Abstract
Background
Psychological distress is highly noticeable among caregivers working in residential youth care (RYC). Maintaining and enhancing caregivers’ professional mental health and quality of life is crucial to achieve effective outcomes in RYC. Nevertheless, trainings to protect caregivers’ mental health are scarce. Considering the buffering effect over negative psychological outcomes, compassion training could be beneficial in RYC.
Objective
This study is part of a Cluster Randomized Trial examining the effects of the Compassionate Mind Training for Caregivers (CMT-Care Homes), looking at professional quality of life and mental health of caregivers working in RYC.
Method
The sample was composed of 127 professional caregivers from 12 Portuguese residential care homes (RCH). RCHs were randomly allocated at experimental (N = 6) and control group (N = 6). Participants were assessed at baseline, post-treatment, and 3 and 6-month follow-ups, answering to the Professional Quality of Life Scale and the Depression, Anxiety and Stress Scale. Program effects were tested using a two-factor mixed MANCOVA, with self-critical attitude and education degree as covariates.
Results
MANCOVA showed a significant Time × Group interaction effects (F = 1.890, p = .014; \({\eta }_{p}^{2}\) = .050), with CMT-Care Homes participants presenting lower scores on burnout, anxiety, and depression at 3 and 6-months follow-ups, when compared with controls. Participants that received CMT-Care Homes considered the program useful to deal with pandemic threats and with youth during lockdowns.
Conclusion
This study shows the benefits of the CMT-Care Homes in helping professional caregivers reducing burnout, anxiety and depression, and dealing with pandemic challenges in RYC.
Trial registration: This cluster randomized trial was registered at ClinicalTrials.gov (TRN: NCT04512092) on 6th August 2020.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Residential youth care (RYC) is an alternative care response to youth with prior history of maltreatment, aiming to offer them a chance to have a healthy development and shape their future (Quality4Children, 2007). Research demonstrates that the resilience of those who suffer trauma can be enhanced if they are connected to a caring and responsive caregiver (Larkin et al., 2012).
Caregivers have a key role within RYC settings (Li & Julian, 2012; Santos et al., 2023c). Nevertheless, they face many challenges linked to the target group and working conditions, that might threaten both the quality of care and the relationships established not only with children but also among co-workers (Colton & Roberts, 2007; McElvaney & Tatlow-Golden, 2016). Specifically, caregivers are required to actively listen to youth previous experiences and, at the same time, they are expected to soothe them, offer counselling, and care without being overwhelmed by their own emotional responses (Pfaff et al., 2017). Caregivers have to deal with highly traumatized youth, frequently presenting mental health difficulties, while having to cope with episodes of aggression and disruptive behaviors (McElvaney & Tatlow-Golden, 2016). At the same time, they are expected to meet the complex needs and ensure the well-being of children and youth under their care (Barford & Whelton, 2010; Steinlin et al., 2017). Additionaly, working conditions are often poor and the care system frequently does not offer appropiate responses considereing the youth intervention needs (McElvaney & Tatlow-Golden, 2016). On the one hand, the high number of youths under care usually contributes to long hours of work which, combined with shifts, set the base for excessive workloads. On the other hand, the opportunities offered for professional and financial rewards are usually scarce for professionals working within these settings (Colton & Roberts, 2007). The lack of support among colleagues and also by the organization management, as well as communication barriers between professionals, have also been reported as a matter of concern (Del Valle et al., 2007; McElvaney & Tatlow-Golden, 2016).
