Abstract
Background
Medical students in the USA have negative perceptions of primary care careers, which are exacerbated by the hidden curriculum and medical school culture. Longitudinal integrated clerkships (LICs) have shown promise in ameliorating this situation by promoting student/preceptor continuity relationships and helping students maintain empathy.
Aim
The aim of this study is to describe the Student Continuity of Practice Experience (SCOPE) program and demonstrate program outcomes using evaluation data from residency match results, course evaluations, and student grades.
Setting
University of Texas Medical Branch, an academic health center in Galveston, Texas.
Participants
Undergraduate medical students.
Program Description
Learners participate in a longitudinal curriculum designed to enhance their skills as primary care physicians. They regularly attend continuity clinic, establishing a panel of patients by their third year. Students receive frequent feedback from a faculty mentor on assignments and clinical performance.
Program Evaluation
SCOPE students have high primary care residency match rates and experience patient continuity rates comparable to an intern. Their interest in primary care increases between years one and three, a departure from typical medical student trends.
Discussion
SCOPE appears to promote and maintain primary care career interest in participants and has transferability to other institutions.
Similar content being viewed by others
INTRODUCTION
One third of the physicians in the USA practice in primary care fields, a number the American Association of Medical Colleges finds inadequate to care for the population.1 Further compounding the primary care physician shortage is a lack of medical student interest in primary care careers.2, 3 Students are influenced by a variety of factors including perceptions of PCP lifestyles and perceived lower prestige associated with the field, as well as their desired future patient population4, 5 and the disparity in reimbursement models for specialists versus generalists.2, 6, 7 The effects of a “hidden curriculum,” which are the systemic and organizational influences at play in an institution’s culture, further discourage students from primary care careers.8, 9 In addition, students tend to lose interest in primary care over the course of medical school; about half of the students who start their education interested in primary care switch to a non-primary care field by graduation.10, 11
Consequently, medical educators have a vested interest in pursuing educational experiences that will encourage students to consider primary care careers. Though several existing medical education practices have shown promise in this direction a cohesive model is lacking.
The most promising model to foster primary care interest is the longitudinal integrated clerkship (LIC), which is structured to allow students to care for a panel of patients over time in the same setting with the same faculty mentors. LICs and primary care are a natural fit, both emphasizing patient-centered care and continuity relationships among students, faculty, and patients, which can also have positive effects on students’ primary care career selection.12,13,14
Students in LICs experience continuity across multiple dimensions—“continuity of patient contact and care, continuity of assessment and supervision, and continuity of clinical and cultural learning through patients, peers, health providers, and community health and social resources”.15 Continuity with preceptors is especially important as they play a key role in shaping students’ perceptions of primary care careers. Stagg et al.16 found student/preceptor relationships have the greatest effect on student career choice when multiple dimensions of continuity are present.
The LIC model does have limitations. LICs do not take full advantage of the opportunity to promote continuity due to their relatively short length. Though longer than many other training models, LICs are usually maximum one year in duration and restricted to the first clerkship year.17 By this time, most students have already changed their specialty interest, typically away from primary care.10 While they do encourage many positive outcomes, LICs do not necessarily aim to increase primary care interest or to alter institutional perceptions of primary care careers.12
Given all the benefits continuity models like LICs can bring to students and with an awareness of their limitations, we designed a curriculum that embraces the best parts of the LIC while increasing its duration and adding components to enhance learner perceptions of primary care. Our longitudinal continuity program, Student Continuity of Practice Experience (SCOPE), has three broad goals:
-
1.
To introduce students to the concept of longitudinal primary patient care in a patient-centered medical home model early and repeatedly throughout their medical education
-
2.
To utilize patient interactions and faculty mentor relationships to enhance primary care clinical skills, as well as develop enthusiasm for a career in primary care
-
3.
To create an institutional culture where primary care is viewed as a positive, dynamic career choice by students
The aim of this study is to describe the SCOPE program and to demonstrate program outcomes to date, focusing on primary care interest and persistence and on dimensions of continuity in our student population.
