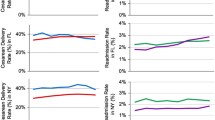
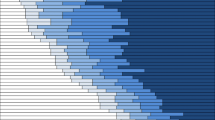
Objective: Because postpartum hemorrhage may result from factors related to obstetrical practice patterns, we examined the variability of postpartum hemorrhage and related risk factors (obstetrical trauma, chorioamnionitis, and protracted labor) across hospital types and hospitals in California. Methods: Linked birth certificate and hospital discharge data from 507,410 births in California in 1997 were analyzed. Cases were identified using International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes. Comparisons were made across hospital types and individual hospitals. Risk adjustments were made using 1) sample restriction to a subset of 324,671 low-risk women, and 2) Bayesian hierarchical logistic regression model to simultaneously quantify the effects of patient-level and hospital-level risk factors. Results: Postpartum hemorrhage complicated 2.4% of live births. The incidence ranged from 1.6% for corporate hospitals to 4.9% for university hospitals in the full sample, and from 1.4% for corporate hospitals to 3.9% for university hospitals in the low-risk sample. Low-risk women who delivered at government, HMO and university hospitals had two- to threefold increased odds (odds ratios 1.98 to 2.71; 95% confidence sets ranged from 1.52 to 4.62) of having postpartum hemorrhage compared to women who delivered at corporate hospitals, irrespective of patient-level characteristics. They also had significantly higher rates of obstetrical trauma and chorioamnionitis. Greater variations were observed across individual hospitals. Conclusion: The incidence of postpartum hemorrhage and related risk factors varied substantially across hospital types and hospitals in California. Further studies using primary data sources are needed to determine whether these variations are related to the processesof care.


Similar content being viewed by others
References
Mousa HA, Walkinshaw S. Major postpartum haemorrhage. Curr Opin Obstet Gynecol 2001;13:595–603.
Bonnar J. Massive obstetric haemorrhage. Baillieres Best Pract Res Clin Obstet Gynaecol 2000;14:1–18.
Combs CA, Murphy EL, Laros RK Jr. Factors associated with postpartum hemorrhage with vaginal birth. Obstet Gynecol 1991;77:69–76.
Combs CA, Murphy EL, Laros RK Jr. Factors associated with hemorrhage in cesarean deliveries. Obstet Gynecol 1991;77:77–82.
American College of Obstetricians and Gynecologists. Postpartum hemorrhage. ACOG Educational Bulletin. Number 243, January 1998.
Casey BM, Cox SM. Chorioamnionitis and endometritis. Infect Dis Clin North Am 1997;11(1):203–22.
Herrchen-Danielsen B, Gould JB. User manual and technical report: Linkage of vital statistics linked birth/infant death, infant, and maternal hospital discharge file. Berkeley: UC Berkeley, 1996.
Herrchen-Danielsen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res 1997;30:290–305.
Office of Statewide Health Planning and Development (OSHPD). California Graduate Medical Education Programs, 1996–1997 update. Sacramento, CA: OSHPD, 1998.
Agency for Healthcare Research and Quality. AHRQ quality indicators—Guide to inpatient quality indicators. Rockville, MD: AHRQ Publication 03-R203, 2003.
Kotelchuck M. An evaluation of the Kessner Adequacy of Prenatal Care Index and a proposed Adequacy of Prenatal Care Utilization Index. Am J Public Health 1994;84:1414–20.
Spiegelhalter DJ, Thomas A, Best NG, Lunn D. WinBUGS: Bayesian inference using Gibbs Sampling for Windows, Version 1.4. Cambridge, UK: MRC Biostatistics Unit, 2003.
Gatsonis CA, Epstein AM, Newhouse JP, Normand SL, McNeil BJ. Variations in the utilization of coronary angiography for elderly patients with an acute myocardial infarction: An analysis using hierarchical logistic regression. Med Care 1995;33:625–42.
Prasertcharoensuk W, Swadpanich U, Lumbiganon P. Accuracy of the blood loss estimation in the third stage of labor. Int J Gynaecol Obstet 2000;71:69–70.
Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: Case-control study. BMJ 2001;322:1089–94.
Hill JA, Fadel HE, Nelson MC, Nelson RM, Nelson GH. Blood loss at vaginal delivery. South Med J 1986;79:188–92.
Donabedian A. Promoting quality through evaluating the process of patient care. Med Care 1968;6:181–202.
ACKNOWLEDGMENTS
Financial support for this work was provided by the California Department of Health Services Maternal and Child Health Branch (Contract No. 01-15166).
