Abstract
Background
Patients with chronic pancreatitis (CP) have poor quality of life (QOL). Sleep disorders affect QOL when associated with chronic pain and opioid use. Hence patients with CP may have unrecognized sleep disturbances.
Aims
The aim of the study was to evaluate sleep disturbances in CP and its impact on QOL.
Methods
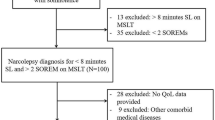
Established CP patients were prospectively enrolled after exclusion of patients with co-morbidities known to negatively affect sleep and QOL. Three questionnaires were used to identify sleep disturbances, PROMISv1SF8, Insomnia Severity Index, and Epworth Sleepiness Scale, and one for restless leg syndrome (RLS). PANQOLI and SF12 questionnaires were used to evaluate QOL. Two blinded sleep pulmonologists evaluated the responses. QOL assessments were then analyzed in patients with and without sleep disturbances.
Results
Of 89 patients, 48 met exclusion criteria, 41 were eligible, and 28 completed the study. Twenty patients (71%) had sleep disturbances with significantly worse scores across all 3 sleep questionnaires and also had lower scores on both PANQOLI (50 vs 76, p = 0.002) and SF-12 (physical component 29.3 vs 53.9, p < 0.001; mental component 36.4 vs 46.1, p = 0.03). Eleven patients (39%) had RLS and sleep disturbances.
Conclusion
In patients with established CP there was a high prevalence of sleep disturbances and RLS with worse QOL representing a potential therapeutic target to improve QOL.

Similar content being viewed by others
References
Hirota M, Shimosegawa T, Masamune A et al (2012) The sixth nationwide epidemiological survey of chronic pancreatitis in Japan. Pancreatology 12:79–84
Hirota M, Shimosegawa T, Masamune A et al (2014) The seventh nationwide epidemiological survey for chronic pancreatitis in Japan: clinical significance of smoking habit in Japanese patients. Pancreatology 14:490–496
Yadav D, Timmons L, Benson JT et al (2011) Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. Am J Gastroenterol 106:2192–2199
Levy P, Barthet M, Mollard BR et al (2006) Estimation of the prevalence and incidence of chronic pancreatitis and its complications. Gastroenterol Clin Biol 30:838–844
Dominguez-Munoz JE, Lucendo A, Carballo LF et al (2014) A Spanish multicenter study to estimate the prevalence and incidence of chronic pancreatitis and its complications. Rev Esp Enferm Dig 106:239–245
Wang LW, Li ZS, Li SD et al (2009) Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas 38:248–254
Gardner TB, Adler DG, Forsmark CE et al (2020) ACG clinical guideline. Am J Gastroenterol 115(3):322–339
Whitcomb DC, Frulloni L, Garg P et al (2016) Chronic pancreatitis: an international draft consensus proposal for a new mechanistic definition. Pancreatology 16(2):218–224
Machicado JD, Amann ST, Anderson MA et al (2017) Quality of life in chronic pancreatitis is determined by constant pain, disability/unemployment, current smoking, and associated co-morbidities. Am J Gastroenterol 112(4):633–642
Amann ST, Yadav D, Barmada MM et al (2013) Physical and mental quality of life in chronic pancreatitis: a case-control study from the North American Pancreatitis Study 2 cohort. Pancreas 42:293–300
Pezzilli R, Morselli-Labate AM, Frulloni L et al (2006) The quality of life in patients with chronic pancreatitis evaluated using the SF-12 questionnaire: a comparative study with the SF-36 questionnaire. Dig Liver Dis 38:109–115
Wehler M, Nichterlein R, Fischer B et al (2004) Factors associated with health-related quality of life in chronic pancreatitis. Am J Gastroenterol 99:138–146
