Abstract
Purpose
Preoperative embolization of radiographically suspected meningiomas is often performed to facilitate tumor resection. Its effects on the subsequent disease course of meningioma patients have not been studied in detail and randomized trials are lacking. The purpose of this study was to explore associations of preoperative meningioma embolization with postoperative outcome.
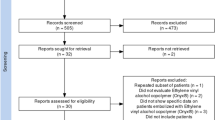
Patients and methods
Patients undergoing resection of an intracranial meningioma at the University Hospital Zurich 2000–2013 (N = 741) were reviewed for the inclusion of pre-operative embolization in the management strategy. Annotations included demographics, radiographic, surgical, histological and hematological parameters, cardiovascular risk factors, pre- and postoperative neurological function and gene methylation-based classification. Binary regression and Cox proportional hazards models were applied to determine factors associated with outcome.
Results
Pre-operative embolization was performed in 337 patients (42%). Cardiovascular events after surgery comprised mostly deep vein thrombosis (N = 39) and pulmonary embolisms (N = 64). On multivariate analyses of post-operative cardiovascular adverse events controlling for established risk factors, there were associations with embolization (OR 2.38, 95% CI 1.37–4.00), and with female gender (OR 2.18, 95% CI 1.17–4.08). Recurrence-free survival (RFS) of embolized patients was less favorable among patients with WHO grade II or grade III meningiomas (median RFS: 4.3 vs. 7.0 years, P = 0.029) or in patients with intermediate or malignant gene methylation subtype meningiomas (median RFS: 2.0 vs. 8.2 years, P = 0.005).
Conclusion
Pre-operative meningioma embolization may cause adverse outcomes. Randomized trials to determine benefit-risk ratios are warranted to clarify the role of pre-operative embolization for the treatment of meningioma patients.


Similar content being viewed by others
References
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2015) CBTRUS Statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol 17(Suppl 4):iv1–iv62. https://doi.org/10.1093/neuonc/nov189
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820. https://doi.org/10.1007/s00401-016-1545-1
Goldbrunner R, Minniti G, Preusser M, Jenkinson MD, Sallabanda K, Houdart E, von Deimling A, Stavrinou P, Lefranc F, Lund-Johansen M, Moyal EC, Brandsma D, Henriksson R, Soffietti R, Weller M (2016) EANO guidelines for the diagnosis and treatment of meningiomas. Lancet Oncol 17(9):e383–e391. https://doi.org/10.1016/s1470-2045(16)30321-7
Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J, Schiff D, Weber DC, Wen PY, Vogelbaum MA (2015) Meningiomas: knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg 122(1):4–23. https://doi.org/10.3171/2014.7.JNS131644
Shah AH, Patel N, Raper DM, Bregy A, Ashour R, Elhammady MS, Aziz-Sultan MA, Morcos JJ, Heros RC, Komotar RJ (2013) The role of preoperative embolization for intracranial meningiomas. J Neurosurg 119(2):364–372. https://doi.org/10.3171/2013.3.jns121328
Singla A, Deshaies EM, Melnyk V, Toshkezi G, Swarnkar A, Choi H, Chin LS (2013) Controversies in the role of preoperative embolization in meningioma management. Neurosurg Focus 35(6):E17. https://doi.org/10.3171/2013.9.FOCUS13351
Perry A, Chicoine MR, Filiput E, Miller JP, Cross DT (2001) Clinicopathologic assessment and grading of embolized meningiomas: a correlative study of 64 patients. Cancer 92(3):701–711
Barresi V, Branca G, Granata F, Alafaci C, Caffo M, Tuccari G (2013) Embolized meningiomas: risk of overgrading and neo-angiogenesis. J Neurooncol 113(2):207–219. https://doi.org/10.1007/s11060-013-1117-3
Wirsching HG, Morel C, Gmur C, Neidert MC, Baumann CR, Valavanis A, Rushing EJ, Krayenbuhl N, Weller M (2016) Predicting outcome of epilepsy after meningioma resection. Neuro Oncol 18(7):1002–1010. https://doi.org/10.1093/neuonc/nov303
Sanai N, Sughrue ME, Shangari G, Chung K, Berger MS, McDermott MW (2010) Risk profile associated with convexity meningioma resection in the modern neurosurgical era. J Neurosurg 112(5):913–919. https://doi.org/10.3171/2009.6.JNS081490
