Abstract
Background
Bariatric surgery is the most effective treatment for morbid obesity, yet 20 to 30% of such patients regain weight approximately 2 years post-surgery. A psychological intervention adjunctive to bariatric surgery that addresses eating pathology often observed in bariatric populations may improve outcomes. In the present study, a brief, adapted DBT-ST group for bariatric surgical candidates was evaluated as an adjunctive intervention to bariatric surgery in the pre-surgical period to reduce eating pathology and clinical impairment.
Methods
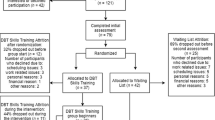
Participants included 95 bariatric surgery candidates, with 50 candidates in the DBT-ST plus treatment as usual (TAU) group and 45 candidates in the TAU (i.e., comparison) group. Participants completed measures of eating pathology at three time points (i.e., T1 = pre-DBT-ST program; T2 = post-DBT-ST program; T3 = 4 months post-DBT-ST; comparable time points employed for TAU group). Average wait time for surgery following the pre-surgical program was approximately 2 to 4 months.
Results
A series of 2 (group: DBT-ST + TAU versus TAU) × 3 (assessment time: T1, T2, and T3) mixed-model ANOVAs were completed. Participants in the DBT-ST plus TAU group showed significant reductions in binge eating, emotional eating, global eating pathology, and clinical impairment related to eating difficulties over time in comparison to TAU.
Conclusions
Findings demonstrated that a brief DBT-ST group integrated as an adjunctive intervention to TAU in a bariatric pre-surgical program could aid in addressing eating pathology. Bariatric participants in a DBT-ST plus TAU group may be on a better weight loss trajectory than those who only receive TAU.

Similar content being viewed by others
References
Brethauer SA, Chand B, Schauer PR. Risks and benefits of bariatric surgery: current evidence. Cleve Clin J Med. 2006;73(11):993–1007.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–8.
Kral JG. Eating disorders and obesity: a comprehensive handbook. New York: The Guilford Press; 1995.
Frühbeck G. Bariatric and metabolic surgery: a shift in eligibility and success criteria. Nat Rev Endocrinol. 2015;11(8):465–77.
Maggard MA, Shugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142:547–59.
Nocca D, Krawezykowsky D, Bomans B, et al. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18(5):560–5.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18(6):648–51.
Nicoletti CF, Oliveira BA, Pinhel MA, et al. Influences of excess weight loss and weight regain on biochemical indicators during a 4-year follow-up after Roux-en-Y gastric bypass. Obes Surg. 2015;25(2):279–84.
Chang SH, Stoll CRT, Song J, et al. The effectiveness and risks of bariatric surgery. An updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149:275–87.
Puzziferri N, Rosheck TB, Gallegher R, et al. Long-term follow up after bariatric surgery. A systematic review. JAMA. 2014;312:934–42.
Karmali S, Brar R, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23:1922–33.
Sugerman HJ. Bariatric surgery for severe obesity. J Assoc Acad Minor Phys. 2001;12:129–36.
Kushner RF, Sorensen KW. Prevention of weight regain following bariatric surgery. Curr Obes Rep. 2015;4:198–206.
Conceicao EM, Utzinger LM, Mitchell JE. Eating disorders and problematic eating behaviours before and after bariatric surgery: characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev. 2015;23(6):417–25.
Campos JM, Lins DC, Silva LB, et al. Metabolic surgery, weight regain, and diabetes re-emergence. Arq Bras Circ Dig. 2013;26(Suppl1):57–62.
Hsu LKG, Betancourt S, Sullivan SP. Eating disturbances before and after vertical banded gastroplasty: a pilot study. Int J Eat Disord. 1996;19(1):23–34.
Lopez PP, Patel NA, Koche LS. Outpatient complications encountered following Roux-en Y gastric by-pass. Med Clin N Am. 2007;91:471–83.
Malone M, Alger-Mayer S. Binge status and quality of life after gastric bypass surgery: a one-year study. Obesity Res. 2004;12:473–81.
Mundi MS, Lorentz PA, Swain J, et al. Moderate physical activity as predictor of weight loss after bariatric surgery. Obes Surg. 2013;23(10):1645–9.
Shah M, Simha V, Garg A. Review: long term impact of bariatric surgery on body weight, comorbities, and nutritional status. J Clin Endocrinol Metab. 2006;91:4223–31.
Spitzer RR, Devleu M, Walsh BT, et al. Binge eating disorder: a multisite field trial of the diagnostic criteria. Int J Eat Disord. 1992;11:191–203.