Olesen SS, Juel J, Nielsen AK et al (2014) Pain severity reduces life quality in chronic pancreatitis: implications for design of future outcome trials. Pancreatology 14:497–502
Mokrowiecka A, Pinkowski D, Malecka-Panas E et al (2010) Clinical, emotional and social factors associated with quality of life in chronic pancreatitis. Pancreatology 10:39–46
Han S, Patel B, Min M et al (2018) Quality of life comparison between smokers and non-smokers with chronic pancreatitis. Pancreatology 18(3):269–274. https://doi.org/10.1016/j.pan.2018.02.012
Afolalu EF, Ramlee F, Tang NKY (2018) Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev 39:82–97
Smith MT, Haythornthwaite JA (2004) How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Med Rev 8(2):119–132
Finan PH, Goodin BR, Smith MT (2013) The association of sleep and pain: an update and a path forward. J Pain 14(12):1539–1552
Marshansky S, Mayer P, Rizzo D et al (2018) Sleep, chronic pain, and opioid risk for apnea. Prog Neuropsychopharmacol Biol Psychiatry 87(Pt B):234–244
Mathias JL, Cant ML, Burke ALJ (2018) Sleep disturbances and sleep disorders in adults living with chronic pain: a meta-analysis. Sleep Med 52:198–210
Van Ryswyk E, Antic NA (2016) Opioids and sleep-disordered breathing. Chest 150(4):934–944
Wassef W, DeWitt J, McGreevy K et al (2016) Pancreatitis quality of life instrument: a psychometric evaluation. Am J Gastroenterol 111(8):1177–1186
Fitzsimmons D, Kahl S, Butturini G et al (2005) Symptoms and quality of life in chronic pancreatitis assessed by structured interview and the EORTC QLQ-C30 and QLQ-PAN26. Am J Gastroenterol 100(4):918–926
Löhr JM, Dominguez-Munoz E, Rosendahl J et al (2017) United European gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J 5(2):153–199
Cheatle MD, Foster S, Pinkett A et al (2016) Assessing and managing sleep disturbance in patients with chronic pain. Anesthesiol Clin 34(2):379–393
Buysse DJ, Yu L, Moul DE et al (2010) Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep 33(6):781–792
Full KM, Malhotra A, Crist K et al (2019) Assessing psychometric properties of the PROMIS sleep disturbance scale in older adults in independent-living and continuing care retirement communities. Sleep Health 5(1):18–22
Gagnon C, Bélanger L, Ivers H et al (2013) Validation of the insomnia severity index in primary care. J Am Board Fam Med 26(6):701–710
Morin CM, Belleville G, Bélanger L et al (2011) The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34(5):601–608
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Lapin BR, Bena JF, Walia HK, Moul DE 2018 The Epworth sleepiness scale: validation of one-dimensional factor structure in a large clinical sample. J Clin Sleep Med 14(8):1293-1301. Published 2018 Aug 15. https://doi.org/10.5664/jcsm.7258
Muth CC (2017) Restless Legs Syndrome. JAMA 317(7):780
Ferré S, García-Borreguero D, Allen RP et al (2019) New insights into the neurobiology of restless legs syndrome. Neuroscientist 25(2):113–125. https://doi.org/10.1177/1073858418791763
Ware JE, Kosinski M, Turner-Bowker DM et al (2002) How to score version 2 of the SF 12 health survey with a supplement documenting version 1. Quality Metric Incorporated (Rhode Island) and Health Assessment Lab (Boston, Massachusetts)
Koo BB (2015) Restless leg syndrome across the globe: epidemiology of the restless legs syndrome/Willis-Ekbom disease. Sleep Med Clin 10(3):189–xi
Aul EA, Davis BJ, Rodnitzky RL (1998) The importance of formal serum iron studies in the assessment of restless legs syndrome. Neurology 51(3):912
LeBlanc M, Merette C, Savard J et al (2009) Incidence and risk factors of insomnia in a population-based sample. Sleep 32(8):1027–1037
