Abstract
Purpose
Long-term opioid use for chronic pain has increased, but limited evidence exists on its benefits. Evaluation of long-term benefits in pain is based on patient-reported measures such as health-related quality of life (HRQoL). This study examined the long-term effects of opioid use on HRQoL and its subdomains in patients with back pain or arthritis by comparing opioid users to non-opioid users for three metrics: (1) any opioid use, (2) duration of opioid use, and (3) average daily morphine equivalent dose.
Methods
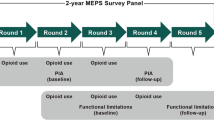
A nationally representative sample of cancer-free adults with chronic back pain or arthritis was selected. Using the 12-Item Short Form Survey, HRQoL measures of Mental Component Score (MCS), Physical Component Score (PCS), and individual subdomains were assessed at baseline and 1 year later. Opioid users were matched to non-opioid users in a 1:1 greedy match using propensity scores estimated based on many patient demographics and baseline HRQoL measures.
Results
At year one, PCS was significantly lower among opioid users, mostly driven by bodily pain subdomain; MCS was not different. Short-term opioid users (< 1 month) had higher MCS while long-term users (≥ 1 month) had lower PCS. Low-dose [< 20 morphine milligram equivalents (MME)/day] opioid use was associated with lower PCS, while no difference was found between high dose (≥ 20 MME/day) and non-opioid users. However, most differences were not clinically significant.
Conclusions
Long-term opioid use is not associated with improvements in HRQoL. Clinicians should carefully evaluate the need for opioid use, especially long-term use in managing chronic back pain and arthritis.




Similar content being viewed by others
References
Hootman, J. M., Helmick, C. G., Barbour, K. E., Theis, K. A., & Boring, M. A. (2016). Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015–2040. Arthritis & Rheumatology (Hoboken, N.J.), 68(7), 1582–1587. https://doi.org/10.1002/art.39692.
Freburger, J. K., Holmes, G. M., Agans, R. P., Jackman, A. M., Darter, J. D., Wallace, A. S., et al. (2009). The rising prevalence of chronic low back pain. Archives of Internal Medicine, 169(3), 251–258. https://doi.org/10.1001/archinternmed.2008.543.
Landsman-Blumberg, P. B., Katz, N., Gajria, K., D’Souza, A. O., Chaudhari, S. L., Yeung, P. P., et al. (2017). Health care resource use and cost differences by opioid therapy type among chronic noncancer pain patients. Journal of Pain Research, 10, 1713–1722. https://doi.org/10.2147/JPR.S130913.
Zamora-Legoff, J. A., Achenbach, S. J., Crowson, C. S., Krause, M. L., Davis, J. M., & Matteson, E. L. (2016). Opioid use in patients with rheumatoid arthritis 2005–2014: A population-based comparative study. Clinical Rheumatology, 35(5), 1137–1144. https://doi.org/10.1007/s10067-016-3239-4.
Wright, E. A., Katz, J. N., Abrams, S., Solomon, D. H., & Losina, E. (2014). Trends in prescription of opioids from 2003 to 2009 in persons with knee osteoarthritis. Arthritis Care & Research, 66(10), 1489–1495. https://doi.org/10.1002/acr.22360.
Mafi, J. N., McCarthy, E. P., Davis, R. B., & Landon, B. E. (2013). Worsening trends in the management and treatment of back pain. JAMA Internal Medicine, 173(17), 1573. https://doi.org/10.1001/jamainternmed.2013.8992.
Chaparro, L. E., Furlan, A. D., Deshpande, A., Mailis-Gagnon, A., Atlas, S., & Turk, D. C. (2014). Opioids compared with placebo or other treatments for chronic low back pain. Spine, 39(7), 556–563. https://doi.org/10.1097/BRS.0000000000000249.
Chou, R., Rick Deyo, F., Beth Devine, M., Ryan Hansen, R., Sullivan, S., Jarvik, J. G., et al. (2014). The effectiveness and risks of long-term opioid treatment of chronic pain. Rockville, MD: Agency for Healthcare Research and Quality (US).
Breivik, H., Borchgrevink, P. C., Allen, S. M., Rosseland, L. A., Romundstad, L., Breivik Hals, E. K., et al.(2008). Assessment of pain. British Journal of Anaesthesia, 101(1), 17–24. https://doi.org/10.1093/bja/aen103.
Katz, N. (2002). The impact of pain management on quality of life. Journal of Pain and Symptom Management, 24(1), S38–S47. https://doi.org/10.1016/S0885-3924(02)00411-6.
Agency for Healthcare Research and Quality. (n.d.). Medical Expenditure Panel Survey background. Retrieved August 10, 2016, from https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
Agency for Healthcare Research and Quality. (n.d.). Medical Expenditure Panel Survey home. Retrieved May 3, 2016, from http://meps.ahrq.gov/mepsweb/.