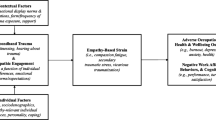
The repeated exposure to emotional pain, in multiple stressful care situations, may lead caregivers to feel frustration, helplessness, and powerlessness, as well as to perceive the job as resulting in greater distress than satisfaction (Colton & Roberts, 2007; McElvaney & Tatlow-Golden, 2016; Stamm, 2010). As a result, caregivers are prone to experience stress, burnout, secondary traumatic stress (STS), anxiety, and depression (Barford & Whelton, 2010; Bürgin et al., 2020; Del Valle et al., 2007; Hermon & Chahla, 2019; Raskin et al., 2015; Santos et al., 2022a; Steinlin et al., 2017). Such conditions may lead to diminished care, loss of interest in others, negative attitudes towards work, and reduced personal accomplishment (Maslach et al., 2001), limiting both the ability to establish empathic relationships and the emotional availability to care (Bride et al., 2007). Besides affecting the quality of care (Steinlin et al., 2017), such condition may also lead to turnover, which is a common problem within RYC (Colton & Roberts, 2007), with negative consequences to the consistency of interventions (Barford & Whelton, 2010).
In addition to the multiple abovementioned work stressors, during the Covid-19 pandemic, residential care homes (RCH) were required to quickly adapt to the public health measures (e.g., lockdowns, closures of schools) and social distancing (Carvalho et al., 2022). As “frontline workers”, while dealing with the risk of becoming infected, professional caregivers had to ensure the provision of care, maintain daily routines as much as possible, and reassure children and youth, who also could be experiencing some psychological disturbance (Ravens-Sieberer et al., 2020). Hence, professionals had to take care of a more stressed group, with even less resources (due to isolations, medical discharges; Whitt-Woosley et al., 2022). These challenges, combined with uncertainty, resulted in additional fears, worries, and stress (Carvalho et al., 2022).
Altogether, the above-mentioned demands reinforce the need to offer proper training to support caregivers in high-stress work environments, as it is the case of RYC (Barford & Whelton, 2010; McElvaney & Tatlow-Golden, 2016). Although some studies tried to overcome this need, some limitations still persist: (1) existing research showed that interventions didn’t had the expected impact (Donald, 2015; Silva & Gaspar, 2014; Vallejos et al., 2016); (2) when positive effects on stress and related syndromes were reached, those studies presented methodological limitations, such as small sample size, lack of randomization and/or absence of control group (Hidalgo et al., 2016; Schmid et al., 2020; Turner, 2017; van Gink et al., 2018); (3) programs were specifically tailored to babies homes (St. Petersburg–USA Orphanage Research Team, 2008). Some trauma-informed approaches also addressed staff mental health. Yet, they also showed some limitations linked to implementation and evaluation (Raymond, 2020).
Compassion-based interventions have been delivered in organizations (Andersson et al., 2022) and in different caring-focused settings, showing a potential to improve care quality, strengthen relationships with clients, protect against burnout, and increase professionals’ well-being (Boellinghaus et al., 2014; Delaney, 2018; Maratos et al., 2019; Matos et al., 2022a; Sansó et al., 2017). This kind of interventions aim to cultivate compassion towards the self and towards others. Compassion can be defined as a motivation to be responsive to one´s own and others suffering and to act in order to alleviate or prevent it (Gilbert, 2020). It may occur in three interactive flows, involving giving compassion to others, receiving compassion from others, and being self-compassionate (Gilbert, 2019). Each of these flows may reveal associated fears, blocks and/or resistances (Gilbert et al., 2011).
Within helping settings, cultivating compassion towards others may facilitate the ‘self-other’ distinction, in order not to absorb others’ suffering or negative emotions as ours own (Vachon, 2016). In other words, if caregivers respond to youth’s suffering with compassion, they will empathize with the suffering, but not identify themselves with it; thus, they will be able to better regulate their own negative affect (Singer & Klimecki, 2014). Hence, compassion can be seen as an emotion-regulation strategy that regulates negative affect (Preckel et al., 2018) and protects against stress (Matos et al., 2017), and mental health problems (Irons & Heriot-Maitland, 2020; Kirby et al., 2017).
