Abstract
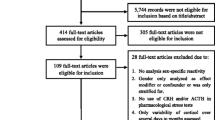
Population-based studies have been hampered in exploring hypothalamic–pituitary–adrenal axis (HPA) activity as a potential explanatory link between stress-related and metabolic disorders due to their lack of incorporation of reliable measures of chronic cortisol exposure. The purpose of this review is to summarize current literature on the reliability of HPA axis measures and to discuss the feasibility of performing them in population-based studies. We identified articles through PubMed using search terms related to cortisol, HPA axis, adrenal imaging, and reliability. The diurnal salivary cortisol curve (generated from multiple salivary samples from awakening to midnight) and 11 p.m. salivary cortisol had the highest between-visit reliabilities (r = 0.63–0.84 and 0.78, respectively). The cortisol awakening response and dexamethasone-suppressed cortisol had the next highest between-visit reliabilities (r = 0.33–0.67 and 0.42–0.66, respectively). Based on our own data, the inter-reader reliability (rs) of adrenal gland volume from non-contrast CT was 0.67–0.71 for the left and 0.47–0.70 for the right adrenal glands. While a single 8 a.m. salivary cortisol is one of the easiest measures to perform, it had the lowest between-visit reliability (R = 0.18–0.47). Based on the current literature, use of sampling multiple salivary cortisol measures across the diurnal curve (with awakening cortisol), dexamethasone-suppressed cortisol, and adrenal gland volume are measures of HPA axis tone with similar between-visit reliabilities which likely reflect chronic cortisol burden and are feasible to perform in population-based studies.


Similar content being viewed by others
Abbreviations
- ACTH:
-
Adrenocorticotrophic hormone
- ARIC:
-
Atheroslerosis Risk In Communities Study
- AUC:
-
Area under the curve
- BMI:
-
Body mass index
- CAR:
-
Cortisol awakening response
- CBG:
-
Corticotrophin binding globulin
- CRH:
-
Corticotrophin releasing hormone
- CT:
-
Computed tomography
- HPA:
-
Hypothalamic–pituitary–adrenal axis
- ICC (R):
-
Intraclass correlation coefficient
- MESA:
-
Multi-Ethnic Study Atherosclerosis
- MRI:
-
Magnetic resonance imaging
- R:
-
Pearson’s linear correlation coefficient
- rs :
-
Spearman’s ordinal correlation coefficient
- UFC:
-
Urine free cortisol
References
McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904.
Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35:2–16.
Rugulies R. Depression as a predictor for coronary heart disease. A review and meta-analysis. Am J Prev Med. 2002;23:51–61.
Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31:2383–90.
Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Roux AV, Lee HB, Lyketsos C. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–9.
Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev. 2007;3:252–9.
Szklo M, Nieto FJ. Quality assurance and control. Epidemiology beyond the Basics. Sudbury: Jones and Bartlett Publishers; 2004. pp. 343–404.
Derr RL, Cameron SJ, Golden SH. Pre-analytic considerations for the proper assessment of hormones of the hypothalamic-pituitary axis in epidemiological research. Eur J Epidemiol. 2006;21:217–26.
Hellhammer DH, Wust S, Kudielka BM. Salivary cortisol as a biomarker in stress research. Psychoneuroendocrinology. 2009;34:163–71.
Raff H. Utility of salivary cortisol measurements in Cushing’s syndrome and adrenal insufficiency. J Clin Endocrinol Metab. 2009;94:3647–55.
Groschl M, Rauh M. Influence of commercial collection devices for saliva on the reliability of salivary steroids analysis. Steroids. 2006;71:1097–100.
Garde AH, Hansen AM. Long-term stability of salivary cortisol. Scand J Clin Lab Invest. 2005;65:433–6.
Levine A, Zagoory-Sharon O, Feldman R, Lewis JG, Weller A. Measuring cortisol in human psychobiological studies. Physiol Behav. 2007;90:43–53.
Broderick JE, Arnold D, Kudielka BM, Kirschbaum C. Salivary cortisol sampling compliance: comparison of patients and healthy volunteers. Psychoneuroendocrinology. 2004;29:636–50.