Medical Expenditure Panel Survey Public Use File Search Results. (n.d.). Retrieved January 11, 2017, from https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=All&cboDataTypeY=1%2CHousehold+Full+Year+File&buttonYearandDataType=Search&cboPufNumber=All&SearchTitle=Medical+Conditions
Multum Source Information. (n.d.). Retrieved from https://www.nlm.nih.gov/research/umls/sourcereleasedocs/current/MMSL/.
Lemke, M. (2015). Prescription opioid use in the U.S. in 2012: Characterizing sustained vs. infrequent use using the medical expenditure panel survey. Retrieved from http://www.lexjansen.com/sesug/2015/182_Final_PDF.pdf.
Stockbridge, E. L., Suzuki, S., & Pagán, J. A. (2015). Chronic pain and health care spending: An analysis of longitudinal data from the Medical Expenditure Panel Survey. Health Services Research, 50(3), 847–870. https://doi.org/10.1111/1475-6773.12263.
IMS Health. (n.d.). IMS LifeLink Health Plan Claims Database: Overview and study design issues. Retrieved November 21, 2015, from http://www.uams.edu/TRI/hsrcore/Lifelink_Health_Plan_Claims_Data_DesignIssues_wcost_April2010%5B1%5D.pdf.
U.S Department of Justice Drug Enforcement Administration Office of Diversion Control. (2014). Rules—2014—Final rule: Rescheduling of hydrocodone combination products from schedule III to schedule II. Retrieved August 11, 2016, from http://www.deadiversion.usdoj.gov/fed_regs/rules/2014/fr0822.htm.
Shah, A., Hayes, C. J., & Martin, B. C. (2017). Characteristics of initial prescription episodes and likelihood of long-term opioid use — United States, 2006–2015. MMWR Morbidity and Mortality Weekly Report, 66(10), 265–269. https://doi.org/10.15585/mmwr.mm6610a1.
Hayes, C. J., Hudson, T. J., Phillips, M. M., Bursac, Z., Williams, J. S., Austin, M. A., et al. (2015). The influence of propoxyphene withdrawal on opioid use in veterans. Pharmacoepidemiology and Drug Safety, 24(11), 1180–1188. https://doi.org/10.1002/pds.3851.
Dowell, D., Haegerich, T. M., & Chou, R. (2016). CDC guideline for prescribing opioids for chronic pain — United States, 2016. MMWR. Recommendations and Reports, 65(1), 1–49. https://doi.org/10.15585/mmwr.rr6501e1er.
Hayes, C., Bhandari, N., Kathe, N., & Payakachat, N. (2017). Reliability and Validity of the medical outcomes study short form-12 version 2 (SF-12v2) in adults with non-cancer pain. Healthcare, 5(2), 22. https://doi.org/10.3390/healthcare5020022.
Ware, J. (2005). How to score version 2 of the SF-12 health survey (with a supplement documenting version 1). Lincoln, RI: QualityMetric Inc.
Cheak-Zamora, N. C., Wyrwich, K. W., & McBride, T. D. (2009). Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Quality of Life Research, 18(6), 727–735. https://doi.org/10.1007/s11136-009-9483-1.
Weblet Importer. (n.d.). Retrieved November 15, 2017, from http://gim.med.ucla.edu/FacultyPages/Hays/utils/sf12v2-1.sas.
Ward, M. M., Guthrie, L. C., & Alba, M. I. (2014). Clinically important changes in short form 36 health survey scales for use in rheumatoid arthritis clinical trials: The impact of low responsiveness. Arthritis Care & Research, 66(12), 1783–1789. https://doi.org/10.1002/acr.22392.
Díaz-Arribas, M. J., Fernández-Serrano, M., Royuela, A., Kovacs, F. M., Gallego-Izquierdo, T., Ramos-Sánchez, M., et al. (2017). Minimal clinically important difference in quality of life for patients with low back pain. SPINE. https://doi.org/10.1097/BRS.0000000000002298.
Escobar, A., Quintana, J. M., Bilbao, A., Aróstegui, I., Lafuente, I., & Vidaurreta, I. (2007). Responsiveness and clinically important differences for the WOMAC and SF-36 after total knee replacement. Osteoarthritis and Cartilage, 15(3), 273–280. https://doi.org/10.1016/j.joca.2006.09.001.
Cohen, J. (1977). Statistical power analysis for the behavioral sciences. New York: Academic Press.
SF-12v2TM Health Survey. (n.d.). Retrieved from http://www.cscc.unc.edu/codi/forms/UNLICOMMSFHSF12ShortFormHealthSurvey03192010.pdf.
Deyo, R. A., Cherkin, D. C., & Ciol, M. A. (1992). Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology, 45(6), 613–619.
Austin, P. C. (2008). Goodness-of-fit diagnostics for the propensity score model when estimating treatment effects using covariate adjustment with the propensity score. Pharmacoepidemiology and Drug Safety, 17(12), 1202–1217. https://doi.org/10.1002/pds.1673.