Hsu LKG, Sullivan SP, Benotti PN. Eating disturbances and outcome of gastric bypass surgery: a pilot study. Int J Eat Disord. 1997;21(4):385–90.
Kalarchian MA, Marcus MD. Management of the bariatric surgery patient: is there a role for the cognitive behavior therapist? Cogn Behav Pract. 2003;10(2):112–0.
Jones-Corneille LR, Wadden TA, Sarwer DB, et al. Axis I psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical interviews. Obes Surg. 2012;22(3):389–97.
Busetto L, Valente P, Pisent C, et al. Eating pattern in the first year following adjustable silicone gastric banding (ASGB) for morbid obesity. Int J Obes Relat Metab Disord. 1996;20(6):539–46.
Beck NN, Mehlsen M, Stoving RK. Psychological characteristics and associations with weight outcomes two years after gastric bypass surgery: postoperative eating disorder symptoms are associated with weight loss outcomes. Eat Behav. 2012;4:394–7.
Chao AM, Wadden TA, Faulconbridge LF, et al. Binge-eating disorder and the outcome of bariatric surgery in a prospective, observational study: two-year results. Obesity. 2016;24(11):2327–33.
Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016;12:1058–67.
Niego SH, Kofman MD, Weiss JJ, et al. Binge eating in the bariatric surgery population: a review of the literature. Int J Eat Disord. 2007;4:349–59.
Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence, and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4(5):640–6.
Chesler BE. Emotional eating: a virtually untreated risk factor for outcome following bariatric surgery. ScientificWorldJournal. 2012;2012:365961.
Gelinas BL, Delparte CA, Hart R, et al. Unrealistic weight loss goals and expectations among bariatric surgery candidates: the impact of sex on pre-surgical weight outcomes. Bari Nurs Surg Patient Care. 2013;8(1):12–7.
Fischer S, Smith GT, Anderson KG. Clarifying the role of impulsivity in bulimia nervosa. Int J Eat Disord. 2007a;33:406–11.
Ochner CN, Dambkowski CL, Yeomans BL, et al. Pre-bariatric surgery weight loss requirements and the effect of preoperative weight loss on postoperative outcome. Int J Obes. 2012;36(11):1380–7.
Liu R. The impact of pre-bariatric surgery psychosocial and behavioural interventions on body composition measures in adults: a systematic review. Can J Diabetes. 2015;39:S38–74.
Abilés V, Abilés J, Rodriguez-Ruiz S, et al. Effectiveness of cognitive-behavioural therapy on weight loss after two years of bariatric surgery in morbidity obese patients. Nutr Hosp. 2013a;28(4):1109–14.
Abilés V, Rodriguez-Ruiz S, Abilés J, et al. Effectiveness of cognitive-behavioral therapy in morbidity obese candidates for bariatric surgery with and without binge eating disorder. Nutr Hosp. 2013b;28:1523–9.
Ashton K, Drerup M, Windover A, et al. Brief, four-session group CBT reduces binge eating behaviors among bariatric surgery candidates. Surg Obes Relat Dis. 2009;5:257–62.
Ashton K, Heinberg L, Windover A, et al. Positive response to binge eating intervention enhances postoperative weight loss. Surg Obes Relat Dis. 2011;7:315–20.
Gade H, Friborg O, Rosenvinge JH, et al. The impact of a preoperative cognitive behavioural therapy (CBT) on dysfunctional eating behaviours, affective symptoms and body weight 1 year after bariatric surgery: a randomized controlled trial. Obes Surg. 2015:1–6.
Leahey TM, Crowther JH, Irwin SR. A cognitive-behavioral mindfulness group therapy intervention for the treatment of binge eating in bariatric surgery patients. Cogn Behav Prac. 2008;15:364–75.
Lier HO, Biringer E, Stubhaug B, et al. The impact of preoperative counseling on postoperative treatment adherence in bariatric surgery patients: a randomized controlled trial. Patient Educ Couns. 2012;87:336–42.
Weineland S, Arvidsson D, Kakoulidis TP, et al. Acceptance and commitment therapy for bariatric surgery patients, a pilot RCT. Obes Res Clin Pract. 2012a;6:e21–30.
Weineland S, Hayes SC, Dahl J. Psychological flexibility and the gains of acceptance-based treatment for post-bariatric surgery: six-month follow-up and a test of the underlying model. Clin Obes. 2012b;2:15–24.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22(1):70–89.
Cassin SE, Sockalingam S, Du C, et al. A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav Res Ther. 2016;80:17–22.
Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41(5):509–28.
Heatherton TF, Baumeister RF. Binge eating as an escape from self-awareness. Psychol Bull. 1991;110(1):86–108.
Wiser S, Telch CF. Dialectical behavior therapy for binge-eating disorder. In Session: Psychotherapy in Practice. J Clin Psychol. 1999;55:755–68.
Villarejo C, Fernandez-Aranda F, Jimenez-Murcia S, et al. Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. Eur Eat Disord Rev. 2012;20(3):250–4.
Silva I. Importance of emotional regulation in obesity and weight loss treatment. Fractal: Revista de Psicologia. 2015;27(3):286–190.
Gianini LM, White MA, Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with binge eating disorder. Eat Behav. 2013;14(3):309–13. https://doi.org/10.1016/j.eatbeh.2013.05.008.
Miller-Matero LR, Armstrong R, McCulloch K, et al. To eat or not to eat; is that really the question? An evaluation of problematic eating behaviors and mental health among bariatric surgery candidates. Eat Weight Disord. 2014;19(3):377–82.
Opolski M, Chur-Hansen A, Wittert G. The eating related behaviours, disorders and expectations of candidates for bariatric surgery. Clin Obes. 2015;5(4):165–97.
Lavender JM, Anderson DA. Contribution of emotion regulation difficulties to disordered eating and body dissatisfaction in college men. Int J Eat Disord. 2010;43:352–7.
Svaldi J, Griepenstroh J, Tuschn-Caffier B, et al. Emotion regulation deficits in eating disorders: a marker of eating pathology or general psychopathology? Psychiatry Res. 2012;197:103–11.
Micanti F, Iasevoli F, Cucciniello C, et al. The relationship between emotional regulation and eating behaviour: a multidimensional analysis of obesity psychopathology. Eat Weight Disord. 2017;22(1):105–15.
Rosik CH. Psychiatric symptoms among prospective bariatric surgery patients: rates of prevalence and their relation to social desirability, pursuit of surgery, and follow-up attendance. Obes Surg. 2005;15:677–83.
Sarwer DB, Cohn NI, Gibbons LM, et al. Psychiatric diagnoses and psychiatric treatment among bariatric surgery candidates. Obes Surg. 2004;14:1148–56.
Linehan MM. Cognitive behavioural treatment of borderline personality disorder. New York: The Guilford Press; 1993.
Heidi HL, Linehan MM. Dialectical behavior therapy: an integrative approach to the treatment of borderline personality disorder. J Psychother Integr. 1994;4(1):55–82.
Palmer RL, Birchall H, Damani S, et al. A dialectical behaviour therapy program for people with an eating disorder and borderline personality disorder - description and outcome. Int J Eat Disord. 2003;33(3):281–6.
Klein AS, Skinner JB, Hawley KM. Adapted group-based dialectical behaviour therapy for binge eating in a practicing clinic: clinical outcomes and attrition. Eur Eat Disord. 2012;20(3):e148–53.
Klein AS, Skinner JB, Hawley KM. Targeting binge eating through components of dialectical behaviour therapy: preliminary outcomes for individually supported diary card self-monitoring versus group-based DBT. Psychotherapy (Chic). 2013;50(4):543–52.
Masson PC, Von Ranson KM, Wallace LM, et al. A randomized wait-list controlled pilot study of dialectical behaviour therapy guided self-help for binge eating disorder. Behav Res Ther. 2013;51(11):723–8.
Safer DL, Robinson AH, Jo B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: comparing dialectical behaviour therapy adapted for binge eating to an active comparison group therapy. Behav Ther. 2010a;41(1):106–20.
Telch CF. Skills training treatment for adaptive affect regulation in a woman with binge-eating disorder. Int J Eat Disord. 1997;22(1):77–81.
Telch CF, Agras WS, Linehan MM. Group dialectical behavior therapy for binge-eating disorder: a preliminary, uncontrolled trial. Behav Ther. 2000;31(3):569–82.
Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. J Consult Clin Psychol. 2001;69(6):1061–5.
Safer DL, Lively TJ, Telch CF, et al. Predictors of relapse following successful dialectical behavior therapy for binge eating disorder. Int J Eat Disord. 2002;32(2):155–63.
Safer DL, Robinson AH, Jo B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behav Ther. 2010b;41(1):106–20.
Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. Am J Psychiatry. 2001;158(4):632–4.
Safer DL, Telch CF, Chen EY. Dialectical behavior therapy for binge eating and bulimia. New York: The Guilford Press; 2009.
