Abstract
The study aimed to verify an association between changes in body mass index (BMI) and quality of life (QoL) in a 4-year follow-up in a population-based study in Poland. The results covered data from 1557 adults from the general Polish population who participated in the follow-up survey, performed in two waves: 2011 (COURAGE in Europe); 2015/2016 (COURAGE-POLFUS). Anthropometric measurements and a structured questionnaire including the WHOQOL-AGE scale were used. Regression models were applied to verify whether the observed BMI–QoL association is linear or U-shaped. The inverse U-shaped association between BMI changes and QoL among Polish adults was found using a univariable model. This association was observed in women, whereas in men a linear relationship was found. At the population level, weight loss (BMI decrease of 5–10%) was associated with better QoL in healthy people. The reverse was true in sick people, whose weight loss was observed to be an indicator of poorer QoL. In conclusion, the study suggests an inverse U-shaped association between BMI and quality of life. Better QoL may be considered an additional benefit of public weight loss programs for healthy adults. Further studies focusing on people with some chronic diseases are needed.
Similar content being viewed by others
Introduction
The worldwide epidemic of obesity and overweight is an important public health concern in most high- and middle-income countries, including Poland, and remains an important topic of scholarly investigations (Webber et al. 2014; Hall 2018; Abarca-Gómez et al. 2017). Obesity, as a multidimensional phenomenon, is perceived in various ways in different social and cultural contexts and has been described from different perspectives (Sobal 2001).
From the social perspective, obesity is associated with the culturally created symbolic meaning of ideal body. Social expectations perceive physical appearance as a part of an individual and social identity, which is based on acceptance of body size in relation to beauty (especially in women) and healthy body. Strong influence of healthism and processes of medicalization caused changes in definitions of social norms associated with expected body size and weight (Sobal 2017; Monaghan et al. 2013). Social attitudes to obese or overweight individuals are also indicators of the position of people who do not follow expectations associated with body image. From the public health perspective (related to the biomedical model), obesity and overweight are perceived as a deviant state and as lack of self-control and self-power which leads to stigmatization. Thus, stigmatization of an individual’s obesity and different forms of discrimination are mostly associated with lack of acceptance of the body (Goffman 1963). The fat stigma power is therefore used to motivate individuals to change health-related behaviors, especially nutritional patterns and physical activity. Stigmatizers, however, do not take into account the social costs of such stigmatization—lack of social acceptance, social discrimination, social exclusion, and an increase of social distance between an obese person and normal weight people, or even a risk of social selection based on body mass index. Obese stigmatization, and especially the attitudes to obese persons presented by medical professions, in consequence, could and still can significantly influence all social interactions in public life (Phelan et al. 2014).
From the medical perspective, obesity is perceived as a complex, multifactorial disease, which has an impact on physical functioning and quality of life (Kolotkin et al. 2001; Kolotkin and Andersen 2017). Moreover, overweight and obesity are well-known risk factors for several chronic diseases, such as adult-onset diabetes, high blood pressure, heart disease, stroke, cancer, obstructive sleep apnea, and metabolic syndrome (Lu et al. 2014; Arnold et al. 2017; Youssef and McCullough 2002). Some studies also showed an association between obesity and psychological problems, showing a continuous increase in the risk of lifetime diagnosis of psychiatric disease in people with obesity and a U-shaped association between weight change and depression (Simon et al. 2006; de Wit et al. 2015). Additionally, overweight and obesity increase the risk of hospitalization and death (León-Muñoz et al. 2005). Studies aimed to assess the nature of relationship between obesity and mortality showed an increased risk of death in higher and lower body mass index (BMI) categories, indicating an inverse U- or J-shape relation. On the other hand, there are some studies indicating that overweight can be neutral or even protective against mortality (Aune et al. 2016; Bombak 2014; Orpana et al. 2010; Laxy et al. 2017; Cohen-Mansfield and Perach 2011).
Research regarding association between BMI and quality of life (QoL) showed an inverse linear trend or inverse U-shaped relation, or when BMI was analyzed as a categorical variable, QoL was impaired among people with overweight or obesity (Laxy et al. 2017; Daviglus et al. 2003; Jia and Lubetkin 2005; Ul-Haq et al. 2013). The results varied depending on the dimension of QoL taken into account or the tools of measurement used. It is worth mentioning that most studies published to date employed SF-36 or other commonly used generic measures of QoL/HRQoL, such as PCS-12, MCS-12, EQ-5D index, EQ VAS, or specific instruments measuring obesity-related quality of life, e.g., IWQOL (Ul-Haq et al. 2013). Taking into account the change in weight, a systematic review performed by Kroes et al. showed that in some studies, weight loss was associated with an improvement in physical dimension of QoL more frequently than in the mental one and with an improvement in almost all of obesity-specific IWQOL-Lite subscales. However, the heterogeneity of the studies included in the review precluded drawing unambiguous conclusions (Kroes et al. 2016). Due to several interferences, it is also difficult to presume causality between weight changes and QoL in intervention studies (Kolotkin and Andersen 2017). The majority of studies in this area were randomized control trials investigating results of intervention aimed at weight reduction. Also, as mentioned by Douketis, “studies investigating weight loss have methodologic limitations that restrict the applicability of findings to obese patients assessed in clinical practice” (Douketis et al. 2005). Results of these studies are inconsistent and do not lead to any reasonable conclusions (the changes in QoL were independent from weight loss, or they were probably the result of weight loss, or the relation was unclear) (Carson et al. 2014).
Aim
The study aims to verify the association between changes in BMI and QoL in a 4-year follow-up study in Poland taking into account different sociodemographic and health characteristics in the population.
Methods
Study Design
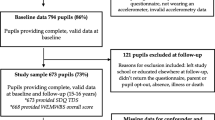
The follow-up survey was performed in two waves. The first was part of the COURAGE in Europe study (Leonardi et al. 2014). The field part of that study took place in 2011. Participants were randomly sampled from a non-institutionalized adult population (18+) based on the multistage clustered design with an oversampling of adults aged 50–79 and > 80. In total, 4071 Polish citizens agreed to participate in the study (the response rate was 66.5%). The second wave, the COURAGE in Europe—follow-up (COURAGE-POLFUS) study—was done in 2015–2016. Overall, 1850 respondents participated in the second wave (the effective response rate was 50%). In both waves, face-to-face interviews were conducted at respondents’ homes by specially trained interviewers. The study was approved by the Bioethical Committee, Jagiellonian University, Krakow, Poland (no. 122.6120.26.2015). The study flow chart is presented in Fig. 1. Data were weighted to generalize the study sample to the reference population. The details are described in the Supplementary file 1.
Measurements
BMI was calculated as weight in kilograms divided by height in meters squared. Weight was measured with a calibrated electronic weighting scale in both waves, whereas height was measured without shoes, using a stadiometer in the first wave only. The changes in BMI were analyzed in two ways: firstly, as a continuous variable calculated as a difference between BMI from the second wave and from the first one; secondly, as a categorical variable based on the percentage of BMI change, in the following five categories: (1) BMI decrease of more than 10%, (2) BMI decrease of 5–10%, (3) BMI change of less than 5%, (4) BMI increase of 5–10%, and (5) BMI increase of more than 10%. To describe the population under study, BMI was categorized as underweight (< 18.50 kg/m2), normal weight (18.50–24.99 kg/m2), overweight (25.00–29.99 kg/m2), obese class I (30.00–34.99 kg/m2), and obese classes II and III (severe obesity) (≥ 35.00 kg/m2).