Badrick E, Kirschbaum C, Kumari M. The relationship between smoking status and cortisol secretion. J Clin Endocrinol Metab. 2007;92:819–24.
Granger DA, Hibel LC, Fortunato CK, Kapelewski CH. Medication effects on salivary cortisol: tactics and strategy to minimize impact in behavioral and developmental science. Psychoneuroendocrinology. 2009;34:1437–48.
Coste J, Strauch G, Letrait M, Bertagna X. Reliability of hormonal levels for assessing the hypothalamic-pituitary-adrenocortical system in clinical pharmacology. Br J Clin Pharmacol. 1994;38:474–9.
Harris TO, Borsanyi S, Messari S, Stanford K, Cleary SE, Shiers HM, Brown GW, Herbert J. Morning cortisol as a risk factor for subsequent major depressive disorder in adult women. Br J Psychiatr. 2000;177:505–10.
Viardot A, Huber P, Puder JJ, Zulewski H, Keller U, Muller B. Reproducibility of nighttime salivary cortisol and its use in the diagnosis of hypercortisolism compared with urinary free cortisol and overnight dexamethasone suppression test. J Clin Endocrinol Metab. 2005;90:5730–6.
Masserini B, Morelli V, Bergamaschi S, Ermetici F, Eller-Vainicher C, Barbieri AM, Maffini MA, Scillitani A, Ambrosi B, Beck-Peccoz P, Chiodini I. The limited role of midnight salivary cortisol levels in the diagnosis of subclinical hypercortisolism in patients with adrenal incidentaloma. Eur J Endocrinol. 2009;160:87–92.
Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, Kaspers F, Kirschbaum C. Free cortisol levels after awakening: a reliable biological marker for the assessment of adrenocortical activity. Life Sci. 1997;61:2539–49.
Edwards S, Clow A, Evans P, Hucklebridge F. Exploration of the awakening cortisol response in relation to diurnal cortisol secretory activity. Life Sci. 2001;68:2093–103.
Kraemer HC, Giese-Davis J, Yutsis M, O’Hara R, Neri E, Gallagher-Thompson D, Taylor CB, Spiegel D. Design decisions to optimize reliability of daytime cortisol slopes in an older population. Am J Geriatr Psychiatr. 2006;14:325–33.
Ranjit N, Diez-Roux AV, Sanchez B, Seeman T, Shea S, Shrager S, Watson K. Association of salivary cortisol circadian pattern with cynical hostility: multi-ethnic study of atherosclerosis. Psychosom Med. 2009;71:748–55.
Hruschka DJ, Kohrt BA, Worthman CM. Estimating between- and within-individual variation in cortisol levels using multilevel models. Psychoneuroendocrinology. 2005;30:698–714.
Knutsson U, Dahlgren J, Marcus C, Rosberg S, Bronnegard M, Stierna P, Albertsson-Wikland K. Circadian cortisol rhythms in healthy boys and girls: relationship with age, growth, body composition, and pubertal development. J Clin Endocrinol Metab. 1997;82:536–40.
Schmidt-Reinwald A, Pruessner JC, Hellhammer DH, Federenko I, Rohleder N, Schurmeyer TH, Kirschbaum C. The cortisol response to awakening in relation to different challenge tests and a 12-hour cortisol rhythm. Life Sci. 1999;64:1653–60.
Arnaldi G, Angeli A, Atkinson AB, Bertagna X, Cavagnini F, Chrousos GP, Fava GA, Findling JW, Gaillard RC, Grossman AB, Kola B, Lacroix A, Mancini T, Mantero F, Newell-Price J, Nieman LK, Sonino N, Vance ML, Giustina A, Boscaro M. Diagnosis and complications of Cushing’s syndrome: a consensus statement. J Clin Endocrinol Metab. 2003;88:5593–602.
Ljung T, Andersson B, Bengtsson BA, Bjorntorp P, Marin P. Inhibition of cortisol secretion by dexamethasone in relation to body fat distribution: a dose-response study. Obes Res. 1996;4:277–82.