Krause AJ, Prather AA, Wager TD et al (2019) The pain of sleep loss: a brain characterization in humans. J Neurosci 39(12):2291–2300. https://doi.org/10.1523/JNEUROSCI.2408-18.2018
Huang CT, Chiang RP, Chen CL et al (2014) Sleep deprivation aggravates median nerve injury-induced neuropathic pain and enhances microglial activation by suppressing melatonin secretion. Sleep 37(9):1513-1523. Published 2014 Sep 1. https://doi.org/10.5665/sleep.4002
Knowles S, Swan L, Salzberg M, Castle D et al (2014) Exploring the relationships between health status, illness perceptions, coping strategies and psychological morbidity in a chronic kidney disease cohort. Am J Med Sci 348(4):271–276
Castro-Marrero J, Zaragozá MC, González-Garcia S et al. (2018) Poor self-reported sleep quality and health-related quality of life in patients with chronic fatigue syndrome/myalgic encephalomyelitis. J Sleep Res 27(6):e12703. https://doi.org/10.1111/jsr.12703
Bruyneel M, Sersté T (2018) Sleep disturbances in patients with liver cirrhosis: prevalence, impact, and management challenges. Nat Sci Sleep 10:369–375. Published 2018 Nov 2
Coniglio AC, Mentz RJ (2020) Sleep breathing disorders in heart failure. Heart Fail Clin 16(1):45–51
Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE (2020) Sleep inconsistency and markers of inflammation. Front Neurol 11:1042
Okun ML, Reynolds CF, Buysse DJ, Monk TH, Mazumdar S, Begley A et al (2011) Sleep variability, health-related practices, and inflammatory markers in a community dwelling sample of older adults. Psychosom Med 73:142–50
Donath MY, Meier DT, Böni-Schnetzler M (2019) Inflammation in the pathophysiology and therapy of cardiometabolic disease. Endocr Rev 40(4):1080–1091
Katagiri A, Kato T (2020) Multi-dimensional role of the parabrachial nucleus in regulating pain-related affective disturbances in trigeminal neuropathic pain. J Oral Sci 62:160–164
Kaur S, Saper CB (2019) Neural circuitry underlying waking up to hypercapnia. Front Neurosci 13:401
Hamdaoui M, Ruppert E, Comtet H et al (2018) Restless legs syndrome related to hemorrhage of a thoracic spinal cord cavernoma. J Spinal Cord Med 41:245–247
Türkoglu ŞA, Bolac ES, Yildiz S et al (2021) Presynaptic inhibition in restless legs syndrome. Int J Neurosci 131(3):213–219. https://doi.org/10.1080/00207454.2020.1737048
Meneely S, Dinkins ML, Kassai M et al (2018) Differential dopamine D1 and D3 receptor modulation and expression in the spinal cord of two mouse models of restless legs syndrome. Front Behav Neurosci 12:199
Telles SC, Alves RS, Chadi G (2012) Spinal cord injury as a trigger to develop periodic leg movements during sleep: an evolutionary perspective. Arq Neuropsiquiatr 70:880–884
Möller JC, Oertel WH (2008) Single-question screen for restless legs syndrome. Nat Clin Pract Neurol 4(3):132–3. https://doi.org/10.1038/ncpneuro0736
Collister D, Rodrigues JC, Mazzetti A, Salisbury K, Morosin L, Rabbat C, Brimble KS, Walsh M (2018) Screening questions for the diagnosis of restless legs syndrome in hemodialysis. Clin Kidney J 12(4):559–563
Ferri R, Lanuzza B, Cosentino FI et al (2007) A single question for the rapid screening of restless legs syndrome in the neurological clinical practice. Eur J Neurol 14(9):1016–21
Acknowledgements
Awais Ahmed MD and Ishani Shah are fellows of the Barbara Janson and Arthur Hilsinger Pancreatology Fellowship at Beth Israel Deaconess Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahmed, A., Anand, A.N., Shah, I. et al. Prospective evaluation of sleep disturbances in chronic pancreatitis and its impact on quality of life: a pilot study. Sleep Breath 26, 1683–1691 (2022). https://doi.org/10.1007/s11325-021-02541-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02541-7