QoL was assessed by the WHOQOL-AGE scale that consists of 13 items and covers six dimensions such as physical and psychological domains, level of independence, social relationships, environment, and spirituality/ religion/ personal beliefs (THE WHOQOL GROUP 1995). The tool contains items from EUROHIS-QOL (items related to physical, psychological, social relationships, and environment) and WHOQOL-OLD (items related to sensory abilities, autonomy, past, present, and future abilities, social participation, and intimacy) scales and specially adapted for the aging population. The final score ranged from 0 to 100 points. Higher score is interpreted as better health-related quality of life (Caballero et al. 2013).
Covariates
Sociodemographic characteristics (age, sex, level of education, marital status, having children); health-related behaviors (physical activity—categories based on Global Physical Activity Questionnaire (GPAQ), vegetables and fruit consumption—number of servings per day, alcohol consumption, tobacco consumption); and chronic conditions—presence of chronic condition diagnosis—were based on self-reported data. In case of angina, arthritis, asthma, and chronic obstructive pulmonary disease, questions about the presence of symptoms during the past 12 months, the same as those developed for the World Health Survey, were asked. Finally, the prevalence of disease was estimated by an appropriate algorithm taking into account the diagnosis and symptoms (Moussavi et al. 2007). For diabetes, stroke, and cancer, respondents were considered having the disease if they reported being ever diagnosed with those diseases. The question about the diagnosis of cancer was asked only in the second wave. An injury was considered a disease when respondents suffered a physical disability as a result of being injured in the last 12 months. The presence of depression was assessed based on the DSM-IV criteria. For further analysis, respondents were grouped into two categories: a respondent either had any of the aforementioned conditions or had none of them.
Feeling of loneliness was assessed by the three-item UCLA Loneliness Scale (Hughes et al. 2004).
The construct of social networks was measured by the COURAGE Social Network Index (COURAGE-SNI) (Zawisza et al. 2014). The tool assesses structural and functional aspects of individuals’ social network.
Statistical Analysis
A chi-square test or Mann-Whitney U test was performed to see whether there are any significant differences between gender groups in BMI, sociodemographic characteristics, health-related behaviors, and disease characteristics, also in WHOQOL-AGE.
The association between changes in BMI and QoL was analyzed using linear regression models, with linear or linear and quadratic term of BMI changes, to verify whether the relationship is linear or U-shaped. Additionally, the BIC and AIC criteria for model selection were used. All models were weighted and first analyzed unadjusted for age, then adjusted for age, and next adjusted for age and other sociodemographic and health characteristics. Finally, the feeling of loneliness and social networks were added as covariates. Analyses were conducted for the whole sample as well as separately by sex and disease status, and across three age categories (< 50, 50–64, and 65+).
As the next step, logistic regression models were used to verify the relationship between the percentage of BMI change in five categories and poor QoL. QoL was defined as poor when the values of the WHOQOL-AGE scale were lower than the first quartile (coded as 1) and as moderate or good otherwise (coded as 0).
The significance level was set at < 0.05. Two-sided tests were used. The data were analyzed using SAS 9.4.
Results
The basic characteristics of respondents are presented in Table 1. According to the weighted data, the obesity rate among Polish adults was almost 25% (BMI ≥ 30 kg/m2) in 2011 and 2015, including around 5% in 2011 and 7% in 2015 affected with severe obesity. The percentage was greater among males than females (26.4% vs. 23.7% in 2011 and 26.2% vs. 23.3% in 2015). Additionally, the number of adults with overweight increased by about 5 percentage points (around 7 percentage points in men and less than 1 percentage point in women). During the follow-up, the average BMI increased (from median = 26.10 to median = 26.25), especially among men (from median = 26.40 to median = 26.78). The characteristics of the population based on the whole sample of people participating in the first wave are available in Table S1 (Supplementary file 2). Almost 32% of Polish adults surveyed had a university degree (35.6% of women, 29.2% of men), 67.5% were currently married or cohabited, about 11% were lifetime abstainers (14% of women, 7.4% of men), 25% were daily smokers (19% of women, 32% of men), 6.5% had depression, and almost 26% had at least one chronic disease. Females had higher saturation of social networks (at the second wave) and quality of life.
BMI Change–QoL Relationship—Results of Linear Regression Models
The results showed an inverse U-shaped association between changes in BMI and QoL after the follow-up (BIC = 8131.1 for the model with linear term and BIC = 8130.2 for the model with linear and quadratic term—both weighted and unadjusted). After controlling for all considered covariates, the relationship was not found significant.
BMI Change–QoL Relationship—Results of Linear Regression Models in Subgroups
Further investigation in subgroups suggested the inverse U-shaped association in women in models unadjusted and adjusted for age. In men, a linear relationship was observed, where the greatest BMI increase was related not to a lower but a higher level of QoL.
It was also shown among the youngest group, even in a fully adjusted model. Reversely, the inverse linear BMI change–QoL relationship was found among the youngest females.
For people with chronic diseases, the inverse U-shape relationship was also found, but after it was adjusted for health-related behaviors and health and social variables, a linear relationship was identified. In age subgroups, the inverse U-shaped relation was revealed among those with any disease aged from 18 to 49 in an unadjusted model; controlling for other covariates resulted in reversing the U-shape curve. Among healthy people, no significant relationship was observed, and an inverse U-shape relationship was found among the youngest people in a fully adjusted model (Tables 2 and 3) (Table S2 (Supplementary file 2)).
BMI Change–QoL Relationship—Results of Logistic Regression Models
Next we wanted to check whether the BMI change is associated with higher or lower odds of poorer QoL. People whose BMI decreased by about 10% or more during the follow-up had a two times higher chance of poorer QoL compared with people who changed their BMI by less than 5%.
BMI Change–QoL Relationship—Results of Logistic Regression Models in Subgroups
The aforementioned relationship was also observed among females (OR = 2.54), but not among males (p value for interaction with BMI = 0.023). Different relationships among gender groups were also observed in those whose BMI increased during the follow-up. Going into details, men with increased BMI had lower risk of poorer QoL (OR = 0.39 for increasing BMI by 10% or more and OR = 0.55 for increasing it by about 5–10%; in the second case, the results are at the edge of significance: p = 0.051), whereas women had about 2-fold higher odds of having poorer QoL (OR = 1.84 for increasing BMI by about 5–10% and OR = 1.88 for increasing it by 10% or more).
Stratified analyses across disease status showed that a decrease of 5–10% in BMI was related with higher odds of poorer QoL among those diagnosed with any disease (OR = 2.08) but lower odds of poorer QoL among the healthy group (OR = 0.40) (p value for interaction with BMI = 0.023). Decreasing BMI by more than 10% was related to 4-fold higher chance of poorer QoL only among diseased people (OR = 4.13) (Fig. 2).
