in women after breast cancer treatment. Pain Manag Nurs. 2009;10(4):197–205.
Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med. 2017;51(2):199–213.
Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–90.
Khoo E-L, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network meta-analysis. Evidence-Based Mental Health. 2019;22(1):26–35.
Pleman B, Park M, Han X, Price LL, Bannuru RR, Harvey WF, et al. Mindfulness is associated with psychological health and moderates the impact of fibromyalgia. Clin Rheumatol. 2019;38(6):1737–45.
Poulin P, Romanow H, Rahbari N, Small R, Smyth CE, Hatchard T, et al. The relationship between mindfulness, pain intensity, pain catastrophizing, depression, and quality of life among cancer survivors living with chronic neuropathic pain. Support Care Cancer. 2016;24(10):4167–75.
Rozworska KA, Poulin PA, Carson A, Tasca GA, Nathan HJ. Mediators and moderators of change in mindfulness-based stress reduction for painful diabetic peripheral neuropathy. J Behav Med. 2020;43(2):297–307.
Lengacher CA, Reich RR, Paterson CL, Ramesar S, Park JY, Alinat C, et al. Examination of broad symptom improvement resulting from mindfulness-based stress reduction in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2016;34(24):2827–34.
Matchim Y, Armer JM, Stewart BR. Effects of mindfulness-based stress reduction (MBSR) on health among breast cancer survivors. West J Nurs Res. 2011;33(8):996–1016.
Hoffman CJ, Ersser SJ, Hopkinson JB, Nicholls PG, Harrington JE, Thomas PW. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and well-being in stage 0 to III breast cancer: a randomized, controlled trial. J Clin Oncol. 2012;30(12):1335–42.
Lerman R, Jarski R, Rea H, Gellish R, Vicini F. Improving symptoms and quality of life of female cancer survivors: a randomized controlled study. Ann Surg Oncol. 2012;19(2):373–8.
Raichle ME. The brain’s default mode network. Annu Rev Neurosci. 2015;38:433–47.
Khan RS, Ahmed K, Blakeway E, Skapinakis P, Nihoyannopoulos L, Macleod K, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201(1):122–31.
Toth C, Brady S, Hatfield M. The importance of catastrophizing for successful pharmacological treatment of peripheral neuropathic pain. J Pain Res. 2014;7:327–38.
Baliki MN, Mansour AR, Baria AT, Apkarian AV. Functional reorganization of the default mode network across chronic pain conditions. PLoS ONE. 2014;9:e106133.
Malfliet A, Coppieters I, Van Wilgen P, Kregel J, De Pauw R, Dolphens M, et al. Brain changes associated with cognitive and emotional factors in chronic pain: a systematic review. Eur J Pain. 2017;21:769–86.
Baliki MN, Geha PY, Apkarian AV, Chialvo DR. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. 2008;28(6):1398–403.
Harrison R, Zeidan F, Kitsaras G, Ozcelik D, Salomons TV. Trait mindfulness is associated with lower pain reactivity and connectivity of the default mode network. J Pain. 2019;20(6):645–54.
Loggia ML, Kim J, Gollub RL, Vangel MG, Kirsch I, Kong J, et al. Default mode network connectivity encodes clinical pain: an arterial spin labeling study. Pain. 2013;154(1):24–33.
Kucyi A, Moayedi M, Weissman-Fogel I, Goldberg MB, Freeman BV, Tenenbaum HC, et al. Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. J Neurosci. 2014;34(11):3969–75.
Shergill Y, Rice D, Khoo EL, Jarvis G, Zhang T, Taljaard M, Monterio L, et al. Mindfulness-based stress reduction in breast cancer survivors with chronic neuropathic pain: a randomized controlled trial. [unpublished results –under review in Pain]. n.d.
Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap. 1994;23(2):129–38.
Baer A, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45.
Tan G, Jensen MP, Thornby JI, Shanti BF. Validation of the Brief Pain Inventory for chronic non-malignant pain. Pain. 2004;5(2):133–7.
Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, et al. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–42.
Faes MC, Reelick MF, Perry M, Olde Rikkert MG, Borm GF. Studies with group treatments required special power calculations, allocation methods, and statistical analyses. J Clin Epidemiol. 2012;65(2):138–46.
Jiang B, Mu W, Wang J, Lu J, Jiang S, Li L, et al. MicroRNA-138 functions as a tumor suppressor in osteosarcoma by targeting differentiated embryonic chondrocyte gene 2. Journal of Experimental & Clinical Cancer Research: CR. 2016;35:69.
Gusnard DA, Akbudak E, Shulman GL, Raichle ME. Medial prefrontal cortex and self-referential mental activity: relation to a default mode of brain function. Proc Natl Acad Sci U S A. 2001;98(7):4259–64.
Cauda F, D’Agata F, Sacco K, Duca S, Cocito D, Paolasso I, et al. Altered resting state attentional networks in diabetic neuropathic pain. J Neurol Neurosurg Psychiatry. 2010;81(7):806–11.
Li J, Huang X, Sang K, Bodner M, Ma K, Dong X-W. Modulation of prefrontal connectivity in postherpetic neuralgia patients with chronic pain: a resting-state functional magnetic resonance–imaging study. J Pain Res. 2018;11:2131–44.
Mills EP, Di Pietro F, Alshelh Z, Peck CC, Murray GM, Russell Vickers E, et al. Brainstem pain-control circuitry connectivity in chronic neuropathic pain. Neurobiol Dis. 2018;38(2):465–73.
Acknowledgments
The authors wish to thank the MRI technologists from the Ottawa Hospital for their assistance with data collection. We also thank the participants, MBSR group leaders, and the research staff involved in the primary study.
Funding
This work was supported by the Canadian Institutes of Health Research and the Canadian Breast Cancer Foundation.
Author information
Authors and Affiliations
Contributions
AS: conceptualization, supervision, resources, investigation, funding acquisition, writing, data curation, formal analysis, methodology, visualization, design. AL: writing—original draft. ZF: formal analysis, resources, visualization, writing—review and editing. TH: investigation, writing—review and editing. OM: investigation. MS: writing—review and editing. AF: writing—review and editing. PP: conceptualization, funding acquisition, writing—review and editing, supervision.
Corresponding author
Ethics declarations
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Smith, A.M., Leeming, A., Fang, Z. et al. Mindfulness-based stress reduction alters brain activity for breast cancer survivors with chronic neuropathic pain: preliminary evidence from resting-state fMRI. J Cancer Surviv 15, 518–525 (2021). https://doi.org/10.1007/s11764-020-00945-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-020-00945-0