Austin, P. C. (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46(3), 399–424. https://doi.org/10.1080/00273171.2011.568786.
LaValley, M. P. (2008). Logistic regression. Circulation, 117(18), 2395–2399. https://doi.org/10.1161/CIRCULATIONAHA.106.682658.
Hochberg, Y., & Benjamini, Y. (1990). More powerful procedures for multiple significance testing. Statistics in Medicine, 9(7), 811–818. https://doi.org/10.1002/sim.4780090710.
Whittle, S. L., Richards, B. L., & Buchbinder, R. (2013). Opioid analgesics for rheumatoid arthritis pain. JAMA, 309(5), 485. https://doi.org/10.1001/jama.2012.193412.
Krebs, E. E., Gravely, A., Nugent, S., Jensen, A. C., DeRonne, B., Goldsmith, E. S., et al. (2018). Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain. JAMA, 319(9), 872. https://doi.org/10.1001/jama.2018.0899.
Sites, B. D., Beach, M. L., & Davis, M. A. (2014). Increases in the use of prescription opioid analgesics and the lack of improvement in disability metrics among users. Regional Anesthesia and Pain Medicine, 39(1), 6–12. https://doi.org/10.1097/AAP.0000000000000022.
Bostick, G. P., Toth, C., Carr, E. C. J., Stitt, L. W., Morley-Forster, P., Clark, A. J., et al. (2015). Physical functioning and opioid use in patients with neuropathic pain. Pain Medicine (Malden, Mass.), 16(7), 1361–1368. https://doi.org/10.1111/pme.12702.
Warkentin, L. M., Majumdar, S. R., Johnson, J. A., Agborsangaya, C. B., Rueda-Clausen, C. F., Sharma, A. M., et al. (2014). Weight loss required by the severely obese to achieve clinically important differences in health-related quality of life: Two-year prospective cohort study. BMC Medicine, 12, 175. https://doi.org/10.1186/s12916-014-0175-5.
Parker, S. L., Adogwa, O., Mendenhall, S. K., Shau, D. N., Anderson, W. N., Cheng, J. S., et al. (2012). Determination of minimum clinically important difference (MCID) in pain, disability, and quality of life after revision fusion for symptomatic pseudoarthrosis. The Spine Journal, 12(12), 1122–1128. https://doi.org/10.1016/j.spinee.2012.10.006.
Parker, S. L., Mendenhall, S. K., Shau, D., Adogwa, O., Cheng, J. S., Anderson, W. N., et al. (2012). Determination of minimum clinically important difference in pain, disability, and quality of life after extension of fusion for adjacent-segment disease. Journal of Neurosurgery: Spine, 16(1), 61–67. https://doi.org/10.3171/2011.8.SPINE1194.
Ashworth, J., Green, D. J., Dunn, K. M., & Jordan, K. P. (2013). Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up? Pain, 154(7), 1038–1044. https://doi.org/10.1016/j.pain.2013.03.011.
Dobscha, S. K., Lovejoy, T. I., Morasco, B. J., Kovas, A. E., Peters, D. M., Hart, K., et al. (2016). Predictors of improvements in pain intensity in a national cohort of older veterans with chronic pain. The Journal of Pain, 17(7), 824–835. https://doi.org/10.1016/j.jpain.2016.03.006.
Benyamin, R., Trescot, A. M., Datta, S., Buenaventura, R., Adlaka, R., Sehgal, N., et al. (2008). Opioid complications and side effects. Pain Physician, 11(2 Suppl), S105–S120.
Bartoli, A., Michna, E., He, E., & Wen, W. (2015). Pain intensity and interference with functioning and well-being in subgroups of patients with chronic pain treated with once-daily hydrocodone tablets. Journal of Opioid Management, 11(6), 519–533. https://doi.org/10.5055/jom.2015.0305.
Kea, B., Fu, R., Lowe, R. A., & Sun, B. C. (2016). Interpreting the national hospital ambulatory medical care survey: United States Emergency Department Opioid Prescribing, 2006–2010. Academic Emergency Medicine, 23(2), 159–165. https://doi.org/10.1111/acem.12862.
Funding
Funding was provided by National Institute on Drug Abuse (Grant No. 1T32 DA 022981).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hayes was supported by the Translational Training in Addiction [1T32 DA 022981]. Dr. Payakachat received a research grant from 7-Hybrid Cultivation, an honorarium for service as a paid consultant to Roche Ltd., service as a consultant to CBPartners, and ownership of stock in Pfizer. Drs. Hayes and Li declare that they have no conflict of interest.
Research involving human and animal participants
This article utilizes public-use data from the Agency for Healthcare Research and Quality (AHRQ). Therefore, it does not contain any studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hayes, C.J., Payakachat, N. & Li, C. Evaluation of opioid use among patients with back disorders and arthritis. Qual Life Res 27, 3021–3035 (2018). https://doi.org/10.1007/s11136-018-1941-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1941-1