The assessment of changes in the BMI categories as a determinant of poor QoL measured by WHOQOL-AGE in a 4-year follow-up (COURAGE-POLFUS study—wave 2). The results of the logistic regression models. The observations are weighted; the models are adjusted for baseline demographic characteristics (age, sex, education level, marital status, having children), baseline health behaviors (physical activity, vegetable and fruit consumption, alcohol consumption, tobacco consumption), baseline social variables (social network and loneliness), and diseases diagnosis for both waves (diagnosis of depression, diagnosis of any chronic disease). “No disease” and “Any disease” groups are based on chronic disease or depression diagnosis in the second wave
What BMI Changes Are Linked with the Best QoL?
Assuming an inverse U-shaped association between BMI and QoL at the population level (based on the unadjusted weighted models), the question was about what BMI changes are linked with the best QoL overall and across subgroups (Figs. 3 and 4). For the whole sample, the highest QoL was observed in those who had BMI increased by about 4.14 kg/m2. In females, the highest QoL was noticed among those who increased their BMI by 2.50 kg/m2. Among people who reported at least one disease, an increase in BMI by 5.19 kg/m2 was linked with the highest QoL (Fig. 3).
Results Across Age Groups by Gender
In females, the U-shaped curves in the three age groups studied were quite similar to one another, with the highest QoL for an increase in BMI from 1.51 in the youngest group to 2.74 kg/m2 in the oldest group (statistical significance was found only in the youngest group; for older groups, p value was around 0.065). Among men in the youngest age group, the U-shaped curve was reversed, with the lowest QoL among those whose BMI decreased by 0.66 kg/m2. The relationships between BMI change and QoL were approximately linear in older males with a higher QoL for a greater increase of BMI among men aged 50–64, and a reverse trend (but not significant) was observed for men aged 65+ (Table 2) (Fig. 4).
Results Across Age Groups by Disease Status
Among people diagnosed with any disease, the highest QoL was observed in the case of increasing BMI by about 6 kg/m2 for younger groups and by 1 kg/m2 in the oldest group (65+) (Fig. 4).
Results Across Gender by Disease Status
Additionally, the curves (inverse U-shape) looked very similar among males and females with any of the chronic diseases. At the same time, among healthy females, the inverse U-shape relation was found, with the highest QoL for a decrease in BMI by about 0.7 kg/m2. Reversely, healthy men indicated better QoL for a bigger decrease and increase in BMI (the QoL was minimum for a decrease in BMI by about 0.2 kg/m2) (Figure S1 (Supplementary file 3)).
Discussion
The estimated prevalence and trends observed in changes of the prevalence of obesity in Poland based on our studies were in line with other ones (Webber et al. 2014; WHO 2013).
Our study showed an inverse U-shaped association between changes in BMI and quality of life among Polish adults, in women, not in men, and among people who reported chronic diseases. Controlling for health-related behaviors, the presence of diseases, quality of social networks, and feeling of loneliness did not result in any significant findings, or in the case of ill people, a rather linear relationship was observed.
The inverse U-shape relation between the weight status measured by BMI and the quality of life was found in the US population (Laxy et al. 2017). A similar pattern was observed in the Norwegian population aged 40–49, with changes in BMI measured by self-reported questionnaire and health-related quality of life measured by SF-36 (Hervik Thorbjørnsen et al. 2014).
The results of studies investigating the association between BMI and QoL across gender groups showed a stronger relation in women than in men (Wang et al. 2012). This may be explained by a link between obesity and difficulties in daily living activities, which was found to be stronger in women (Koyanagi et al. 2015). The results of our study also showed a different pattern of relationship between QoL and BMI in men and women, an inverse U-shaped association in females, and a linear association in males, showing better QoL when BMI increased. Thus, it has been suggested that gender might be a modifier of BMI–QoL association.
The modification effect by gender was found in the US population of patients, with greater negative effects of overweight and obesity on quality of life among women than men (Katz et al. 2000). Similar results were obtained in France but with proportionally lower effects mediated by obesity-related conditions (Audureau et al. 2016).
The results of the French cross-sectional study showed that the total effect of obesity and overweight on QoL was more apparent in women. Among men, an indirect effect through obesity-related conditions was observed. This research concluded that women suffer a burden of excess weight due to an interplay of different factors within a psychosocial process, rather than medical conditions (Audureau et al. 2016). There are studies indicating the association between obesity and depression or other psychological disorders and that they are modified by gender. This association was typically observed among women, not in men. Besides, obesity was noticed to decrease the risk of depression in men (Anderson et al. 2006), which may partially explain the linear association in men. In age subgroups, the analysis showed that this result is significant among the youngest men (19–49 years old). The beneficial effect of marriage may be considered a possible explanation, as it increases opportunities for eating and stability in eating patterns and weakens motivation for keeping the body weight down (Jeffery and Rick 2002). On the contrary, there are also studies where the BMI–QoL association was found among both gender groups (Søltoft et al. 2009; Pimenta et al. 2015).
A question emerges—what BMI is associated with the highest QoL? In a study by Laxy et al., the highest QoL was observed among women with BMI at around 22 kg/m2 and among men with BMI in a range of 22–30 kg/m2 (Laxy et al. 2017). In our study, we investigated what change in BMI is reflected in the highest QoL. The result of our study suggests various conclusions depending on gender, age, and disease status. An increase in BMI by 2.50 kg/m2 was observed in females and by 5.19 kg/m2 in people who reported at least one disease. Reversely, it was losing weight that was more likely to be reflected in better QoL in healthy people.
The next condition which may play a role in BMI–QoL association is the health status. Our analyses in the disease status subgroups showed the inverse U-shaped BMI–QoL association in the group “with a chronic disease.” Besides, weight loss (BMI decrease by 5–10%) was associated with better QoL in healthy people, unlike diseased people, whose weight loss was observed to be an indicator of poorer QoL. This suggests BMI may be a proxy measure, which is, especially through physical activity, associated with some QoL dimensions in this group. Other studies showed that the nature of BMI–QoL association varied depending on whether participants were recruited from the general healthy population, from medical outpatient or patient population, or from obesity clinics in particular (Yancy et al. 2002). An investigation by Doll and colleagues showed that obesity is related to a lower level in physical dimensions of QoL, which was stronger in subjects with chronic conditions than in healthy individuals. The decrease in mental dimension of QoL was observed only in obese people with an accompanying disease (Doll et al. 2000). Other studies performed in clinical settings in the USA showed a reverse relation between BMI categories and physical functioning, general health perception, and vitality measured by SF-36. The association was not noticed however for mental functioning (Katz et al. 2000). The differences in the relation between obesity and HRQoL, depending on existing comorbidities, were presented in a review performed by Kolotkin and Andersen (Kolotkin and Andersen 2017). Among outpatients, the study revealed significantly worse physical functioning, bodily pain, and lower vitality among men with obesity types II and III, but regarding mental health, the association was significant for men with overweight and obesity type I only as compared with normal weight participants (Yancy et al. 2002).
