Abstract
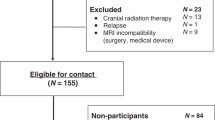
The presence of neurocognitive late effects in survivors of pediatric brain tumors is well established. However, there remains some debate about how best to conceptualize these deficits. Sluggish cognitive tempo (SCT) is a proposed conceptual framework that has been used to describe a subset of children with ADHD who exhibit a particular profile characterized by lethargy, day dreaming and staring, and poor organization. Previous work has suggested that survivors of leukemia exhibit a similar profile, but it has not yet been examined in survivors of pediatric brain tumors. A sample of 65 survivors of pediatric brain tumors, 25 survivors of leukemia and 50 community controls completed the Child Behavior Checklist, with four items used to measure SCT. Survivors completed additional measures of neurocognitive functioning. Survivors of brain tumors demonstrated significantly greater symptoms of SCT than survivors of leukemia or controls. SCT was associated with attention problems and working memory deficits and the presence of a VP-shunt. Results provided conditional support for the presence of SCT in survivors of brain tumors, with further research needed to determine the clinical utility of the framework.
Similar content being viewed by others
References
Robinson KE, Futtesch JF, Champion JE, Andreotti CF, Hipp DW, Bettis A, Barnwell A, Compas BE (2010) A quantitative meta-analysis of neurocognitive sequelae in survivors of pediatric brain tumors. Pediatr Blood Cancer 55:525–531. doi:10.1002/pbc.22568
Maddrey AM, Bergeron JA, Lombardo ER, McDonald NK, Mulne AF, Barenberg PD, Bowers DC (2005) Neuropsychological performance and quality of life of 10 year survivors of childhood medulloblastoma. J Neurooncol 72:245–253. doi:10.1007/s11060-004-3009-z
Zebrack BJ, Gurney JG, Oeffinger K, Whitton J, Packer RJ, Mertens A, Turk N, Castleberry R, Dreyer Z, Robison LL, Zeltzer LK (2004) Psychological outcomes in long-term survivors of childhood brain cancer: a report from the childhood cancer survivors study. J Clin Oncol 22:999–1006. doi:10.1200/JCO.2004.06.148
Kahalley LS, Conklin HM, Tyc VL, Wilson SJ, Hinds PS, Wu S, Xiong X, Hudson MM (2011) ADHD and secondary ADHD criteria fail to identify many at-risk survivors of pediatric ALL and brain tumor. Pediatr Blood Cancer 57:110–118. doi:10.1002/pbc.22998
Bonner MJ, Hardy KK, Willard VW, Gururangan S (2009) Additional evidence of a nonverbal learning disability in survivors of pediatric brain tumors. Child Health Care 38:49–63. doi:10.1080/02739610802615849
Buono LA, Morris MK, Morris RD, Krawiecki N, Norris FH, Foster MA, Copeland DR (1998) Evidence for the syndrome of nonverbal learning disabilities in children with brain tumors. Child Neuropsychol 4:144–157. doi:10.1076/chin.4.2.144.3184
Carey ME, Barakat LP, Foley B, Gyato K, Phillips PC (2001) Neuropsychological functioning and social functioning of survivors of pediatric brain tumors: evidence of a nonverbal learning disability. Child Neuropsychol 7:265–272. doi:0929-7049/01/0704-265
Poggi G, Liscio M, Adduci A, Galbiati S, Massimino M, Sommovigo M, Zettin M, Figini E, Castelli E (2005) Psychological and adjustment problems due to acquired brain lesions in childhood: a comparison between post-traumatic patients and brain tumour survivors. Brain Inj 19:777–785. doi:10.1080/0269905500110132
Butler RW, Copeland DR (2002) Attentional processes and their remediation in children treated for cancer: a literature review and the development of a therapeutic approach. J Int Neuropsychol Soc 8:115–124. doi:10.1017/S1355617702811110
Harrington KM, Waldman ID (2010) Evaluating the utility of sluggish cognitive tempo in discriminating among DSM-IV ADHD subtypes. J Abnorm Child Psychol 38:173–184. doi:10.1007/s10802-009-9355-8
Hartman CA, Willcutt EG, Rhee SH, Pennington BF (2004) The relation between sluggish cognitive tempo and DSM-IV ADHD. J Abnorm Child Psychol 32:491–503. doi:10.1023/B:JACP.0000037779.85211.29
McBurnett K, Pfiffner LJ, Frick PJ (2001) Symptom properties as a function of ADHD type: an argument for continued study of sluggish cognitive tempo. J Abnorm Child Psychol 29:207–213. doi:10.1023/A:1010377530749