SETTING AND PARTICIPANTS
The University of Texas Medical Branch (UTMB) is a large academic health center located in Galveston, Texas. We have an average medical school class size of 230 students and diverse student demographics; 31.9% are from underrepresented minority groups. Our curriculum is a traditional four year model, with two years of preclinical education followed by two years of clinical training.
Institutionally, UTMB defines primary care as Family Medicine, General Internal Medicine, Obstetrics and Gynecology, and Pediatrics. SCOPE places students at a variety of ambulatory practices affiliated with the following departments: General Internal Medicine, Pediatrics, Family Medicine, Obstetrics and Gynecology, Geriatrics, Psychiatry, Palliative Care, and our student-run free clinic. Although these clinics are not all explicitly in primary care fields they embrace the same patient-centered ethos and continuity paradigm. Students from years one through three of the medical school curriculum participate in SCOPE. For the purposes of this study, our sample includes all students who have participated in SCOPE from 2014 to 2017. This study is a program evaluation which draws from quantitative data sources to address the study aims, including residency match results, course evaluations, and student grades. Our data collection supports SCOPE meeting its goals for the curriculum and the general feasibility of running a longitudinal continuity clinical training program.
PROGRAM DESCRIPTION
SCOPE was launched as a pilot program for one academic year (2014–2015), with participants selected at random from a pool of interested third year students who submitted application essays. Due to its popularity and additional funding from the Texas Higher Education Coordinating Board, SCOPE expanded its enrollment and clinical sites in subsequent years. The following study data was granted exempt status by the University of Texas Medical Branch Institutional Review Board.
Program Admissions
After the pilot year we modified the admissions process, adding an essay component, multiple mini interviews (MMIs) and an abbreviated version of the survey “Medical Student Attitudes Toward the Underserved.” The applicants were scored on each component and ranked by total score for program selection. Application data were reviewed by the faculty leadership team to make final determinations.
Faculty Champion
Students select their preferred specialty area within primary care and are placed at a clinic with a dedicated preceptor. This preceptor, called a faculty champion, supervises the student in clinic and provides regular verbal feedback on their performance, as well as written feedback on assignments. Each student stays with the same faculty champion at the same clinic throughout their time in SCOPE, with the potential to maintain this continuity for their entire medical school career.
Clinical Component
Preclinical students’ visits take place approximately monthly throughout the academic year. After each visit, preclinical students complete a written assignment, which include patient notes, reflective essays, and guideline research reports. Students also post an informal list of “5 Things I Learned in Clinic” to a faculty-monitored online discussion board after every visit to encourage regular reflection on their learning. Third year students increase their SCOPE visits to one half-day per week. They take greater responsibility for patient care, essentially becoming junior partners in the clinic practice. Our electronic medical record allows for the creation of patient lists for students, which connects the student provider with their patients and allows for greater ownership of care.
Didactic Component
Didactics for preclinical learners take the form of quarterly dinner meetings, covering topics such as health literacy and treatment adherence. Students participate in clinical skill-building workshops geared to their level of training, as well as a week-long Public Health elective course developed by the Department of Preventive Medicine and Community Health.
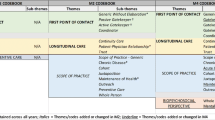
The third year students meet monthly with SCOPE faculty for a half-day workshop. The workshops cover a variety of topics, as described in Table 1. Students have a corresponding written assignment for each didactic session. Monthly didactics include a small group component that incorporates reflective dialog, responding to prompts which ask students to reflect on their role as a healer in the past month.
Third year students are required to complete a quality improvement (QI) project at their clinic. Two monthly workshops are dedicated to teaching students about quality improvement, with follow-up assignments to ensure they are progressing appropriately. Faculty also provide guidance on student QI projects, directing students’ research and connecting them with necessary resources.