In the follow-up, the results of our study showed the highest QoL when BMI increased by about 2.5 kg/m2 in women and when BMI increased by about 5 kg/m2 in those with chronic diseases. Although discussable, it is consistent with the opinion that extra weight may be protective in older age or in the case of people with some diseases (Napoli et al. 2014). It is also not clear whether it is worth to enforce a reduction in body weight by dietary changes in older adults, as they have difficulties in changing health-related behaviors and it was observed that weight loss may increase stress, release persistent organic pollutants, and increase a risk of osteoporosis in this group (Bombak 2014).
Our study has several strengths: Firstly, we have recruited a relatively large representative sample from the general Polish population. Secondly, the BMI–QoL association was investigated in a follow-up. Thirdly, body weight was measured directly in individuals, which avoided the recall bias frequently present in questionnaire-based studies. Fourthly, a set of important covariates, including social networks and the feeling of loneliness, were taken into account. The adjustment for social variables was made because social norms play a key role in the determination of ideal body weight, especially among women.
The study however is not free from some limitations. BMI as a measure of body weight does not distinguish between excess fat, muscle, or bone mass and does not provide information about fat distribution. There was no information about satisfaction with body image which might influence self-assessment of QoL independently from BMI, especially among women. Besides, there was no information about binge eating or about weight and shape concerns. Finally, there was a relatively high percentage of dropouts, which might cause selection bias. Losses to follow-up were caused by deaths among participants in advanced age, who represented a relatively high proportion of the study sample as a result of the oversampling of people aged 80+ at baseline. We believe that selection bias in our study is rather unlikely, as the comparison of individuals who were analyzed (n = 1557) and those who were in the group of dropouts or excluded (n = 2229) showed that there were no differences in sex and quality of life distribution. However, members of the group lost to follow-up were older (medians, 58 for the analyzed and 59 for the excluded; p = 0.003), had slightly lower BMI (medians, 27.1 for the analyzed and 26.6 for the excluded; p = 0.007), and had slightly poorer social network measured by COURAGE-SNI (median, 67.3 for participants and 65.8 for excluded).
In summary:
-
1.
An inverse U-shaped association between changes in BMI and quality of life was found among Polish adults, but adjusting for health-related behaviors, presence of diseases, quality of social networks, and feeling of loneliness resulted in no significant relationship.
-
2.
An inverse U-shaped association was observed in women, whereas a rather positive linear relationship was suggested in men.
-
3.
An inverse U-shaped association was observed in people with a chronic disease.
-
4.
A modification effect by gender and disease status of the BMI change–QoL association was observed.
-
5.
Further investigation is needed to verify these relationships using e.g. other measurements, e.g., waist/hip ratio
References
Abarca-Gómez, L., Abdeen, Z. A., Hamid, Z. A., Abu-Rmeileh, N. M., Acosta-Cazares, B., Acuin, C., Adams, R. J., Aekplakorn, W., Afsana, K., Aguilar-Salinas, C. A., Agyemang, C., Ahmadvand, A., Ahrens, W., Ajlouni, K., Akhtaeva, N., al-Hazzaa, H. M., al-Othman, A. R., al-Raddadi, R., al Buhairan, F., al Dhukair, S., Ali, M. M., Ali, O., Alkerwi, A.’., Alvarez-Pedrerol, M., Aly, E., Amarapurkar, D. N., Amouyel, P., Amuzu, A., Andersen, L. B., Anderssen, S. A., Andrade, D. S., Ängquist, L. H., Anjana, R. M., Aounallah-Skhiri, H., Araújo, J., Ariansen, I., Aris, T., Arlappa, N., Arveiler, D., Aryal, K. K., Aspelund, T., Assah, F. K., Assunção, M. C. F., Aung, M. S., Avdicová, M., Azevedo, A., Azizi, F., Babu, B. V., Bahijri, S., Baker, J. L., Balakrishna, N., Bamoshmoosh, M., Banach, M., Bandosz, P., Banegas, J. R., Barbagallo, C. M., Barceló, A., Barkat, A., Barros, A. J. D., Barros, M. V. G., Bata, I., Batieha, A. M., Batista, R. L., Batyrbek, A., Baur, L. A., Beaglehole, R., Romdhane, H. B., Benedics, J., Benet, M., Bennett, J. E., Bernabe-Ortiz, A., Bernotiene, G., Bettiol, H., Bhagyalaxmi, A., Bharadwaj, S., Bhargava, S. K., Bhatti, Z., Bhutta, Z. A., Bi, H., Bi, Y., Biehl, A., Bikbov, M., Bista, B., Bjelica, D. J., Bjerregaard, P., Bjertness, E., Bjertness, M. B., Björkelund, C., Blokstra, A., Bo, S., Bobak, M., Boddy, L. M., Boehm, B. O., Boeing, H., Boggia, J. G., Boissonnet, C. P., Bonaccio, M., Bongard, V., Bovet, P., Braeckevelt, L., Braeckman, L., Bragt, M. C. E., Brajkovich, I., Branca, F., Breckenkamp, J., Breda, J., Brenner, H., Brewster, L. M., Brian, G. R., Brinduse, L., Bruno, G., Bueno-de-Mesquita, H. B.(.)