ABSTRACT
BACKGROUND
Quality of U.S. health care has been the focus of increasing attention, with deficiencies in patient care well recognized and documented. However, relatively little is known about the extent to which hospitals engage in quality improvement activities (QIAs) or factors influencing extent of QIAs.
OBJECTIVE
To identify 1) the extent of QIAs in Veterans Administration (VA) inpatient medical services; and 2) factors associated with widespread adoption of QIAs, in particular use of hospitalists, non-physician providers, and extent of goal alignment between the inpatient service and senior managers on commitment to quality.
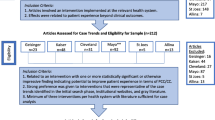
DESIGN
Cross-sectional, descriptive study of QIAs using a survey administered to Chiefs of Medicine (COM) at all 124 VA acute care hospitals. We conducted hierarchical regression, regressing QIA use on facility contextual variables, followed by use of hospitalists, non-physician providers, and goal alignment/quality commitment.
MAIN MEASURES
Outcome measures pertained to use of a set of 27 QIAs and to three dimensions—infrastructure, prevention, and information gathering—that were identified by factor analysis among the 27 QIAs overall.
KEY RESULTS
Survey response rate was 90 % (111/124). Goal alignment/quality commitment was associated with more widespread use of all four QIA categories [infrastructure (b = 0.42; p < 0.001); prevention (b = 0.24; p < 0.001); information gathering (b = 0.28; p = <0.001); and overall QIA (b = 0.31; p < 0.001)], as was greater use of hospitalists [infrastructure (b = 0.55; p = 0.03); prevention (b = 0.61; p < 0.001); information gathering (b = 0.75; p = 0.01); and overall QIAs (b = 0.61; p < 0.001)]; higher occupancy rate was associated with greater infrastructure QIAs (b = 1.05, p = 0.02). Non-physician provider use, hospital size, university affiliation, and geographic region were not associated with QIAs.
CONCLUSION
As hospitals respond to changes in healthcare (e.g., pay for performance, accountable care organizations), this study suggests that practices such as use of hospitalists and leadership focus on goal alignment/quality commitment may lead to greater implementation of QIAs.
Similar content being viewed by others
REFERENCES
Preventing Medication Errors. Washington, DC: National Academies Press; 2006.
Committee on Quality of Health Care in America Institute of Medicine: To Err Is Human: Building a Safer Health System. The National Academies Press; 2000.
Committee on Quality of Health Care in America Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century. The National Academies Press; 2001.
McGlynn EA, Asch SM, Adams J, et al. The Quality of Health Care Delivered to Adults in the United States. N Engl J Med. 2003;348(26):2635–45.
Ross JS, Cha SS, Epstein AJ, et al. Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff. 2007;26(1):238–48.
Landon BE, Normand SL, Lessler A, et al. Quality of care for the treatment of acute medical conditions in US hospitals. Arch Intern Med. 2006;166(22):2511–7.
Kizer KW. Patient safety: a call to action: a consensus statement from the National Quality Forum. Medsc Gen Med. 2001;3(2):10.
Heget JR, Bagian JP, Lee CZ, Gosbee JW, John M. Eisenberg Patient Safety Awards. System innovation: Veterans Health Administration National Center for Patient Safety. Jt Comm J Qual Improv. 2002;28(12):660–5.
Galvin R, Milstein A. Large employers’ new strategies in health care. N Engl J Med. 2002;347(12):939–42.
Safe Practices for Better Health Care: A Consensus Report. Washington, DC: National Quality Forum; 2003.
Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals—the Hospital Quality Alliance program. N Engl J Med. 2005;353(3):265–74.
Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? [see comment]. JAMA. 2005;293(19):2384–90.
Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient-centered care. Am J Manage Care. 2004;10(11 Pt 2):828–36.
Wachter RM. The end of the beginning: patient safety five years after ‘to err is human’. Health affairs. Jul-Dec 2004; Suppl Web Exclusives:W4–534–545.
Clancy CM. Ten years after To Err is Human. Am J Med Qual. 2009;24(6):525–8.
Glasgow JM, Scott-Caziewell JR, Kaboli PJ. Guiding Inpatient Quality Improvement: A Systematic Review of Lean and Six Sigma. Jt Comm J Qual Patient Saf. 2010;36(12):533–40.
Cohen AB, Restuccia JD, Shwartz M, et al. A survey of hospital quality improvement activities. Med Care Res Rev. 2008;65(5):571–95.
Wachter RM. Reflections: the hospitalist movement a decade later. J Hosp Med. 2006;1(4):248–52.
Kaboli PJ, Barrett T, Vazirani S, Osterberg L, Auerbach AD. Hospitalist in the Veteran Health Administration: An Integrated Health Care System. In: Mckean SC, Ross JJ, Dressler DD, Brotman DJ, Ginsberg JS, eds. Principles and Practice of Hospital Medicine. New York: McGraw-Hill; 2012;2245–9.
Conway PH. Value-driven health care: implications for hospitals and hospitalists. J Hosp Med. 2009;4(8):507–11.
Schnipper JL, Magee M, Larsen K, Inzucchi SE, Maynard G. Society of Hospital Medicine Glycemic Control Task Force summary: practical recommendations for assessing the impact of glycemic control efforts. J Hosp Med. 2008;3(5 Suppl):66–75.
Maynard G, Stein J. Designing and implementing effective venous thromboembolism prevention protocols: lessons from collaborative efforts. J Thromb Thrombolysis. 2010;29(2):159–66.
Williams MV, Coleman E. BOOSTing the hospital discharge. J Hosp Med. 2009;4(4):209–10.
Vasilevskis EE, Knebel RJ, Wachter RM, Auerbach AD. California hospital leaders’ views of hospitalists: meeting needs of the present and future. J Hosp Med. 2009;4(9):528–34.
Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218–27.
White HL, Glazier RH. Do hospitalist physicians improve the quality of inpatient care delivery? A systematic review of process, efficiency and outcome measures. BMC Med. 2011;9:58.
Roy CL, Liang CL, Lund M, et al. Implementation of a physician assistant/hospitalist service in an academic medical center: impact on efficiency and patient outcomes. J Hosp Med. 2008;3(5):361–8.
Ford WT, Britting LL. Nonphysician providers in the hospitalist model: a prescription for change and a warning about unintended side effects. J Hosp Med. 2010;5(2):99–102.
Kleinpell RM, Ely EW, Grabenkort R. Nurse practitioners and physician assistants in the intensive care unit: an evidence-based review. Crit Care Med. 2008;36(10):2888–97.
James HE, Macgregor TL, Postlethwait RA, Hofrichter PB, Aldana PR. Advanced registered nurse practitioners and physician assistants in the practice of pediatric neurosurgery: a clinical report. Pediatr Neurosurg. 2011;47(5):359–63.
Moote M, Krsek C, Kleinpell R, Todd B. Physician assistant and nurse practitioner utilization in academic medical centers. Am J Med Qual. 2011;26(6):452–60.
McIntosh N, Meterko M, Burgess JF, Jr, et al. Organizational predictors of coordination in inpatient medicine (In Press). Health Care Managemant Review. 2014.
O’Mahony S, Mazur E, Charney P, Wang Y, Fine J. Use of multidisciplinary rounds to simultaneously improve quality outcomes, enhance resident education, and shorten length of stay. J Gen Intern Med. 2007;22(8):1073–9.
Krein SL, Kowalski CP, Hofer TP, Saint S. Preventing hospital-acquired infections: a national survey of practices reported by u.s. Hospitals in 2005 and 2009. J Gen Intern Med. 2012;27(7):773–9.
VanDeusen LC, Engle RL, Holmes SK, et al. Strengthening organizations to implement evidence-based clinical practices. Health Care Manag Rev. 2010;35(3):235–45.
Dillman D. Mail and internet surveys: The tailored design method (2nd ed.). New York: John Wiley & Sons, Inc; 2000.
Shortell SM. National survey of hospital efforts to improve quality Evanston. IL: Northwestern University; 1995.
The Leapfrog Hospital Survey. 2012; http://leapfroghospitalsurvey.org/web/wp-content/uploads/2012/03/2012Survey.pdf. Accessed June, 20, 2012.
Shwartz M, Cramer IE, Holmes SK, et al. Survey-assessed quality and organizational factors related to quality in Pursuing Perfection hospitals. Qual Manage Health Care. 2010;19(4):349–63.
Doescher M, Skillman S. Rural–urban commuting area codes (RUCAs). http://depts.washington.edu/uwruca/index.php. Accessed December, 2013.
Bowling A. Measuring health: A review of quality of life measurement scales (2nd Edition). Buckingham (UK): Open University; 1997.
Ware JJ, Harris W, Gandek B, Rogers B, Reese P. MAP-R for Windows: Multitrait/Multi-item Analysis Program - Revised User’s Guide. Boston (MA): Health Assessment Lab; 1997.
Campbell D, Fisk D. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychiatr Bull. 1959;56(2):81–105.
Velez-Gonzalez H, Pradhan R, Weech-Maldonado R. The role of non-financial performance measures in predicting hospital financial performance: the case of for-profit system hospitals. J Health Care Finance. 2011;38(2):12–23.
Mennicken R, Kuntz L, Schwierz C. The trade-off between efficiency and quality in hospital departments. J Health Organ Manag. 2011;25(5):564–77.
Huergoa E, Jaumandreu J. Firm’s age, process innovation, and productivity growth. Int J Ind Organ. 2004;22(4):541–59.
Angst CM, Agarwal R, Sambamurthy V, Kelley K. Social contagion and information technology diffusion: the adoption of electronic medical records in U.S. hospitals. Manag Sci. 2010;56(8):1219–41.
Benzer JK, Young GJ, Burgess JF, Jr, et al. Sustainability of Quality Improvement Following Removal of Pay-for-Performance Incentives. J Gen Internal Med. Aug 9 2013.
Werner RM, Bradlow ET. Public reporting on hospital process improvements is linked to better patient outcomes. Health Aff. 2010;29(7):1319–24.
Parker VA, Wubbenhorst WH, Young GJ, Desai KR, Charns MP. Implementing quality improvement in hospitals: the role of leadership and culture. Am J Med Qual. 1999;14(1):64–9.
Restuccia JD, Cohen AB, Horwitt JN, Shwartz M. Hospital implementation of health information technology and quality of care: are they related? BMC Med Inform Decis Mak. 2012;12:109.
Acknowledgements
The work reported here was supported by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (REA 09-220), and the Comprehensive Access & Delivery Research and Evaluation (CADRE) Center at the Iowa City VAMC (HFP 04-149) and the Center for Organizational Leadership and Management Research (COLMR) at the Boston VA Healthcare System (HFP 04-145). We acknowledge and appreciate the intellectual contribution made by Dr. Alan Cohen, Dr. Michael Shwartz and Jed Horwitt who, along with Dr. Restuccia, developed the Quality Improvement Activities Survey from which many of the questions in our survey were drawn. We also wish to thank Dr. Caitlin Brennan and Dr. James Burgess for their careful review of the manuscript and insightful comments. Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Restuccia, J.D., Mohr, D., Meterko, M. et al. The Association of Hospital Characteristics and Quality Improvement Activities in Inpatient Medical Services. J GEN INTERN MED 29, 715–722 (2014). https://doi.org/10.1007/s11606-013-2759-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2759-8