Field AE, Herzog DB, Keller MB, et al. Distinguishing recover from remission in a cohort of bulimic women: how should asymptomatic periods be described? J Clin Epidemiol. 1997;50:1339–45.
McFarlane T, Olmsted MP, Trottier K. Timing and prediction of relapse in a transdiagnostic eating disorder sample. Int J Eat Disord. 2008;41(7):587–93.
Milos G, Spindler A, Schnyder U, et al. Instability of eating disorder diagnoses: prospective study. Br J Psychiatry. 2005;187:573–8.
Fairburn CG, Beglin SJ. Eating disorder examination questionnaire (EDE-Q 6.0). In C.G. Fairburn (Eds), cognitive behavior therapy and eating disorders (appendix II). New York: The Guilford Press; 2008.
Grilo CM, Masheb RB, Brody M, et al. Childhood maltreatment in extremely obese male and female bariatric surgery candidates. Obes Res. 2005;13(1):123–30.
Kalarchian MA, Marcus MD, Wilson GT, et al. Binge eating among gastric bypass patients at long-term follow-up. Obes Surg. 2002;12(2):270–5.
White MA, Masheb RM, Rothschild BS, et al. The prognostic significance of regular binge eating in extremely obese gastric bypass patients: 12-month postoperative outcomes. J Clin Psychiatry. 2006;67(12):1928–35.
Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: longitudinal assessment of bariatric surgery. Surg Obes Relat Dis. 2007;3(2):116–26.
Reas DL, Grilo CM, Masheb RM. Reliability of the eating disorder examination-questionnaire in patients with binge eating disorder. Behav Res Ther. 2006;44(1):43–51.
Hrabosky JI, White MA, Masheb RM, et al. Psychometric evaluation of the eating disorder examination-questionnaire for bariatric surgery candidates. Obes. 2008;16:763–9.
Gormally J, Black S, Daston S, et al. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55.
Alger-Mayer S, Rosati C, Polimeni JM, et al. Preoperative binge eating status and gastric bypass sugery: a long-term outcome study. Obes Surg. 2009;19(2):139–45.
Mazzeo SE, Saunders R, Mitchell KS. Gender and binge eating among bariatric surgery candidates. Eat Behav. 2006;7(1):47–52.
Arnow B, Kenardy J, Agras WS. The emotional eating scale: the development of a measure to assess coping with negative affect by eating. Int J Eat Disord. 1995;18(1):79–90.
Fischer S, Chen E, Katterman S, et al. Emotional eating in a morbidly obese bariatric surgery-seeking population. Obes Surg. 2007b;17(6):778–84.
Bohn K, Fairburn CG. The Clinical Impairment Assessment Questionnaire (CIA). In: Fairburn CG, editor. Cognitive behaviour therapy and eating disorders (appendix III). New York: Guilford Press; 2008.
Spittal MJ, Fruhbeck G. Bariatric surgery: many benefits, but emerging risks. Lancet Diabetes Endocrinol. 2018;6(3):161–3.
Morgan SJ, Ho KM. Incidence and risk factors for deliberate self-harm, mental illness, and suicide following bariatric surgery: a state-wide population-based linked-data cohort study. Ann Surg. 2017;265(2):244–52.
Bhatti JA, Nathens AB, Thiruchelvam D, et al. Self-harm emergencies after bariatric surgery: a population-based cohort study. JAMA Surg. 2016;151(3):226–32.
Gade H, Hjelmesaeth J, Rosenvinge JH, et al. Effectiveness of a cognitive behavioural therapy for dysfunctional eating among patients admitted for bariatric surgery: a randomized controlled trial. J Obes. 2014;2014:127936.
Benfield JA, Szlemko WJ. Internet-based data collection: promises and realities. J Res Pract. 2006;2(2):Article D1.
Acknowledgements
Thank you to Dr. Regan Shercliffe and Dr. Ron Martin for their assistance, encouragement, and contributions to this project.
Funding
This research was funded by the Canadian Institute of Health Research Doctoral Research Award and the Faculty of Graduate Studies and Research at the University of Regina.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Statement
Ethical approval to conduct this study was obtained through the University of Regina and RQHR Research Ethics Boards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Delparte, C.A., Power, H.A., Gelinas, B.L. et al. Examination of the Effectiveness of a Brief, Adapted Dialectical Behavior Therapy-Skills Training Group for Bariatric Surgical Candidates. OBES SURG 29, 252–261 (2019). https://doi.org/10.1007/s11695-018-3515-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3515-2