., Bugge, A., Buoncristiano, M., Burazeri, G., Burns, C., de León, A. C., Cacciottolo, J., Cai, H., Cama, T., Cameron, C., Camolas, J., Can, G., Cândido, A. P. C., Capanzana, M., Capuano, V., Cardoso, V. C., Carlsson, A. C., Carvalho, M. J., Casanueva, F. F., Casas, J. P., Caserta, C. A., Chamukuttan, S., Chan, A. W., Chan, Q., Chaturvedi, H. K., Chaturvedi, N., Chen, C. J., Chen, F., Chen, H., Chen, S., Chen, Z., Cheng, C. Y., Chetrit, A., Chikova-Iscener, E., Chiolero, A., Chiou, S. T., Chirita-Emandi, A., Chirlaque, M. D., Cho, B., Cho, Y., Christensen, K., Christofaro, D. G., Chudek, J., Cifkova, R., Cinteza, E., Claessens, F., Clays, E., Concin, H., Confortin, S. C., Cooper, C., Cooper, R., Coppinger, T. C., Costanzo, S., Cottel, D., Cowell, C., Craig, C. L., Crujeiras, A. B., Cucu, A., D’Arrigo, G., d’Orsi, E., Dallongeville, J., Damasceno, A., Damsgaard, C. T., Danaei, G., Dankner, R., Dantoft, T. M., Dastgiri, S., Dauchet, L., Davletov, K., de Backer, G., de Bacquer, D., de Curtis, A., de Gaetano, G., de Henauw, S., de Oliveira, P. D., de Ridder, K., de Smedt, D., Deepa, M., Deev, A. D., Dehghan, A., Delisle, H., Delpeuch, F., Deschamps, V., Dhana, K., di Castelnuovo, A. F., Dias-da-Costa, J. S., Diaz, A., Dika, Z., Djalalinia, S., Do, H. T. P., Dobson, A. J., Donati, M. B., Donfrancesco, C., Donoso, S. P., Döring, A., Dorobantu, M., Dorosty, A. R., Doua, K., Drygas, W., Duan, J. L., Duante, C., Duleva, V., Dulskiene, V., Dzerve, V., Dziankowska-Zaborszczyk, E., Egbagbe, E. E., Eggertsen, R., Eiben, G., Ekelund, U., el Ati, J., Elliott, P., Engle-Stone, R., Erasmus, R. T., Erem, C., Eriksen, L., Eriksson, J. G., la Peña, J. E. D., Evans, A., Faeh, D., Fall, C. H., Sant’Angelo, V. F., Farzadfar, F., Felix-Redondo, F. J., Ferguson, T. S., Fernandes, R. A., Fernández-Bergés, D., Ferrante, D., Ferrari, M., Ferreccio, C., Ferrieres, J., Finn, J. D., Fischer, K., Flores, E. M., Föger, B., Foo, L. H., Forslund, A. S., Forsner, M., Fouad, H. M., Francis, D. K., Franco, M. . C., Franco, O. H., Frontera, G., Fuchs, F. D., Fuchs, S. C., Fujita, Y., Furusawa, T., Gaciong, Z., Gafencu, M., Galeone, D., Galvano, F., Garcia-de-la-Hera, M., Gareta, D., Garnett, S. P., Gaspoz, J. M., Gasull, M., Gates, L., Geiger, H., Geleijnse, J. M., Ghasemian, A., Giampaoli, S., Gianfagna, F., Gill, T. K., Giovannelli, J., Giwercman, A., Godos, J., Gogen, S., Goldsmith, R. A., Goltzman, D., Gonçalves, H., González-Leon, M., González-Rivas, J. P., Gonzalez-Gross, M., Gottrand, F., Graça, A. P., Graff-Iversen, S., Grafnetter, D., Grajda, A., Grammatikopoulou, M. G., Gregor, R. D., Grodzicki, T., Grøntved, A., Grosso, G., Gruden, G., Grujic, V., Gu, D., Gualdi-Russo, E., Guallar-Castillón, P., Guan, O. P., Gudmundsson, E. F., Gudnason, V., Guerrero, R., Guessous, I., Guimaraes, A. L., Gulliford, M. C., Gunnlaugsdottir, J., Gunter, M., Guo, X., Guo, Y., Gupta, P. C., Gupta, R., Gureje, O., Gurzkowska, B., Gutierrez, L., Gutzwiller, F., Hadaegh, F., Hadjigeorgiou, C. A., Si-Ramlee, K., Halkjær, J., Hambleton, I. R., Hardy, R., Kumar, R. H., Hassapidou, M., Hata, J., Hayes, A. J., He, J., Heidinger-Felso, R., Heinen, M., Hendriks, M. E., Henriques, A., Cadena, L. H., Herrala, S., Herrera, V. M., Herter-Aeberli, I., Heshmat, R., Hihtaniemi, I. T., Ho, S. Y., Ho, S. C., Hobbs, M., Hofman, A., Hopman, W. M., Horimoto, A. R. V. R., Hormiga, C. M., Horta, B. L., Houti, L., Howitt, C., Htay, T. T., Htet, A. S., Htike, M. M. T., Hu, Y., Huerta, J. M., Petrescu, C. H., Huisman, M., Husseini, A., Huu, C. N., Huybrechts, I., Hwalla, N., Hyska, J., Iacoviello, L., Iannone, A. G., Ibarluzea, J. M., Ibrahim, M. M., Ikeda, N., Ikram, M. A., Irazola, V. E., Islam, M., Ismail, A. . S., Ivkovic, V., Iwasaki, M., Jackson, R. T., Jacobs, J. M., Jaddou, H., Jafar, T., Jamil, K. M., Jamrozik, K., Janszky, I., Jarani, J., Jasienska, G., Jelakovic, A., Jelakovic, B., Jennings, G., Jeong, S. L., Jiang, C. Q., Jiménez-Acosta, S. M., Joffres, M., Johansson, M., Jonas, J. B., Jørgensen, T., Joshi, P., Jovic, D. P., Józwiak, J., Juolevi, A., Jurak, G., Jureša, V., Kaaks, R., Kafatos, A., Kajantie, E. O., Kalter-Leibovici, O., Kamaruddin, N. A., Kapantais, E., Karki, K. B., Kasaeian, A., Katz, J., Kauhanen, J., Kaur, P., Kavousi, M., Kazakbaeva, G., Keil, U., Boker, L. K., Keinänen-Kiukaanniemi, S., Kelishadi, R., Kelleher, C., Kemper, H. C. G., Kengne, A. P., Kerimkulova, A., Kersting, M., Key, T., Khader, Y. S., Khalili, D., Khang, Y. H., Khateeb, M., Khaw, K. T., Khouw, I. M. S. L., Kiechl-Kohlendorfer, U., Kiechl, S., Killewo, J., Kim, J., Kim, Y. Y., Klimont, J., Klumbiene, J., Knoflach, M., Koirala, B., Kolle, E., Kolsteren, P., Korrovits, P., Kos, J., Koskinen, S., Kouda, K., Kovacs, V. A., Kowlessur, S., Koziel, S., Kratzer, W., Kriemler, S., Kristensen, P. L., Krokstad, S., Kromhout, D., Kruger, H. S., Kubinova, R., Kuciene, R., Kuh, D., Kujala, U. M., Kulaga, Z., Kumar, R. K., Kunešová, M., Kurjata, P., Kusuma, Y. S., Kuulasmaa, K., Kyobutungi, C., la, Q. N., Laamiri, F. Z., Laatikainen, T., Lachat, C., Laid, Y., Lam, T. H., Landrove, O., Lanska, V., Lappas, G., Larijani, B., Laugsand, L. E., Lauria, L., Laxmaiah, A., Bao, K. L. N., le, T. D., Lebanan, M. A. O., Leclercq, C., Lee, J., Lee, J., Lehtimäki, T., León-Muñoz, L. M., Levitt, N. S., Li, Y., Lilly, C. L., Lim, W. Y., Lima-Costa, M. F., Lin, H. H., Lin, X., Lind, L., Linneberg, A., Lissner, L., Litwin, M., Liu, J., Loit, H. M., Lopes, L., Lorbeer, R., Lotufo, P. A., Lozano, J. E., Luksiene, D., Lundqvist, A., Lunet, N., Lytsy, P., Ma, G., Ma, J., Machado-Coelho, G. L. L., Machado-Rodrigues, A. M., Machi, S., Maggi, S., Magliano, D. J., Magriplis, E., Mahaletchumy, A., Maire, B., Majer, M., Makdisse, M., Malekzadeh, R., Malhotra, R., Rao, K. M., Malyutina, S., Manios