Also, relevant to helping professionals is the fact that individuals who give care to others, but do not seek care from others, reveal some difficulties in self-compassion and self-reassurance (Hermanto & Zuroff, 2016). Professionals who lack self-compassion, and particularly those expressing a higher self-critical attitude, are more susceptible to burnout as a result of continuously caring for others, while ignoring their own emotional needs (Gracia-Gracia & Oliván-Blázquez, 2017). In addition, those who lack self-compassion are not only more self-critical, but also more critical and controlling towards others (Gilbert et al., 2011), which may compromise both the establishment of secure relationships as the provision of appropriate care. Self-compassion involves relating to oneself with care and concern when facing hardship or perceived inadequacy (Neff, 2003), and it has been linked to increased well-being (Barnard & Curry, 2011), and lower levels of psychopathology, including anxiety and depression (Ferrari et al., 2019; MacBeth & Gumley, 2012; Wilson et al., 2019). At a professional level, self-compassion can help in coping with uncertain and challenging conditions, resulting in increased job satisfaction and professional well-being, as well as less burnout, depression, anxiety, and stress (Andersson et al., 2022; Babenko et al., 2019). Considering that self-care has been associated with caregivers’ quality of life (Sansó et al., 2015) and higher self-confidence as a caregiver (Bratt et al., 2019), motivating these professionals and raising their awareness on the need to care for their own well-being seems essential.
This study is part of a Cluster Randomized Trial (CRT) aiming to test the effectiveness of the Compassionate Mind Training for Caregivers (CMT-Care Homes) working within RYC settings in several compassion related variables (Santos et al., 2022b, 2023b). It expands compassion-based approaches to RYC settings. It tests the effectiveness of a new training program specifically designed for RYC staff, based in a well-established therapeutic model and practices, resorting to a CRT in a real-world setting. In the current work, the effects of the CMT-Care Homes will be investigated on caregivers’ professional quality of life and mental health symptoms, also investigating whether observed changes after program completion are sustained across time. It responds to the gaps reported in recent systematic reviews about the scarcity of evidence-based and manualized programs to protect and enhance the mental health of RYC professionals, who work in a highly stressful and emotionally demanding setting (Santos et al., 2023a). Considering that caregivers are key agents of change in RYC, this program may contribute to improve the care practices and to reach better outcomes for children and youth placed in RYC, by providing support to those who have been given the responsibility to help these youth to heal and thrive.
The main research questions of this study are: (1) How does the CMT-Care Homes impacts Professional Quality of life and Mental Health symptoms among caregivers working in RYC settings? (2) Are the effects of CMT-Care Homes in these variables sustained across time? Considering that the pandemic situation started during the current CRT, secondary questions are: (1) Was the CMT-Care Homes useful to deal with the pandemic situation? (2) Was the CMT-Care Homes useful to deal with children and youth within RCHs during lockdowns? In accordance with previous research testing compassion-based approaches in helping settings (Matos et al., 2022a; Sansó et al., 2017), it is hypothesized that the CMT-Care Homes will produce significant improvements in burnout, STS, depression, anxiety, and stress, as well as an increase in compassion satisfaction, when comparing caregivers who received the training with those in the control group. In addition, it is expected that the effects of attending the CMT-Care Homes will be maintained at 3 and 6-month follow-ups (Ferrari et al., 2019; Irons & Heriot-Maitland, 2020; Matos et al., 2022a).
Method
This cluster randomized trial followed the standards of Consort 2010 statement: Extension to cluster randomized trials (Campbell et al., 2012). The current study was approved by the Ethics Committee of the Faculty of Psychology and Educational Sciences from the University of Coimbra (CEDI22.03.2018) and its procedures were in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The authors have no competing interests to declare that are relevant to the content of this article.
Participants
This study was carried out between 2019 and 2020 in 12 Portuguese residential care homes (RCH). The following cluster eligibility criteria were considered: (1) RCHs that receive youths aged between 12 and 25 years old, located in the center region of Portugal were included; (2) RCHs specialized in mental and behavioral disorders and/or substance abuse problems were excluded, because they adopt different and specific intervention models. Within the selected RCHs, caregivers who were directly involved in the delivery of services to youth on a regular basis were invited to collaborate.