Huizenga NA, Koper JW, de Lange P, Pols HA, Stolk RP, Grobbee DE, de Jong FH, Lamberts SW. Interperson variability but intraperson stability of baseline plasma cortisol concentrations, and its relation to feedback sensitivity of the hypothalamo-pituitary-adrenal axis to a low dose of dexamethasone in elderly individuals. J Clin Endocrinol Metab. 1998;83:47–54.
Golden SH, Malhotra S, Wand GS, Brancati FL, Ford D, Horton K. Adrenal gland volume and dexamethasone-suppressed cortisol correlate with total daily salivary cortisol in African-American women. J Clin Endocrinol Metab. 2007;92:1358–63.
Yanovski SZ, Yanovski JA, Gwirtsman HE, Bernat A, Gold PW, Chrousos GP. Normal dexamethasone suppression in obese binge and nonbinge eaters with rapid weight loss. J Clin Endocrinol Metab. 1993;76:675–9.
Wingenfeld K, Lange W, Wulff H, Berea C, Beblo T, Saavedra AS, Mensebach C, Driessen M. Stability of the dexamethasone suppression test in borderline personality disorder with and without comorbid PTSD: a one-year follow-up study. J Clin Psychol. 2007;63:843–50.
Reynolds RM, Bendall HE, Whorwood CB, Wood PJ, Walker BR, Phillips DI. Reproducibility of the low dose dexamethasone suppression test: comparison between direct plasma and salivary cortisol assays. Clin Endocrinol (Oxf). 1998;49:307–10.
Gozansky WS, Lynn JS, Laudenslager ML, Kohrt WM. Salivary cortisol determined by enzyme immunoassay is preferable to serum total cortisol for assessment of dynamic hypothalamic–pituitary–adrenal axis activity. Clin Endocrinol (Oxf). 2005;63:336–41.
Harris B, Watkins S, Cook N, Walker RF, Read GF, Riad-Fahmy D. Comparisons of plasma and salivary cortisol determinations for the diagnostic efficacy of the dexamethasone suppression test. Biol Psychiatr. 1990;27:897–904.
Imaki T, Naruse M, Takano K. Adrenocortical hyperplasia associated with ACTH-dependent Cushing’s syndrome: comparison of the size of adrenal glands with clinical and endocrinological data. Endocr J. 2004;51:89–95.
Rubin RT, Phillips JJ, Sadow TF, McCracken JT. Adrenal gland volume in major depression. Increase during the depressive episode and decrease with successful treatment. Arch Gen Psychiatr. 1995;52:213–8.
Cooper MS, Stewart PM. Diagnosis and treatment of ACTH deficiency. Rev Endocr Metab Disord. 2005;6:47–54.
Klose M, Lange M, Kosteljanetz M, Poulsgaard L, Feldt-Rasmussen U. Adrenocortical insufficiency after pituitary surgery: an audit of the reliability of the conventional short synacthen test. Clin Endocrinol (Oxf). 2005;63:499–505.
Rubin RT, Phillips JJ, McCracken JT, Sadow TF. Adrenal gland volume in major depression: relationship to basal and stimulated pituitary-adrenal cortical axis function. Biol Psychiatr. 1996;40:89–97.
Amsterdam JD, Marinelli DL, Arger P, Winokur A. Assessment of adrenal gland volume by computed tomography in depressed patients and healthy volunteers: a pilot study. Psychiatr Res. 1987;21:189–97.
Brauckhoff M, Stock K, Stock S, Lorenz K, Sekulla C, Brauckhoff K, Thanh PN, Gimm O, Spielmann RP, Dralle H. Limitations of intraoperative adrenal remnant volume measurement in patients undergoing subtotal adrenalectomy. World J Surg. 2008;32:863–72.
Grant LA, Napolitano A, Miller S, Stephens K, McHugh SM, Dixon AK. A pilot study to assess the feasibility of measurement of adrenal gland volume by magnetic resonance imaging. Acta Radiol. 2010;51:117–20.
Anagnostis P, Athyros VG, Tziomalos K, Karagiannis A, Mikhailidis DP. Clinical review: the pathogenetic role of cortisol in the metabolic syndrome: a hypothesis. J Clin Endocrinol Metab. 2009;94:2692–701.