, Y., Mann, J. I., Manzato, E., Margozzini, P., Markaki, A., Markey, O., Marques, L. P., Marques-Vidal, P., Marrugat, J., Martin-Prevel, Y., Martin, R., Martorell, R., Martos, E., Marventano, S., Masoodi, S. R., Mathiesen, E. B., Matijasevich, A., Matsha, T. E., Mazur, A., Mbanya, J. C. N., McFarlane, S. R., McGarvey, S. T., McKee, M., McLachlan, S., McLean, R. M., McLean, S. B., McNulty, B. A., Yusof, S. M., Mediene-Benchekor, S., Medzioniene, J., Meirhaeghe, A., Meisfjord, J., Meisinger, C., Menezes, A. M. B., Menon, G. R., Mensink, G. B. M., Meshram, I. I., Metspalu, A., Meyer, H. E., Mi, J., Michaelsen, K. F., Michels, N., Mikkel, K., Miller, J. C., Minderico, C. S., Miquel, J. F., Miranda, J. J., Mirkopoulou, D., Mirrakhimov, E., Mišigoj-Durakovic, M., Mistretta, A., Mocanu, V., Modesti, P. A., Mohamed, M. K., Mohammad, K., Mohammadifard, N., Mohan, V., Mohanna, S., Yusoff, M. F. M., Molbo, D., Møllehave, L. T., Møller, N. C., Molnár, D., Momenan, A., Mondo, C. K., Monterrubio, E. A., Monyeki, K. D. K., Moon, J. S., Moreira, L. B., Morejon, A., Moreno, L. A., Morgan, K., Mortensen, E. L., Moschonis, G., Mossakowska, M., Mostafa, A., Mota, J., Mota-Pinto, A., Motlagh, M. E., Motta, J., Mu, T. T., Muc, M., Muiesan, M. L., Müller-Nurasyid, M., Murphy, N., Mursu, J., Murtagh, E. M., Musil, V., Nabipour, I., Nagel, G., Naidu, B. M., Nakamura, H., Námešná, J., Nang, E. E. K., Nangia, V. B., Nankap, M., Narake, S., Nardone, P., Navarrete-Muñoz, E. M., Neal, W. A., Nenko, I., Neovius, M., Nervi, F., Nguyen, C. T., Nguyen, N. D., Nguyen, Q. N., Nieto-Martínez, R. E., Ning, G., Ninomiya, T., Nishtar, S., Noale, M., Noboa, O. A., Norat, T., Norie, S., Noto, D., Nsour, M. A., O’Reilly, D., Obreja, G., Oda, E., Oehlers, G., Oh, K., Ohara, K., Olafsson, Ö., Olinto, M. T. A., Oliveira, I. O., Oltarzewski, M., Omar, M. A., Onat, A., Ong, S. K., Ono, L. M., Ordunez, P., Ornelas, R., Ortiz, A. P., Osler, M., Osmond, C., Ostojic, S. M., Ostovar, A., Otero, J. A., Overvad, K., Owusu-Dabo, E., Paccaud, F. M., Padez, C., Pahomova, E., Pajak, A., Palli, D., Palloni, A., Palmieri, L., Pan, W. H., Panda-Jonas, S., Pandey, A., Panza, F., Papandreou, D., Park, S. W., Parnell, W. R., Parsaeian, M., Pascanu, I. M., Patel, N. D., Pecin, I., Pednekar, M. S., Peer, N., Peeters, P. H., Peixoto, S. V., Peltonen, M., Pereira, A. C., Perez-Farinos, N., Pérez, C. M., Peters, A., Petkeviciene, J., Petrauskiene, A., Peykari, N., Pham, S. T., Pierannunzio, D., Pigeot, I., Pikhart, H., Pilav, A., Pilotto, L., Pistelli, F., Pitakaka, F., Piwonska, A., Plans-Rubió, P., Poh, B. K., Pohlabeln, H., Pop, R. M., Popovic, S. R., Porta, M., Portegies, M. L. P., Posch, G., Poulimeneas, D., Pouraram, H., Pourshams, A., Poustchi, H., Pradeepa, R., Prashant, M., Price, J. F., Puder, J. J., Pudule, I., Puiu, M., Punab, M., Qasrawi, R. F., Qorbani, M., Bao, T. Q., Radic, I., Radisauskas, R., Rahman, M., Rahman, M., Raitakari, O., Raj, M., Rao, S. R., Ramachandran, A., Ramke, J., Ramos, E., Ramos, R., Rampal, L., Rampal, S., Rascon-Pacheco, R. A., Redon, J., Reganit, P. F. M., Ribas-Barba, L., Ribeiro, R., Riboli, E., Rigo, F., de Wit, T. F. R., Rito, A., Ritti-Dias, R. M., Rivera, J. A., Robinson, S. M., Robitaille, C., Rodrigues, D., Rodríguez-Artalejo, F., del Cristo Rodriguez-Perez, M., Rodríguez-Villamizar, L. A., Rojas-Martinez, R., Rojroongwasinkul, N., Romaguera, D., Ronkainen, K., Rosengren, A., Rouse, I., Roy, J. G. R., Rubinstein, A., Rühli, F. J., Ruiz-Betancourt, B. S., Russo, P., Rutkowski, M., Sabanayagam, C., Sachdev, H. S., Saidi, O., Salanave, B., Martinez, E. S., Salmerón, D., Salomaa, V., Salonen, J. T., Salvetti, M., Sánchez-Abanto, J., Sandjaja, Sans, S., Marina, L. S., Santos, D. A., Santos, I. S., Santos, O., dos Santos, R. N., Santos, R., Saramies, J. L., Sardinha, L. B., Sarrafzadegan, N., Saum, K. U., Savva, S., Savy, M., Scazufca, M., Rosario, A. S., Schargrodsky, H., Schienkiewitz, A., Schipf, S., Schmidt, C. O., Schmidt, I. M., Schultsz, C., Schutte, A. E., Sein, A. A., Sen, A., Senbanjo, I. O., Sepanlou, S. G., Serra-Majem, L., Shalnova, S. A., Sharma, S. K., Shaw, J. E., Shibuya, K., Shin, D. W., Shin, Y., Shiri, R., Siani, A., Siantar, R., Sibai, A. M., Silva, A. M., Silva, D. A. S., Simon, M., Simons, J., Simons, L. A., Sjöberg, A., Sjöström, M., Skovbjerg, S., Slowikowska-Hilczer, J., Slusarczyk, P., Smeeth, L., Smith, M. C., Snijder, M. B., So, H. K., Sobngwi, E., Söderberg, S., Soekatri, M. Y. E., Solfrizzi, V., Sonestedt, E., Song, Y., Sørensen, T. I. A., Soric, M., Jérome, C. S., Soumare, A., Spinelli, A., Spiroski, I., Staessen, J. A., Stamm, H., Starc, G., Stathopoulou, M. G., Staub, K., Stavreski, B., Steene-Johannessen, J., Stehle, P., Stein, A. D., Stergiou, G. S., Stessman, J., Stieber, J., Stöckl, D., Stocks, T., Stokwiszewski, J., Stratton, G., Stronks, K., Strufaldi, M. W., Suárez-Medina, R., Sun, C. A., Sundström, J., Sung, Y. T., Sunyer, J., Suriyawongpaisal, P., Swinburn, B. A., Sy, R. G., Szponar, L., Tai, E. S., Tammesoo, M. L., Tamosiunas, A., Tan, E. J., Tang, X., Tanser, F., Tao, Y., Tarawneh, M. R., Tarp, J., Tarqui-Mamani, C. B., Tautu, O. F., Braunerová, R. T., Taylor, A., Tchibindat, F., Theobald, H., Theodoridis, X., Thijs, L., Thuesen, B. H., Tjonneland, A., Tolonen, H. K., Tolstrup, J. S., Topbas, M., Topór-Madry, R., Tormo, M. J., Tornaritis, M. J., Torrent, M., Toselli, S., Traissac, P., Trichopoulos, D., Trichopoulou, A., Trinh, O. T. H., Trivedi, A., Tshepo, L., Tsigga, M., Tsugane, S., Tulloch-Reid, M. K., Tullu, F., Tuomainen, T. P., Tuomilehto, J., Turley, M. L., Tynelius, P., Tzotzas, T., Tzourio, C., Ueda, P., Ugel, E. E., Ukoli, F. A. M., Ulmer, H., Unal, B., Uusitalo, H. M. T., Valdivia, G., Vale, S., Valvi, D., van