A total of 127 professional caregivers accepted to participate. Randomization took place at the cluster level, after baseline. Six RCHs were allocated to the treatment group (66 caregivers; 52%), and six RCHs were allocated to the control group (61 subjects; 48%). From the six RCHs allocated to the treatment group, four RCHs were mixed and two received only females, accommodating from 15 to 45 children and youth. These RCHs had between 10 and 21 professionals with different roles. The six RCHs of the control group accommodated from 15 to 40 children and youth, four were mixed and two were gender specific, one for females, and the other one for males. These RCHs had between 14 and 23 professionals with different roles. All RCHs included in this study were 24/7 open group homes (e.g., youth attend local public schools, they are integrated in community sports, and visit their families), they are located in urban and rural areas on the center of Portugal mainland, and receive mostly nationwide children and youth referred by the child protection services. In Portugal, RCHs have the main goal of time-limited protection of youth at-risk, aiming to ensure their safety, well-being, education, and healthy development. Most placements are due to maltreatment (e.g., neglect and psychological, physical and sexual abuse), and the remaining are due to abandonment by caregivers or the lack of family support (ISS, 2022). All RCHs have a technical (e.g., technical director, psychologist, social worker), educational (e.g., educators, direct care staff), and support (e.g., cook, cleaning staff) teams, being supervised by the public Welfare Services. Staff from educational and support teams often do not have an academic degree or pre-service training, and might work in rotating shifts. In accordance with a recent assessment of the quality of care in Portuguese RCHs, most of the RCHs revealed not to use evidence-based practices or interventions (Rodrigues & Barbosa-Ducharne, 2017).
Participants were mostly female (89%), and were aged between 22 and 62 years old, with a mean age of 43.99 (SD = 10.96). The majority of participants were married (69%), 23% were single and 7.9% were divorced. Participants had been working within RYC settings for less than a month to 39 years (M = 11.95, SD = 8.99), having a technical (29.4%; e.g., management, psychologist, social worker), educative (63.5%; e.g., educational assistant) or support (7.1%; e.g., cleaning staff, cooker) function. Half of them (52%) reported they were working in shifts. Concerning educational level, 44.1% had a higher education degree, 19.7% reported having completed high school, and 36.2% some level of elementary or middle school education. No significant differences between groups were found in sociodemographic features (cf. Table 1).
Sample Size
Effective sample size was determined for usual factorial (2 groups) repeated measures (4 assessments) between factors, using G*Power, version 3.1.9.7, considering alpha = 0.05, a medium effect size (Cohen’s f = 0.36) to obtain at least 80% power, assuming a 0.80 correlation coefficient within repeated measures. Under these assumptions, a total of 54 caregivers should be enrolled, 27 in each experimental condition.
Intervention
The CMT-Care Homes is a manualized program developed for professional caregivers working in RYC. Main goals are to cultivate a compassionate-self and foster a caregiving mentality in RYC. It is strongly based on the Compassion Focused Therapy theoretical framework (e.g., affect regulation systems, flows, and fears of compassion) and Compassion Mind Training practices (e.g., compassionate imagery, soothing rhythm breathing, compassionate letter) (Gilbert, 2020) applied to the RYC needs and practices. The CMT-Care Homes is made of twelve 2-h and half structured sessions, offered once a week, during approximately three months. Sessions took place at the workplace in a group format, ranging from 6 to 12 participants.
All sessions present the same structure (check-in, exploration, and check-out). Program contents are organized across three modules: (1) Our mind according to a compassion-based approach (to provide insight into the evolved and socially shaped mind and the affect regulation systems; composed of 6 sessions); (2) Compassionate mind training (understanding and cultivating the attributes and competencies of the three flows of compassion, and addressing its fears; composed of 5 sessions); and (3) a Final session (revising key information/practices, and its application into the RCH; composed of 1 session). Contents are explored through psychoeducation and experiential practices followed by group opportunities to debate and share experiences. Considering that the transfer of learnings from training to everyday life constitutes a recurrent problem in RYC (Liu & Smith, 2011), throughout the program, participants are invited to reflect on how session’s learnings can be transferred into: 1) their own daily routine (e.g., self-regulation, self-care, balance between personal and professional life); 2) their relationship with children and youth (e.g., understanding their behavior and using adequate strategies to help them to regulate their emotions); 3) RCHs’ practices and routines (e.g., team work, communication). A compassionate weekly challenge, including between sessions training of formal meditation practices and compassionate learnings, is also given to encourage the transference of CMT-Care Homes’ learnings to caregivers’ daily routine and work tasks.