Greden JF, Gardner R, King D, Grunhaus L, Carroll BJ, Kronfol Z. Dexamethasone suppression tests in antidepressant treatment of melancholia. The process of normalization and test-retest reproducibility. Arch Gen Psychiatr. 1983;40:493–500.
Holsboer F, Liebl R, Hofschuster E. Repeated dexamethasone suppression test during depressive illness. Normalisation of test result compared with clinical improvement. J Affect Disord. 1982;4:93–101.
Heuser I, Yassouridis A, Holsboer F. The combined dexamethasone/CRH test: a refined laboratory test for psychiatric disorders. J Psychiatr Res. 1994;28:341–56.
Kunzel HE, Binder EB, Nickel T, Ising M, Fuchs B, Majer M, Pfennig A, Ernst G, Kern N, Schmid DA, Uhr M, Holsboer F, Modell S. Pharmacological and nonpharmacological factors influencing hypothalamic-pituitary-adrenocortical axis reactivity in acutely depressed psychiatric in-patients, measured by the Dex-CRH test. Neuropsychopharmacology. 2003;28:2169–78.
Acknowledgments
This review and accompanying studies were supported by the National Institute of Diabetes, Digestive, and Kidney Diseases, National Institutes of Health (K23 DK071565 to SHG) and by the National Institute of Alcohol Abuse and Alcoholism (RO1 AA10158 to GW).
Author information
Authors and Affiliations
Corresponding author
Appendix: medline search strategy
Appendix: medline search strategy
“Salivary cortisol”[tiab] OR “Daytime cortisol”[tiab] OR “morning cortisol”[tiab] OR “Awakening cortisol”[tiab] OR “Free cortisol”[tiab] OR “diurnal cortisol”[tiab] OR “cortisol”[ti] OR “cortisol response”[ti] OR “Cortisol levels”[tiab] OR “Cortisol rhythms”[tiab] OR “Cortisol rhythm”[tiab] OR “Cortisol secretion”[tiab] OR “Dexamethasone”[ti] OR “hydrocortisone”[tiab] OR “adrenocorticotropic hormone”[tiab] OR “Saliva/chemistry”[majr] OR “Saliva/drug effects”[majr] OR “adrenocortical stress capacity”[All Fields] OR “magnetic resonance imaging”[tiab] AND (“Adrenal Gland Volume”[tiab] OR “adrenal insufficiency”[tiab] OR “Adrenocortical Insufficiency”[tiab] OR “Adrenocorticotropic hormone deficiency”[All] OR “ACTH deficiency”[tiab] OR “Adrenocortical Hyperplasia”[tiab] OR “adrenocortical activity”[tiab] OR “adrenal incidentaloma”[tiab] OR “Adrenalectomy”[tiab] OR “Hypercortisolism”[tiab] OR “Cushing’s syndrome”[tiab] OR “Hypothalamic Pituitary Adrenal Axis”[tiab] OR “Hypothalamic pituitary axis”[tiab] OR “Hypothalamic pituitary adrenocortical system”[tiab] OR “pituitary adrenal cortical axis”[tiab] OR “Hypothalamo-pituitary-adrenal axis”[tiab] OR “hypothalamus–pituitary–adrenal axis”[tiab] OR “hypothalamo-pituitary-adrenal”[tiab] OR “major depression”[ti] OR “depressive illness”[ti] OR “major depressive disorder”[ti] OR “depressed”[ti] OR “antidepressant treatment”[ti] OR “salivary cortisol”[ti] OR “reliability”[ti] OR “cortisol response”[ti]) AND (“humans”[MeSH Terms] AND English[lang] AND “adult”[MeSH Terms] AND (“1982”[PDAT] : “2010/06/30”[PDAT])) NOT review[ptyp].
Rights and permissions
About this article
Cite this article
Golden, S.H., Wand, G.S., Malhotra, S. et al. Reliability of hypothalamic–pituitary–adrenal axis assessment methods for use in population-based studies. Eur J Epidemiol 26, 511–525 (2011). https://doi.org/10.1007/s10654-011-9585-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-011-9585-2