Abstract
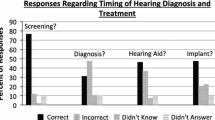
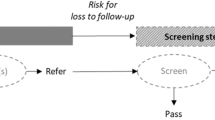
Infant hearing loss has the potential to cause significant communication impairment. Timely diagnosis and intervention is essential to preventing permanent deficits. Many infants from rural regions are delayed in diagnosis and treatment of hearing loss. The purpose of this study is to characterize the barriers in timely infant hearing healthcare for rural families following newborn newborn hearing screening (NHS) testing. Using stratified purposeful sampling, the study design involved semi-structured phone interviews with parents/guardians of children who failed NHS testing in the Appalachian region of Kentucky between 2012 and 2014 to describe their experiences with early hearing detection and intervention program. Thematic qualitative analysis was performed on interview transcripts to identify common recurring themes in content. 40 parents/guardians participated in the study and consisted primarily of mothers. Demographic data revealed limited educational levels of the participants and 70 % had state-funded insurance coverage. Participants reported barriers in timely infant hearing healthcare that included poor communication of hearing screening results, difficulty in obtaining outpatient testing, inconsistencies in healthcare information from primary care providers, lack of local resources, insurance-related healthcare delays, and conflict with family and work responsibilities. Most participants expressed a great desire to obtain timely hearing healthcare for their children and expressed a willingness to use resources such as telemedicine to obtain that care. There are multiple barriers to timely rural infant hearing healthcare. Minimizing misinformation and improving access to care are priorities to prevent delayed diagnosis and treatment of hearing loss.
Similar content being viewed by others
References
Centers for Disease Control and Prevention. National Center on Birth Defects and Developmental Disabilities. Hearing loss. http://www.cdc.gov/ncbddd/dd/ddhi.htm.
Muse, C., Harrison, J., Yoshinaga-Itano, C., Grimes, A., Brookhouser, P. E., Epstein, S., et al. (2013). Supplement to the JCIH 2007 position statement: Principles and guidelines for early intervention after confirmation that a child is deaf or hard of hearing. Pediatrics, 131(4), e1324–e1349.
Bush, M., Hardin, B., Rayle, C., Lester, C., Studts, C., & Shinn, J. (2015). Rural barriers to early diagnosis and treatment of infant hearing loss in Appalachia. Otology and Neurotology, 36(1), 93–98.
Bush, M. L., Bianchi, K., Lester, C., Shinn, J. B., Gal, T. J., Fardo, D. W., et al. (2014). Delays in diagnosis of congenital hearing loss in rural children. The Journal of pediatrics., 164(2), 393–397.
Yoshinaga-Itano, C., Sedey, A. L., Coulter, D. K., & Mehl, A. L. (1998). Language of early- and later-identified children with hearing loss. Pediatrics, 102(5), 1161–1171.
Preventive, U. S. (2008). Services task force. Universal screening for hearing loss in newborns: US preventive services task force recommendation statement. Pediatrics, 122(1), 143–148.
American Academy of Pediatrics JCoIH. (2007). Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatrics, 120(4), 898–921.
Bush, M. L., Osetinsky, M., Shinn, J. B., Gal, T. J., Ding, X., Fardo, D. W., et al. (2014). Assessment of Appalachian region pediatric hearing healthcare disparities and delays. The Laryngoscope, 124(7), 1713–1717.
Nelson, H. D., Bougatsos, C., & Nygren, P. (2008). Force USPST. Universal newborn hearing screening: Systematic review to update the 2001 US preventive services task force recommendation. Pediatrics, 122(1), e266–e276.
Moeller, M. P. (2000). Early intervention and language development in children who are deaf and hard of hearing. Pediatrics, 106(3), e43.
Bush, M. L., Burton, M., Loan, A., & Shinn, J. B. (2013). Timing discrepancies of early intervention hearing services in urban and rural cochlear implant recipients. Otology and Neurotology, 34(9), 1630–1635.
Appalachian Regional Commission. The Appalachian Region. http://www.arc.gov/appalachian_region/TheAppalachianRegion.asp. Accessed February 27, 2015.
Blackley, D., Behringer, B., & Zheng, S. (2012). Cancer mortality rates in Appalachia: Descriptive epidemiology and an approach to explaining differences in outcomes. Journal of Community Health, 37(4), 804–813.
Lengerich, E., Wyatt, S., Rubio, M., Beaulieu, J., Coyne, C., Fleisher, L., et al. (2004). The Appalachia cancer network: Cancer control research among a rural, medically underserved population. The Journal of Rural Health, 20(2), 181–187.
Yao, N., Lengerich, E. J., & Hillemeier, M. M. (2012). Breast cancer mortality in Appalachia: Reversing patterns of disparity over time. Journal of Health Care for the Poor and Underserved, 23(2), 715–725.
Rural-Urban Continuum Codes. USDA Economic Research Service. U.S. Department of Agriculture. http://www.ers.usda.gov/data-products/ruralYurban-continuum-codes.aspx. Accessed December 4, 2014.
Bush, M. L., Alexander, D., Noblitt, B., Lester, C., Shinn, J. B. (2015). Pediatric hearing healthcare in Kentucky’s Appalachian primary care setting. Journal of Community Health, 40(4), 762–768.
McCarthy, M., Munoz, K., & White, K. R. (2010). Teleintervention for infants and young children who are deaf or hard-of-hearing. Pediatrics, 126(Suppl 1), S52–S58.
Acknowledgments
This work was supported by the National Center for Advancing Translational Sciences (University of Kentucky Physician-Mentored Student Research Fellowship—UL1TR000117 (JE)) and KL2 Career Development Program—8 KL2 TR000116-02) (MLB), Triological Society Career Development Award (MLB), and National Institute of Deafness and Other Communication Disorders (1U24-DC012079-01 and 1K23DC014074-01A1)(MLB).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elpers, J., Lester, C., Shinn, J.B. et al. Rural Family Perspectives and Experiences with Early Infant Hearing Detection and Intervention: A Qualitative Study. J Community Health 41, 226–233 (2016). https://doi.org/10.1007/s10900-015-0086-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-015-0086-1