Measures
The Professional Quality of Life Scale, Version 5 (ProQOL-5; Stamm, 2010; Portuguese Version by Carvalho, 2011)
ProQOL is a 30-item self-report scale designed to measure the positive and negative effects of working in stressful environments. ProQOL is composed of three subscales: Compassion Satisfaction (CS), Burnout (BO) and Secondary Traumatic Stress (STS). Participants are instructed to indicate how frequently each item was experienced in the workplace, during the previous 30 days, using a 5-point scale (1 = never, to 5 = very often). The original version reported internal consistency values of 0.88 for CS, 0.75 for BO, and 0.81 for STS (Stamm, 2010). The Portuguese version also showed good internal consistency (CS α = 0.86, BO α = 0.71, STS α = 0.83) (Carvalho, 2011). In this study, Cronbach’s alphas were 0.81 for CS, 0.64 for BO and 0.67 for STS.
Depression, Anxiety and Stress Scales (DASS-21; Lovibond & Lovibond, 1995 ; Portuguese Version by Pais-Ribeiro et al., 2004)
DASS-21 is a 21-item self-report scale designed to assess symptoms of depression, anxiety, and stress. Participants are asked to rate how much each statement applied to them during the previous week, using a 4-point scale (0 = not apply at all to me, to 3 = applied to me most of the time). In the original version, the DASS-21 subscales presented high internal consistency: Depression α = 0.91, Anxiety α = 0.84, and Stress α = 0.90 (Lovibond & Lovibond, 1995). The Portuguese version showed good internal consistency (Depression α = 0.85, Anxiety α = . 74, Stress α = 0.81) and good convergent and discriminant validity (Pais-Ribeiro et al., 2004). In this study, Cronbach’s alphas were 0.87 for depression, 0.86 or anxiety and 0.87 for stress.
Self-Compassion Scale (SCS; Neff, 2003; Portuguese Version by Castilho et al., 2015)
SCS is a 26 self-reported scale designed to assess self-compassion. Participants are instructed to answer the items regarding “how I typically act towards myself in difficult times”, using a 5-point scale (1 = almost never, to 5 = almost always). In the original version, the scale has a total score (α = 0.92) and six subscales (Self-Kindness, Self-Judgement, Common Humanity, Isolation, Mindfulness, and Over-Identification), with alpha values ranging from 0.75 for Mindfulness to 0.81 for Over-Identification (Neff, 2003). In the current study, we used the two-factor model found in the Portuguese version: Self-Compassionate attitude (comprising the positive subscales: Self-Kindness, Common Humanity, Mindfulness) and Self-Critical attitude (comprising the negative subscales: Self-Judgement, Isolation and Over-Identification), with alpha coefficients of 0.91 and 0.89, respectively (Costa et al., 2015). In the current study, Self-Critical attitude was used as a covariate (α = 0.88).
Pandemic Related Questions
Considering that Covid-19 pandemic co-occurred with 3 and 6-month follow-up assessments, a brief questionnaire was developed to address the level of anxiety that the pandemic triggered on caregivers. It was assessed through one item question (“Please indicate the level of anxiety that the current situation of COVID-19 causes you”), ranging from 0 “nothing” to 10 “extremely”. For the treatment group, the questionnaire also addressed the level of usefulness of the CMT-Care Homes to deal with the pandemic (“Please indicate to what extent CMT-Care Homes is useful to deal with the current situation of COVID-19, e.g., fear, anxiety, change in routines and habits, social isolation, uncertainty regarding the future”) and with children and youth during lockdown measures (“Please indicate how useful the CMT-Care Homes is to deal with children and young people in residential care during the current COVID-19 pandemic”), using the same scale.