der Schouw, Y. T., van Herck, K., van Minh, H., van Rossem, L., van Schoor, N. M., van Valkengoed, I. G. M., Vanderschueren, D., Vanuzzo, D., Vatten, L., Vega, T., Veidebaum, T., Velasquez-Melendez, G., Velika, B., Veronesi, G., Verschuren, W. M. M., Victora, C. G., Viegi, G., Viet, L., Viikari-Juntura, E., Vineis, P., Vioque, J., Virtanen, J. K., Visvikis-Siest, S., Viswanathan, B., Vlasoff, T., Vollenweider, P., Völzke, H., Voutilainen, S., Vrijheid, M., Wade, A. N., Wagner, A., Waldhör, T., Walton, J., Bebakar, W. M. W., Mohamud, W. N. W., Wanderley, R. S., Jr., Wang, M. D., Wang, Q., Wang, Y. X., Wang, Y. W., Wannamethee, S. G., Wareham, N., Weber, A., Wedderkopp, N., Weerasekera, D., Whincup, P. H., Widhalm, K., Widyahening, I. S., Wiecek, A., Wijga, A. H., Wilks, R. J., Willeit, J., Willeit, P., Wilsgaard, T., Wojtyniak, B., Wong-McClure, R. A., Wong, J. Y. Y., Wong, J. E., Wong, T. Y., Woo, J., Woodward, M., Wu, F. C., Wu, J., Wu, S., Xu, H., Xu, L., Yamborisut, U., Yan, W., Yang, X., Yardim, N., Ye, X., Yiallouros, P. K., Yngve, A., Yoshihara, A., You, Q. S., Younger-Coleman, N. O., Yusoff, F., Yusoff, M. F. M., Zaccagni, L., Zafiropulos, V., Zainuddin, A. A., Zambon, S., Zampelas, A., Zamrazilová, H., Zdrojewski, T., Zeng, Y., Zhao, D., Zhao, W., Zheng, W., Zheng, Y., Zholdin, B., Zhou, M., Zhu, D., Zhussupov, B., Zimmermann, E., Cisneros, J. Z., Bentham, J., di Cesare, M., Bilano, V., Bixby, H., Zhou, B., Stevens, G. A., Riley, L. M., Taddei, C., Hajifathalian, K., Lu, Y., Savin, S., Cowan, M. J., Paciorek, C. J., Chirita-Emandi, A., Hayes, A. J., Katz, J., Kelishadi, R., Kengne, A. P., Khang, Y. H., Laxmaiah, A., Li, Y., Ma, J., Miranda, J. J., Mostafa, A., Neovius, M., Padez, C., Rampal, L., Zhu, A., Bennett, J. E., Danaei, G., Bhutta, Z. A., & Ezzati, M. (2017). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. The Lancet., 390, 2627–2642. https://doi.org/10.1016/S0140-6736(17)32129-3.
Anderson, S. E., Cohen, P., Naumova, E. N., & Must, A. (2006). Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Archives of Pediatrics & Adolescent Medicine, 160(3), 285.
Arnold, M., Renehan, A. G., & Colditz, G. A. (2017). Excess weight as a risk factor common to many cancer sites: Words of caution when interpreting meta-analytic evidence. Cancer Epidemiology Biomarkers and Prevention. American Association for Cancer Research. doi, 26, 663–665. https://doi.org/10.1158/1055-9965.EPI-16-0940.
Audureau, E., Pouchot, J., & Coste, J. (2016). Gender-related differential effects of obesity on health-related quality of life via obesity-related comorbidities: a mediation analysis of a French nationwide survey. Circulation. Cardiovascular Quality and Outcomes, 9(3), 246–256.
Aune, D., Sen, A., Prasad, M., Norat, T., Janszky, I., Tonstad, S., et. al. (2016). BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ (Clinical research ed.), 353, i2156.
Bombak, A. (2014). Obesity, health at every size, and public health policy. American Journal of Public Health, 104(2), e60–e67.
Caballero, F., Miret, M., Power, M., Chatterji, S., Tobiasz-Adamczyk, B., Koskinen, S., Leonardi, M., Olaya, B., Haro, J., & Ayuso-Mateos, J. (2013). Validation of an instrument to evaluate quality of life in the aging population: WHOQOL-AGE. Health and Quality of Life Outcomes, 11(1), 177.
Carson, T. L., Hidalgo, B., Ard, J. D., & Affuso, O. (2014). Dietary interventions and quality of life: a systematic review of the literature. Journal of Nutrition Education and Behavior, 46(2), 90–101.
Cohen-Mansfield, J., & Perach, R. (2011). Is there a reversal in the effect of obesity on mortality in old age? Journal of aging research, 2011, 765071.
Daviglus, M. L., Liu, K., Yan, L. L., Pirzada, A., Garside, D. B., Schiffer, L., Dyer, A. R., Greenland, P., & Stamler, J. (2003). Body mass index in middle age and health-related quality of life in older age: the Chicago Heart Association Detection Project in Industry Study. Archives of Internal Medicine, 163(20), 2448–2455.
de Wit, L. M., van Straten, A., Lamers, F., Cuijpers, P., & Penninx, B. W. J. H. (2015). Depressive and anxiety disorders: Associated with losing or gaining weight over 2 years? Psychiatry Research, 227(2–3), 230–237.
Doll, H. A., Petersen, S. E. K., & Stewart-Brown, S. L. (2000). Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obesity Research, 8(2), 160–170.
Douketis, J. D., Macie, C., Thabane, L., & Williamson, D. F. (2005). Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. International Journal of Obesity, 29(10), 1153–1167.
Goffman, E. (1963). Stigma. Englewood Cliffs: Prentice-Hall.
Hall, K. D. (2018). Did the food environment cause the obesity epidemic? Obesity, 26(1), 11–13.
Hervik Thorbjørnsen, G., Riise, T., & Øyen, J. (2014). Bodyweight changes are associated with reduced health related quality of life: the Hordaland Health Study. PLoS One, 9(10), e110173.
Hughes, M. E., Waite, L. J., Hawkley, L. C., & Cacioppo, J. T. (2004). A short scale for measuring loneliness in large surveys results from two population-based studies. Research on Aging, 26(6), 655–672.