Feedback and Assessment
Students receive verbal or written feedback from their faculty champion on all written assignments. Feedback cards are distributed to students at regular intervals to solicit comments from their faculty champions on specific clinical skills. Third year students receive quarterly, competency-based formative feedback from their faculty champion. Lastly, students receive a final online summative evaluation at the end of the academic year. A full curriculum description is available in Table 1.
PROGRAM OUTCOMES
Student Career Interest
Historical match data for UTMB prior to SCOPE (2013–2015) show an average of 45% of students in the match going into primary care. Primary care match rates have held steady since then at about the same number, as indicated in Table 2. SCOPE student match rates into primary care are higher, which is to be expected given its primary care focus, while SCOPE applicants fall in between the two groups.
All SCOPE students were asked to rate the statement “I plan a career in primary care” on a 5-point Likert scale (1 = Strongly Disagree–5 = Strongly Agree) on their end of course evaluations. This survey was developed by the SCOPE faculty leadership team and incorporated questions from the AAMC’s Graduate Questionnaire as well as Schultz et al.’s18 preceptor survey. SCOPE student interest in primary care increased from 3.25 to 4.32 between years one and three. This is not the typical pattern for primary care interest. Students are more likely to enter medical school interested in primary care and then experience a drop by their third year.10
Continuity Measures
For the last three years, SCOPE third year students have achieved continuity levels at or above that of an intern at our institution, with 18% or greater of their patient logs (730 logs total) indicating continuity patient encounters. SCOPE retention rates have been high, with 77% of second year SCOPE students (N = 20) choosing to continue SCOPE for their third year. By building on the LIC concept and extending its best features across the curriculum, we were able to create a program where students can experience continuity through their undergraduate medical school career and receive the support needed to maintain their professional identity.
Academic Performance
SCOPE students are not selected based on academic achievement, and their preclinical and Step 1 grades do not differ from the larger student population. Even though third year SCOPE students leave their clerkship for a half-day per week, SCOPE participants show slightly higher overall clerkship grade performance than their peers. For example, 24% (N = 37) of SCOPE students’ clerkship grades from 2016 to 2017 were Honors grades as opposed to 15% (N = 183) of non-SCOPE students’ clerkship grades (p = 0.0070, Fisher’s exact).
DISCUSSION
SCOPE’s main curricular features are transferrable to other institutions with similar settings, especially ones with a scattered clinic geography which does not lend itself to the LIC model. While the data thus far suggests student participation in SCOPE leads to a higher incidence of primary care career choice, we need to track our students’ career trajectory over time to see if SCOPE made a continuous impact on their career choices.
Limitations
A major study limitation is selection bias in our student population, as many students are likely to already be oriented towards primary care upon entry to SCOPE. However, since one of SCOPE’s aims is to maintain primary care interest, this limitation is acceptable though it does constrain our ability to draw conclusions about SCOPE’s role in encouraging students towards primary care careers. We also are limited in accounting for outside factors, such as lifestyle preferences, that influence students’ primary care selection. Scalability to a larger student population is another limitation; increasing student numbers requires significant resources that may not be available.
CONCLUSION
We have developed a longitudinal continuity clinical training program with competency-based feedback and regular evaluation of student assignments, as well as professional and personal development. The longitudinal curriculum allows multiple opportunities to reinforce student learning, provide formative feedback, and create close mentoring relationships between students and faculty. The SCOPE model shows promise as a way to maintain and possibly increase student interest in primary care and positively impact institutional attitudes towards the field.
References
IHC, Inc. The complexities of physician supply and demand 2016 update: projections from 2014–2025 [Internet]. Washington, DC: American Association of Medical Colleges; 2016 [cited 2017 Apr 24]. Available from https://www.aamc.org/download/458082/data/2016_complexities_of_supply_and_demand_projections.pdf.
Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, Battistone M, DeFer T, Elnicki M, Harrell H, Reddy S. Factors associated with medical students' career choices regarding internal medicine. JAMA 2008 Sep 10;300(10):1154–64.