Procedures
Written informed consent was sought at the cluster (i.e., boards of each RCH) and at the individual level (i.e., caregivers), before randomization. Participants were informed of the goals and procedures, and were asked to voluntarily participate, with no incentives offered for participation. Anonymity was guaranteed, with the use of respondent-specific codes, which were also used to link the data from one timepoint to the other. Caregivers were assessed through self-report measures at baseline, post-treatment, 3 and 6-month follow-up. Considering that the Covid-19 outbreak started during the current CRT, at 3 and 6-month follow-up caregivers were also asked to answer to a questionnaire about the level of anxiety concerning pandemic and usefulness of the program in that context. Due to the pandemic situation, data were collected in person by a researcher assistant (when possible) or were sent to each RCH to be filled out individually. After the baseline assessment, a computer-generated randomization was conducted at the cluster level, following a completely randomized design by the third author of this paper. Each RCH (i.e., cluster) was randomly assigned to treatment or control group (i.e., no training in compassion or any other group interventions). The CMT-Care Homes program was delivered in accordance with the handbook, in a face-to-face format, weekly (2.5-h session) in each RCH, to a group of 6–12 participants, over approximately 3 months, from October 2019 to February 2020. All sessions were delivered by the first author, who is a clinical psychologist trained in cognitive-behavioral interventions and compassionate approaches.
Data Analysis
Data was analyzed with IBM SPSS Statistics v25. Prior to analysis, data were screened for missing data, outliers, and multivariate analysis of covariance (MANCOVA) assumptions (Tabachnick & Fidell, 2013). Missing data were examined by incidence and distribution, both by subject and per item. Five participants presenting more than 20% of missing values in an outcome variable were removed (Peng et al., 2006). Little's (1988) MCAR tests revealed that data in some outcome variables were not missing completely at random (p < 0.05). Considering that deletion of cases would lead to a substantial loss of subjects, missing values of participants with less than 20% of missing data in one outcome variable were dealt via linear interpolation imputation method (Meyers et al., 2006).
Baseline differences between the two groups were examined for demographics and for outcome variables, via independent samples t-tests and chi-square statistics. The effect sizes were calculated, using Cohen’s d, with 0.15 indicating a small effect, 0.36 a medium effect and 0.65 a large effect (Lovakov & Agadullina, 2021); and Cramer’s V, with 0.10 indicating a small effect, 0.30 a medium effect, and 0.50 a large effect (Cohen, 1988).
Although confirming normal univariate distribution by coefficients of skewness and kurtosis (SK <|3| and Ku <|10|; Kline, 2005), with skewness values ranging from − 1.126 to 2.057 and kurtosis values ranging from − 0.564 to 4.963, data did not reveal a multivariate normal distribution (assessed via Mardia’s test; Korkmaz et al., 2014). Violations of normality can, however, be disregarded considering the absence of multivariate outliers (investigated via Mahalanobis distance; Tabachnick & Fidell, 2013). The homogeneity of variance–covariance matrices was ensured (assessed via Box’ M test, p > 0.001) (Field, 2018). Multicollinearity was absent, since correlations between outcome variables were < 0.90 (Tabachnick & Fidell, 2013).
To investigate intervention effects on the multiple outcomes, a two-factor (i.e., between subjects—groups—and within subjects—time) mixed MANCOVA was conducted. In accordance with former research, baseline levels of self-critical attitude were controlled due to individual differences in self-criticism on the response to compassion-based interventions (e.g., chronically self-critical individuals have more difficulties in accessing self-reassuring imagery; Duarte et al., 2015; Gilbert et al., 2004; Matos et al., 2022a), and its role as a major vulnerability factor for several mental disorders (Werner et al., 2019). Education degree was entered as a co-variate in the analysis, considering its possible influence on stress levels (Del Valle et al., 2007; Santos et al., 2022a).