Author information
Authors and Affiliations
Corresponding author
Appendices
APPENDIX A: MATERNAL, FETAL, OR PLACENTAL CONDITIONS EXCLUDED FROM THE LOW-RISK SAMPLE
-
Asthma
-
Congenital fetal CNS anomaly or chromosomal abnormality
-
Diabetes or abnormal glucose tolerance
-
Herpes
-
Intrauterine fetal demise
-
Intrauterine growth restriction
-
Macrosomia
-
Malpresentation
-
Maternal cerebral hemorrhage
-
Maternal congenital and other heart disease
-
Maternal hypotension or obstetrical shock
-
Maternal renal abnormalities
-
Maternal soft tissue disorder
-
Maternal thyroid abnormalities
-
Mental disorder
-
Multiple gestation
-
Oligohydramnios
-
Other types of hypertension
-
Polyhyramnios
-
Preterm gestation
-
Pulmonary embolism
-
Severe hypertension: severe pre-eclampsia or eclampsia
-
Uterine rupture
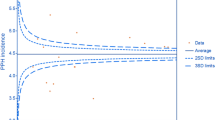
APPENDIX B: BAYESIAN HIERARCHICAL LOGISTIC REGRESSION MODEL USED TO ESTIMATE THE ADJUSTED RATES OF POSTPARTUM HEMORRHAGE, OBSTETRICAL TRAUMA, CHORIOAMNIONITIS, AND PROTRACTED LABOR FOR INDIVIDUAL HOSPITALS
The probability of each of the four events (postpartum hemorrhage, protracted labor, chorioamnionitis, and obstetrical trauma) was modeled using hierarchical logistic regression models. This modeling framework facilitates the analysis of provider variations in outcomes by separating provider-related factors from patient-related ones. The model consists of two equations that are simultaneously estimated, one (patient level) to model within hospital variability, and the other (hospital level) to model between hospital variability. For each dichotomous outcome, the hierarchical logistic regression equations are as follows:
P(Y ij = 1) = P ij is the Bernoulli probability of an event for patient i in hospital j.
-
1.
Patient level equation:
Logit (P ij ) = β 1 j + β 2 j (Age ≥ 35) ij + β 3 j (Poor PNC) ij + β 4 j (Asian) ij + β 5 j (African American) ij + β 7 j (Hispanic) ij + β 8 j (Native American) ij + β 9 j (Nulliparous) ij + β 10 j (Prior CS) ij
Covariates include age, race-ethnicity, parity, prenatal care utilization (10), and prior cesarean delivery. The reference group consists of Caucasian women less than 35 years of age, with adequate or adequate-plus prenatal care, multiparous with no prior cesarean delivery. The beta coefficients from this logistic regression (log-odds scale) measure the effect of patient characteristics on outcome within hospital j. The intercept β 1 j is the baseline (for the reference group) event rate for hospital j and the other β slopes measure the effects of the covariates on outcome.
-
2.
Hospital level equation:
β j is distributed multivariate normal with mean μ and variance–covariance matrix D (bold parameters are multi-dimensional) where,
$$\mu = \gamma _1 + \gamma _2 ({\rm Government})_j + \gamma _3 ({\rm District})_j\\\quad +\, \gamma _4 ({\rm HMO})_j + \gamma _5 ({\rm Not}\;{\rm for}\;{\rm profit})_j \\ \quad +\,\gamma _6 ({\rm UC})_j + \gamma _7 ({\rm Other}\;{\rm hospital}\;{\rm covariates}\;\\\qquad {\rm such}\; {\rm as}\;{\rm OB}\;{\rm teaching}\;{\rm status})_j$$
Covariates for the hospital-level equation include indicator variables for hospital ownership and OB teaching status. The intercept γ 1 is a reference parameter representing corporate hospitals (none of which are obstetrics teaching hospitals).
We assume that the hospital-specific parameter β j is a multivariate normal variate with mean μ that is linearly related to the hospital characteristics. The components of μ are therefore hospital class expectations given the class characteristics. The γ's are parameters common to all hospitals, measuring the effect of hospital characteristics on the expected hospital class rate of outcome. In other words, the components of γ link between hospital characteristics and hospital-specific effects. While the β j are directly related to the patient covariates, the γ's are directly related to hospital level covariates. Note that not only mean hospital rate of outcomes (β intercepts) may vary by hospital characteristics but also β slopes are allowed to vary by hospital characteristics.
The model was estimated under a Bayesian framework that assigns prior probability distributions to all unknown parameters (specifically to γ and D). Posterior distributions of the model parameters (conditional on the data) were derived using Markov Chain Monte Carlo methodology. For each outcome a single Gibbs sampler string was used for inference, implemented using the WinBUGS software (5), with a burn-in of 1000 iterations and a further 2000 iteration used for inference. Starting values for parameters were calculated using logistic regression models. Estimated posterior means for odd ratios are reported with significance determined using 95% confidence sets.
Rights and permissions
About this article
Cite this article
Lu, M.C., Fridman, M., Korst, L.M. et al. Variations in the Incidence of Postpartum Hemorrhage Across Hospitals in California. Matern Child Health J 9, 297–306 (2005). https://doi.org/10.1007/s10995-005-0009-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-005-0009-3