Carlson CL, Mann M (2002) Sluggish cognitive tempo predicts a different pattern of impairment in the attention deficit hyperactivity disorder, predominantly inattentive type. J Clin Child Adolesc Psychol 31:123–129. doi:10.1207/153744202753441738
Lee S, Burns GL, Snell J, McBurnett K (in press) Validity of the sluggish cognitive tempo symptom dimension in children: Sluggish cognitive tempo and ADHD-Inattention as distinct symptom dimensions. J Abnorm Child Psychol. doi:10.1007/s10802-013-9714-3
Wåhlstedt C, Bohlin G (2010) DSM-IV-defined inattention and sluggish cognitive tempo: independent and interactive relations to neuropsychological factors and comorbidity. Child Neuropsychol 16:350–365. doi:10.1080/09297041003671176
Barkley RA (2013) Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. J Atten Disord 42:161–173. doi:10.1080/15374416.2012.734259
Meeske KA, Katz ER, Palmer SN, Burwinkle T, Varni JW (2004) Parent proxy-report health-related quality of life and fatigue in pediatric patients diagnosed with brain tumors and acute lymphoblastic leukemia. Cancer 101:2116–2125. doi:10.1002/cncr.20609
Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P (2002) The PedsQL in pediatric cancer: reliability and validity of the pediatric quality of life inventory. Generic Core Scales, Multidimensional Fatigue Scale, and Cancer Module Cancer 94:2090–2106. doi:10.1002/cncr.10428
Kahalley LS, Conklin HM, Tyc VL, Hudson MM, Wilson SJ, Wu S, Xiong X, Hinds PS (in press) Slower processing speed after treatment for pediatric brain tumor and acute lymphoblastic leukemia. Psychooncology. doi:10.1002/pon.3255
Aukema EJ, Caan MW, Oudhuis N, Majoie CB, Vos FM, Reneman L, Last BF, Grootenhuis MA, Schouten-van Meetersen AY (2009) White matter fractional anisotropy correlates with speed of processing and motor speed in young childhood cancer survivors. Int J Radiat Oncol Biol Phys 74:837–843. doi:10.1016/j.ijrobp.2008.08.060
Mulhern RK, Khan RB, Kaplan S, Helton S, Christensen R, Bonner M, Brown R, Xiong X, Wu S, Gururangan S, Reddick WE (2004) Short-term efficacy of methylphenidate: a randomized, double-blind, placebo-controlled trial among survivors of childhood cancer. J Clin Oncol 22:4795–4803. doi:10.1200/JCO.2004.04.128
Reeves CB, Palmer S, Gross AM, Simonian SJ, Taylor L, Willingham E, Mulhern RK (2007) Brief Report: sluggish cognitive tempo among pediatric survivors of acute lymphoblastic leukemia. J Pediatr Psychol 32:1050–1054. doi:10.1093/jpepsy/jsm063
Ellenberg L, Liu Q, Gioia G, Yasui Y, Packer RJ, Mertens A, Donaldson SS, Stovall M, Kadan-Lottick N, Armstrong G, Robison LL, Zeltzer LK (2009) Neurocognitive status in long-term survivors of childhood CNS malignancies: a report from the childhood cancer survivor study. Neuropsychology 23:705–717. doi:10.1037/a0016674
Butler RW, Haser JK (2006) Neurocognitive effects of treatment for childhood cancer. Dev Disabil Res Rev 12:184–191. doi:10.1002/mrdd.20110
Achenbach TM (1991) Manual for the CBCL. University of Vermont, Burlington
Achenbach TM, Rescorla LA (2001) Manual for the ASEBA school-age forms & profiles. University of Vermont, Research Center for Children, Youth & Families, Burlington
Achenbach TM, Rescorla LA (2007) Multicultural supplement to the manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth & Families, Burlington
Wechsler D (2003) Wechsler intelligence scale for children—4th Edition. The Psychological Corporation, San Antonio
Wechsler D (1997) Wechsler adult intelligence scale—3rd edition. The Psychological Corporation, San Antonio
Conklin HM, Krull KR, Reddick WE, Pei D, Cheng C, Pui CH (2012) Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. J Natl Cancer Inst 104:1386–1395. doi:10.1093/jnci/djs344
Jansen NC, Kingma A, Schuitema A, Bouma A, Huisman J, Veerman AJ, Kamps WA (2006) Post-treatment intellectual functioning in children treated for acute lymphoblastic leukaemia (ALL) with chemotherapy-only: a prospective, sibling-controlled study. Eur J Cancer 42:2765–2772. doi:10.1016/j.ejca.2006.06.014