Stone VE, Kormos WA, Levitan SE, Shannon S, Michener JL, Martin JJ, Barry MJ. Physician education and training in primary care. In: Culliton B, Russell S, eds. Who will provide primary care and how will they be trained? Proceedings of a Conference Sponsored by the Josiah Macy, Jr. Foundation; 2010; Durham, N.C. Josiah Macy, Jr. Foundation; 2010. p 109–65.
Clinite KL, Reddy ST, Kazantsev SM, Kogan JR, Durning SJ, Blevins T, Chou CL, Diemer G, Dunne DW, Fagan MJ, Hartung PJ. Primary care, the ROAD less traveled: what first-year medical students want in a specialty. Acad Med 2013; 88(10):1522–8.
Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997–2006. Acad Med 2010 Jun 1; 85(6):947–58.
Bodenheimer T, Berenson RA, Rudolf P. The primary care–specialty income gap: why it matters. Ann Intern Med 2007; 146(4):301–6.
Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med 2010; 85: S81-S8.
Hafferty FW. Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med 1998 Apr;73(4):403–7.
Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med 2013; 88(12):1919–26.
Compton MT, Frank E, Elon L, Carrera J. Changes in US medical students’ specialty interests over the course of medical school. J Gen Intern Med 2008; 23(7):1095–100.
Babbott D. The stability of specialty preferences among U.S. medical school graduates in 1983. JAMA 1988; 259:1970–5.
Walters L, Greenhill J, Richards J, Ward H, Campbell N, Ash J, Schuwirth LW. Outcomes of longitudinal integrated clinical placements for students, clinicians and society. Med Educ 2012; 46: 1028–41.
Poncelet AN, Mazotti LA, Blumberg B, Wamsley MA, Grennan T, Shore WB. Creating a longitudinal integrated clerkship with mutual benefits for an academic medical center and a community health system. Perm J 2014; 18: 50.
Henschen BL, Bierman JA, Wayne DB, Ryan ER, Thomas JX, Curry RH, Evans DB. Four-year educational and patient care outcomes of a team-based primary care longitudinal clerkship. Acad Med 2015; 90: S43-S9.
Ellaway R, Graves L, Berry S, Myhre D, Cummings BA, Konkin J. Twelve tips for designing and running longitudinal integrated clerkships. Med Teach 2013; 35: 989–95.
Stagg P, Prideaux D, Greenhill J, Sweet L. Are medical students influenced by preceptors in making career choices, and if so how? A systematic review. Rural Remote Health [Internet]. 2012 [cited 2017 Apr 24]; 12 (1832):[about 21 p.]. Available from http://www.rrh.org.au.
Norris TE, Schaad DC, DeWitt D, Ogur B, Hunt DD. Longitudinal integrated clerkships for medical students: an innovation adopted by medical schools in Australia, Canada, South Africa, and the United States. Acad Med 2009; 84: 902–7.
Schultz KW, Kirby J, Delva D, Godwin M, Verma S, Birtwhistle R, Knapper C, Seguin R. Medical students' and residents' preferred site characteristics and preceptor behaviours for learning in the ambulatory setting: a cross-sectional survey. Med Educ 2004 Dec;4(1):12.
Funding
SCOPE is partially supported by the Primary Care Innovation Grant Program from the Texas Higher Education Coordinating Board.
Author information
Authors and Affiliations
Contributions
The authors wish to thank Dr. Charles Mouton for his contributions in the development of this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Prior Presentations
Poster and oral presentation, Southern Group on Educational Affairs conference, Austin, Texas, 2015; poster and oral presentation, Innovations in Health Science Education conference, Austin, Texas, 2016
Rights and permissions
About this article
Cite this article
Ford, C.D., Patel, P.G., Sierpina, V.S. et al. Longitudinal Continuity Learning Experiences and Primary Care Career Interest: Outcomes from an Innovative Medical School Curriculum. J GEN INTERN MED 33, 1817–1821 (2018). https://doi.org/10.1007/s11606-018-4600-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-018-4600-x