Jeffery, R. W., & Rick, A. M. (2002). Cross-sectional and longitudinal associations between body mass index and marriage-related factors. Obesity Research, 10(8), 809–815.
Jia, H., & Lubetkin, E. I. (2005). The impact of obesity on health-related quality-of-life in the general adult US population. Journal of Public Health, 27(2), 156–164.
Katz, D. A., McHorney, C. A., & Atkinson, R. L. (2000). Impact of obesity on health-related quality of life in patients with chronic illness. Journal of General Internal Medicine, 15, 789–796.
Kolotkin, R. L., & Andersen, J. R. (2017). A systematic review of reviews: Exploring the relationship between obesity, weight loss and health-related quality of life. Clinical Obesity, 7(5), 273–289.
Kolotkin, R. L., Meter, K., & Williams, G. R. (2001). Quality of life and obesity. Obesity Reviews, 2(4), 219–229.
Koyanagi, A., Moneta, M. V., Garin, N., Olaya, B., Ayuso-Mateos, J. L., Chatterji, S., Leonardi, M., Sainio, P., Galas, A., & Haro, J. M. (2015). The association between obesity and severe disability among adults aged 50 or over in nine high-income, middle-income and low-income countries: A cross-sectional study. BMJ Open, 5(4), e007313.
Kroes, M., Osei-Assibey, G., Baker-Searle, R., & Huang, J. (2016). Impact of weight change on quality of life in adults with overweight/obesity in the United States: a systematic review. Current Medical Research and Opinion, 32(3), 485–508.
Laxy, M., Teuner, C., Holle, R., & Kurz, C. (2017). The association between BMI and health-related quality of life in the US population: sex, age, and ethnicity matters. International Journal of Obesity, ijo2017252.
Leonardi, M., Chatterji, S., Koskinen, S., Ayuso-Mateos, J. L., Haro, J. M., Frisoni, G., Frattura, L., Martinuzzi, A., Tobiasz-Adamczyk, B., Gmurek, M., Serrano, R., Finocchiaro, C., & on behalf of COURAGE in Europe Project’s Consortium. (2014). Determinants of health and disability in ageing population: the COURAGE in Europe Project (collaborative research on ageing in Europe). Clinical Psychology & Psychotherapy, 21(3), 193–198.
León-Muñoz, L. M., Guallar-Castillón, P., López García, E., Banegas, J. R., Gutiérrez-Fisac, J. L., & Rodríguez-Artalejo, F. (2005). Relationship of BMI, waist circumference, and weight change with use of health services by older adults. Obesity Research, 13(8), 1398–1404.
Lu, Y., Hajifathalian, K., Ezzati, M., Woodward, M., Rimm, E. B., & Danaei, G. (2014). Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: A pooled analysis of 97 prospective cohorts with 1·8 million participants. The Lancet, 383(9921), 970–983.
Monaghan, L. F., Colls, R., & Evans, B. (2013). Obesity discourse and fat politics: Research, critique and interventions. Critical Public Health, 23(3), 249–262.
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & U. B. (2007). Depression, chronic diseases, and decrements in health: results from the World Health Surveys. The Lancet, 370(9590), 851–858.
Napoli, N., Shah, K., Waters, D. L., Sinacore, D. R., Qualls, C., & Villareal, D. T. (2014). Effect of weight loss , exercise , or both on cognition and quality of life in obese older adults. The American Journal of Clinical Nutrition, 100(1), 189–198.
Orpana, H. M., Berthelot, J.-M., Kaplan, M. S., Feeny, D. H., McFarland, B., & Ross, N. A. (2010). BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity, 18(1), 214–218.
Phelan, J. C., Lucas, J. W., Ridgeway, C. L., & Taylor, C. J. (2014). Stigma, status, and population health. Social Science & Medicine, 103, 15–23.
Pimenta, F. B. C., Bertrand, E., Mograbi, D. C., Shinohara, H., & Landeira-Fernandez, J. (2015). The relationship between obesity and quality of life in Brazilian adults. Frontiers in Psychology, 6, 966.
Simon, G. E., Von Korff, M., Saunders, K., Miglioretti, D. L., Crane, P. K., van Belle, G., & Kessler, R. C. (2006). Association between obesity and psychiatric disorders in the US adult population. Archives of General Psychiatry, 63(7), 824–830.
Sobal, J. (2001). Social and cultural influences on obesity. Inteernational Textbook of Obesity, 988707, 305–322.
Sobal, J. (2017). Interpreting weight: The social management of fatness and thinness. Routledge.
Søltoft, F., Hammer, M., & Kragh, N. (2009). The association of body mass index and health-related quality of life in the general population: data from the 2003 Health Survey of England. Quality of Life Research, 18(10), 1293–1299.
Ul-Haq, Z., Mackay, D. F., Fenwick, E., & Pell, J. P. (2013). Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity, 21(3), 322–327.
Wang, R., Wu, M.-J., Ma, X.-Q., Zhao, Y.-F., Yan, X.-Y., Gao, Q., & He, J. (2012). Body mass index and health-related quality of life in adults: a population based study in five cities of China. European Journal of Public Health, 22(4), 497–502.
Webber, L., Halicka, E., Marsh, T., Rtveladze, K., Mcpherson, K., & Brown, M. (2014). Projected incidence of overweight and obesity and related disease incidence across Poland. Central European Journal of Public Health, 22(1), 17–23.
WHO. (2013). Poland - WHO Country Profile. Retrieved February 21, 2018, from http://www.euro.who.int/__data/assets/pdf_file/0020/243317/Poland-WHO-Country-Profile.pdf
Yancy, W. S., Olsen, M. K., Westman, E. C., Bosworth, H. B., & Edelman, D. (2002). Relationship between obesity and health- related quality of life in men. Obesity Research, 10(152), 1057–1064.
Youssef, W., & McCullough, A. J. (2002). Diabetes mellitus, obesity, and hepatic steatosis. Seminars in Gastrointestinal Disease, 13(1), 17–30.
Zawisza, K., Galas, A., Tobiasz-Adamczyk, B., Chatterji, S., Haro, J. M., Miret, M., Koskinen, S., Power, M., & Leonardi, M. (2014). The validity of the instrument to evaluate social network in the ageing population: The collaborative research on ageing in Europe Social Network Index. Clinical Psychology & Psychotherapy, 21(3), 227–241.
Funding
The research leading to these results received funding from the European Community’s Seventh Framework Programme (FP7/2007-2013) under grant agreement number 223071 (COURAGE in Europe), the Polish Ministry for Science and Higher Education grant for an international co-financed project (1277/7PR/ UE/2009/7, 2009-2012), and the Jagiellonian University Medical College grant for the project COURAGE-POLFUS (K/ZDS/005241).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Bioethical Committee, Jagiellonian University, Krakow, Poland (no. 122.6120.26.2015).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zawisza, K., Tobiasz-Adamczyk, B., Galas, A. et al. Changes in Body Mass Index and Quality of Life—Population-Based Follow-up Study COURAGE and COURAGE-POLFUS, Poland. Applied Research Quality Life 16, 501–526 (2021). https://doi.org/10.1007/s11482-019-09776-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-019-09776-3