Carrabba G, Riva M, Conte V, Di Cristofori A, Caroli M, Locatelli M, Castellani M, Bucciarelli P, Artoni A, Stocchetti N, Martinelli I, Rampini P (2018) Risk of post-operative venous thromboembolism in patients with meningioma. J Neurooncol 138(2):401–406. https://doi.org/10.1007/s11060-018-2810-z
Karhade AV, Fandino L, Gupta S, Cote DJ, Iorgulescu JB, Broekman ML, Aglio LS, Dunn IF, Smith TR (2017) Impact of operative length on post-operative complications in meningioma surgery: a NSQIP analysis. J Neurooncol 131(1):59–67. https://doi.org/10.1007/s11060-016-2262-2
Hoefnagel D, Kwee LE, van Putten EH, Kros JM, Dirven CM, Dammers R (2014) The incidence of postoperative thromboembolic complications following surgical resection of intracranial meningioma. A retrospective study of a large single center patient cohort. Clin Neurol Neurosurg 123:150–154. https://doi.org/10.1016/j.clineuro.2014.06.001
Levi AD, Wallace MC, Bernstein M, Walters BC (1991) Venous thromboembolism after brain tumor surgery: a retrospective review. Neurosurgery 28(6):859–863
Sahm F, Schrimpf D, Stichel D, Jones DT, Hielscher T, Schefzyk S, Okonechnikov K, Koelsche C, Reuss DE, Capper D, Sturm D, Wirsching HG, Berghoff AS, Baumgarten P, Kratz A, Huang K, Wefers AK, Hovestadt V, Sill M, Ellis HP, Kurian KM, Okuducu AF, Jungk C, Drueschler K, Schick M, Bewerunge-Hudler M, Mawrin C, Seiz-Rosenhagen M, Ketter R, Simon M, Westphal M, Lamszus K, Becker A, Koch A, Schittenhelm J, Rushing EJ, Collins VP, Brehmer S, Chavez L, Platten M, Hanggi D, Unterberg A, Paulus W, Wick W, Pfister SM, Mittelbronn M, Preusser M, Herold-Mende C, Weller M, von Deimling A (2017) DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol. https://doi.org/10.1016/S1470-2045(17)30155-9
Bendszus M, Rao G, Burger R, Schaller C, Scheinemann K, Warmuth-Metz M, Hofmann E, Schramm J, Roosen K, Solymosi L (2000) Is there a benefit of preoperative meningioma embolization? Neurosurgery 47(6):1306–1311; discussion 1311 – 1302
Bendszus M, Monoranu CM, Schutz A, Nolte I, Vince GH, Solymosi L (2005) Neurologic complications after particle embolization of intracranial meningiomas. Am J Neuroradiol 26(6):1413–1419
Nguyen H, Janich K, Doan N, Patel M, Li L, Mueller W (2017) Extent of T1 + C Intensity is a Predictor of Blood Loss in Resection of Meningioma. World Neurosurg. https://doi.org/10.1016/j.wneu.2017.01.098
Borg A, Ekanayake J, Mair R, Smedley T, Brew S, Kitchen N, Samandouras G, Robertson F (2013) Preoperative particle and glue embolization of meningiomas: indications, results and lessons learned from 117 consecutive patients. Neurosurgery. https://doi.org/10.1227/NEU.0b013e31828e1ffd
Chun JY, McDermott MW, Lamborn KR, Wilson CB, Higashida R, Berger MS (2002) Delayed surgical resection reduces intraoperative blood loss for embolized meningiomas. Neurosurgery 50(6):1231–1235; discussion 1235–1237
Fang QR, He XY, Li XF, Zhang X, Chen M, Li H, Li W, Wang ZQ, Duan CZ (2016) Comparative efficacy of Glubran and polyvinyl-alcohol particles in the embolization of meningiomas. Int J Neurosci 126(12):1112–1119. https://doi.org/10.3109/00207454.2015.1134525
Raper DM, Starke RM, Henderson F Jr, Ding D, Simon S, Evans AJ, Jane JA, Liu S KC (2014) Preoperative embolization of intracranial meningiomas: efficacy, technical considerations, and complications. Am J Neuroradiol 35(9):1798–1804. https://doi.org/10.3174/ajnr.A3919
Shah A, Choudhri O, Jung H, Li G (2015) Preoperative endovascular embolization of meningiomas: update on therapeutic options. Neurosurg Focus 38(3):E7. https://doi.org/10.3171/2014.12.FOCUS14728
Eisenring CV, Neidert MC, Sabanes Bove D, Held L, Sarnthein J, Krayenbuhl N (2013) Reduction of thromboembolic events in meningioma surgery: a cohort study of 724 consecutive patients. PLoS ONE 8(11):e79170. https://doi.org/10.1371/journal.pone.0079170
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the regional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. IRB No.: KEK-ZH-2014-0087.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wirsching, HG., Richter, J.K., Sahm, F. et al. Post-operative cardiovascular complications and time to recurrence in meningioma patients treated with versus without pre-operative embolization: a retrospective cohort study of 741 patients. J Neurooncol 140, 659–667 (2018). https://doi.org/10.1007/s11060-018-2996-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2996-0