Poggi G, Liscio M, Galbiati S, Adduci A, Massimino M, Gandola L, Spreafico F, Clerici CA, Fossati-Bellanti F, Sommovigo M, Castelli E (2005) Brain tumors in children and adolescents: cognitive and psychological disorders at different ages. Psychooncology 14:386–395. doi:10.1002/pon.85510.1002/pon.855
Duffner PK (2010) Risk factors for cognitive decline in children treated for brain tumors. Eur J Paediatr Neurol 14:106–115. doi:10.1016/j.ejpn.2009.10.005
Hardy KK, Bonner MJ, Willard VW, Watral MA, Gururangan S (2008) Hydrocephalus as a possible additional contributor to cognitive outcome in survivors of pediatric medulloblastoma. Psychooncology 17:1157–1161. doi:10.1002/pon.1349
Becker SP, Luebbe AM, Greening L, Fite PJ, Stoppelbein L (in press) A preliminary investigation of the relation between thyroid functioning and sluggish cognitive tempo in children. J Atten Disord. doi:10.1177/1087054712466917
Merchant TE, Conklin HM, Wu S, Lustig RH, Xiong X (2009) Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol 27:3691–3697. doi:10.1200/JCO.2008.21.2738
Sobol G, Musioł K, Kalina M, Kalina-Faska B, Mizia-Malarz A, Ficek K, Mandera M, Woś H, Małecka-Tendera E (2012) The evaluation of function and the ultrasonographic picture of thyroid in children treated for medulloblastoma. Childs Nerv Syst 28:399–404. doi:10.1007/s00381-011-1625-4
Levisohn L, Cronin-Golomb A, Schmahmann JD (2000) Neuropsychological consequences of cerebellar tumour resection in children: cerebellar cognitive affective syndrome in a paediatric population. Brain 123:1041–1050. doi:10.1093/brain/123.5.1041
Garner AA, Marceaux JC, Mrug S, Patterson C, Hodgens B (2010) Dimensions and correlates of attention deficit/hyperactivity disorder and sluggish cognitive tempo. J Abnorm Child Psychol 38:1097–1107. doi:10.1007/s10802-010-9436-8
Ivanenko A, Tauman RG, Gozal D (2003) Modafinil in the treatment of excessive daytime sleepiness in children. Sleep Med 4:579–582. doi:10.1016/S1389-9457(03)00162-X
Kumar R (2008) Approved and investigational uses of modafinil: an evidence-based review. Drugs 68:1803–1839. doi:0012-6667/08/0013-1803
Kahbazi M, Ghoreishi A, Rahiminejad F, Mohammadi MR, Kamalipour A, Akhondzadeh S (2009) A randomized, double-blind and placebo-controlled trial of modafinil in children and adolescents with attention deficit and hyperactivity disorder. Psychiatry Res 168:234–237. doi:10.1016/j.psychres.2008.06.024
Amiri S, Mohammadi MR, Mohammadi M, Nouroozinejad GH, Kahbazi M, Akhondzadeh S (2008) Modafinil as a treatment for attention-deficit/hyperactivity disorder in children and adolescents: a double blind, randomized clinical trial. Prog Neuropsychopharmacol Biol Psychiatry 32:145–149. doi:10.1016/j.pnpbp.2007.07.025
Biederman J, Pliszka SR (2008) Modafinil improves symptoms of attention-deficit/hyperactivity disorder across subtypes in children and adolescents. J Pediatr 152:394–399. doi:10.1016/j.jpeds.2007.07.052
Lundorff LE, Jønsson BH, Sjøgren P (2009) Modafinil for attentional and psychomotor dysfunction in advanced cancer: a double-blind, randomised, cross-over trial. Palliat Med 23:731–738. doi:10.1177/0269216309106872
Penny A, Waschbusch DA, Klein RM, Corkum P, Eskes G (2009) Developing a measure of sluggish cognitive tempo for children: content validity, factor structure, and reliability. Psychol Assess 21:380–389. doi:10.1037/a0016600
Pfiffner LJ, Yee Mikami A, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K (2007) A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly inattentive type. J Am Acad Child Adolesc Psychiatry 46:1041–1050. doi:10.1097/chi.0b013e318064675f
Jacobson LA, Murphy-Bowman SC, Pritchard AE, Tart-Zelvin A, Zabel TA, Mahone EM (2012) Factor structure of a sluggish cognitive tempo scale in clinically-referred children. J Abnorm Child Psychol 40:1327–1337. doi:10.1007/s10802-012-9643-6
Conflict of interest
The authors have no conflicts of interest or funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Willard, V.W., Hardy, K.K., Allen, T.M. et al. Sluggish cognitive tempo in survivors of pediatric brain tumors. J Neurooncol 114, 71–78 (2013). https://doi.org/10.1007/s11060-013-1149-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-013-1149-8