Abstract
Background
Increasing patient cost sharing is a commonly employed mechanism to contain health care expenditures.
Objective
To explore whether the impact of increases in prescription drug copayments differs between high- and low-income areas.
Design
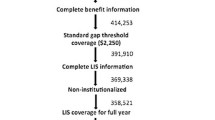
Using a database of 6 million enrollees with employer-sponsored health insurance, econometric models were used to examine the relationship between changes in drug copayments and adherence with medications for the treatment of diabetes mellitus (DM) and congestive heart failure (CHF).
Subjects
Individuals 18 years of age and older meeting prespecified diagnostic criteria for DM or CHF were included.
Measurements
Median household income in the patient’s ZIP code of residence from the 2000 Census was used as the measure of income. Adherence was measured by medication possession ratio: the proportion of days on which a patient had a medication available.
Results
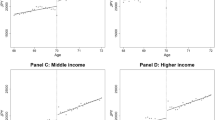
Patients in low-income areas were more sensitive to copayment changes than patients in high- or middle-income areas. The relationship between income and price sensitivity was particularly strong for CHF patients. Above the lowest income category, price responsiveness to copayment rates was not consistently related to income.
Conclusions
The relationship between medication adherence and income may account for a portion of the observed disparities in health across socioeconomic groups. Rising copayments may worsen disparities and adversely affect health, particularly among patients living in low-income areas.


Similar content being viewed by others
References
National Center for Health Statistics. Health, United States, 1998 with Socioeconomic Status and Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 1998.
Rao SV, Kaul P, Newby LK, et al. Poverty, process of care, and outcome in acute coronary syndromes. JACC. 2003;41(11):1948–54.
Lemstra M, Neudorf C, Opondo J. Health disparity by neighbourhood income. Can J Public Health. 2006;97(6):435–9.
Schneeweiss S, Soumerai SB, Glynn RJ, Maclure M, Dormuth C, Walker AM. Impact of reference-based pricing for angiotensin-converting enzyme inhibitors on drug utilization. CMAJ. 2002;166(6):737–45.
Federman AD, Halm EA, Zhu C, Hochman T, Siu AL. Association of income and prescription drug coverage with generic medication use among older adults with hypertension. Am J Manag Care. 2006;12(10):611–8.
Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27(2):384–91.
Claxton G, Gabel J, Gil I, et al. Health benefits in 2006: premium increases moderate, enrollment in consumer-directed health plans remains modest. Health Aff. 2006;25(6):w476–85.
Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291(19):2344–50.
Federman AD, Vladeck BC, Siu AL. Avoidance of health care services because of cost: impact of the medicare savings program. Health Aff. 2005;24(1):263–70.
Rice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004;61(4):415–52.
Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61–9.
Schneeweiss S, Soumerai SB, Glynn RJ, Maclure M, Dormuth C, Walker AM. Impact of reference-based pricing for angiotensin-converting enzyme inhibitors on drug utilization. CMAJ. 2002;166(6):737–45.
Pilote L, Beck C, Richard H, Eisenberg MJ. The effects of cost-sharing on essential drug prescriptions, utilization of medical care and outcomes after acute myocardial infarction in elderly patients. CMAJ. 2002;167(3):246–52.
Hsu J, Price M, Huang J, et al. Unintended consequences of caps on medicare drug benefits. N Eng J Med. 2006;354(22):2349–59.
Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285(4):421–9.
Bryson CL, Au DH, Young B, McDonell MB, Finh SD. A refill adherence algorithm for multiple short intervals to estimate refill compliance (ReComp). Med Care. 2007;45(6):497–504.
Gonnella JS, Lewis DZ, Gozum MV, Callahan CA, Barnes CA. Disease Staging: Clinical Criteria, 5th ed. Ann Arbor, MI: Thomson Medstat; 2005.
Joyce GE, Escarce JJ, Solomon MD, Goldman DP. Employer drug benefit plans and spending on prescription drugs. JAMA. 2002;288(14):1733–9.
Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):455–61.
Gibson TB, Mark TL, McGuigan KA, Axelsen K, Wang S. The effects of prescription drug copayments on statin adherence. Am J Manag Care. 2006;12(9):509–17.
Cole JA, Norman H, Weatherby LB, Walker AM. Drug copayment and adherence in chronic heart failure: effect on cost and outcomes. Pharmacotherapy. 2006;26(8):1157–64.
Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27(12):2800–5.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43(6):521–30.
Gibson TB, McLaughlin CG, Smith DG. A copayment increase for prescription drugs: the long term and short-term effects on use and expenditures. Inquiry. 2005;42(3):293–310.
Taira DA, Wong KS, Frech-Tamas F, Chung RS. Copayment level and compliance with antihypertensive medication: analysis and policy implications for managed care. Am J Manag Care. 2006;12(11):678–83.
Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003;349(23):2224–32.
Soumerai SB, McLaughlin TJ, Ross-Degnan D, Casteris CS, Bollini P. Effects of a limit on Medicaid drug-reimbursement benefits on the use of psychotropic agents and acute mental health services by patients with schizophrenia. N Engl J Med. 1994;331(10):650–5.
Krieger N, Waterman P, Chen JT, Soobader MJ, Subramanian SV, Carson R. Zip code caveat: bias due to spatiotemporal mismatches between ZIP codes and US census-defined geographic areas—the Public Health Disparities Geocoding Project. Am J Pub Health. 2002;92(7):1100–2.
Fendrick AM, Smith DG, Chernew ME, Shah SN. A benefit-based copay for prescription drugs: patient contribution based on total benefits, not drug acquisition cost. Am J Manag Care. 2001;7(9):861–7.
Chernew ME, Rosen AB, Fendrick AM. Value-based insurance design. Health Aff (Millwood). 2007;26(2):w195–203.
Fendrick AM, Chernew ME. Value-based insurance design: a “clinically sensitive, fiscally responsible” approach to mitigate the adverse clinical effects of high-deductible consumer-directed health plans. J Gen Intern Med. 2007;22(6):890–1.
Freudenheim M. To save later, some employers are offering free drugs now. New York Times. February 21, 2007:A1.
Roblin DW, Platt R, Goodman MJ, et al. Effect of increased cost-sharing on oral hypoglycemic use in 5 managed care organizations: how much is too much? Med Care. 2005;43(10):951–959.
Acknowledgments
We thank Amelito Torres for his programming assistance.
Conflict of Interest
This work was supported by financial support from GlaxoSmithKline. At the time of the study, both Dr. Sokol and Dr. Yu-Isenberg were full-time employees of GlaxoSmithKline.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chernew, M., Gibson, T.B., Yu-Isenberg, K. et al. Effects of Increased Patient Cost Sharing on Socioeconomic Disparities in Health Care. J GEN INTERN MED 23, 1131–1136 (2008). https://doi.org/10.1007/s11606-008-0614-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0614-0