For MANCOVA multivariate test, the Pillai’s criterion was used, as it is considered most robust when assumptions are not fully met (Field, 2018). Sphericity was analyzed via Mauchly’s W. When this assumption was not verified, the Greenhouse–Geisser epsilon were checked and when ε \(>\)0.75 Huynh–Feldt criterion was used in univariate tests. Effect sizes for the time effects and time × group effects were calculated using partial eta squares (\({\eta }_{p}^{2}\)), with \({\eta }_{p}^{2}\) = 0.01 referring to a small effect size, 0.06 to a medium effect size and 0.14 to a large effect size (Tabachnick & Fidell, 2013). To understand group differences, Cohen’s d was computed for long-term changes.
Pearson correlations were computed between anxiety related with pandemic and outcome measures for follow-up assessments.
Results
Recruitment and Retention
All caregivers from the 12 RCHs accepted to participate and completed the baseline assessment (N = 127) (cf., Fig. 1). RCHs were randomly distributed to the treatment (6 RCH; N = 66 caregivers) and control (6 RCH; N = 61 caregivers) groups. Of the initial 66 participants allocated to the treatment group, seven (10.61%) did not complete the program: two withdrew due to cancellation of the job contract, three due to prolonged medical discharge, and two dropped out from intervention. Fifty-nine (89.39%) participants completed the program and 57 the posttreatment assessments (86.36%; two caregivers were in medical discharge at time of assessment). Five participants (7.58%) were lost to assessment at 3-month follow-up: two of them due to job contract cancelation, one was transferred to another social response, one was at medical discharge, and one protocol was invalid. Another five participants were lost to assessment at 6-month follow-up (7.58%): two of them due to contract cancelation, two had invalid protocols, and one dropped out. Caregivers within this condition attended 5 to 12 sessions (M = 9.52; SD = 1.99). The main reasons for not completing the whole program were working in shifts/day off, vacation, brief medical discharge or urgent professional diligences. Four caregivers (6.78%) who attended less than 60% of the sessions were excluded from the analyses.
Of the 61 caregivers allocated to the control group, 51 (83.61%) completed the posttreatment assessment, one left the study due to cancellation of the job contract, one was transferred to another social response, and eight dropped out the study. Nine participants were lost to assessment at 3-month follow-up (14.75%): four of them due to contract cancelation, four due to medical discharge, and one dropped out. At 6-month follow-up four participants were lost to assessment (6.56%): one due to medical discharge, one was transferred to another social response, and two dropped out. Four participants (6.56%) were excluded from analyses due to missing data. In total, 77 caregivers (89.6% females), aged between 22 and 62 years old, were included in the analysis, at the experimental (N = 43) or control (N = 34) groups. At 3-month follow-up, 72.1% of the participants at CMT-Care Homes continued to practice exercises and 92.9% still applied the learnings related with the program. At 6-month follow-up percentages were 61.9% and 78.6%, respectively.
Baseline Differences
No significant differences were found between treatment and control group at the onset of the study for demographics (cf., Table 1) and outcome measures (all p > 0.05) (cf., Table 2).
Two-Factor Mixed MANCOVA
Multivariate tests, with self-critical attitude and education degree as covariates, demonstrated a significant Time × Group interaction effect (Pillais’ trace = 0.150, F = 1.890, p = 0.014) corresponding to a small effect size (\({\eta }_{p}^{2}\) = 0.050). Univariate tests for Time × Group interaction, with the same covariates, indicated that when compared with the control group, the treatment group had significantly lower scores in burnout, depression and anxiety (cf., Table 3). These differences corresponded to small to moderate effect sizes. No significant differences were found between groups for stress, compassion satisfaction, and secondary traumatic stress.
When examining means, standard deviations, and corresponding effect sizes (Cohen's d for each group), results showed that caregivers from the treatment group gradually reduced their burnout levels from preintervention to 6-month follow-up (Cohen's d = 0.30). In turn, for the control group, burnout levels were kept stable from preintervention to 6-month follow-up (Cohen's d = 0.13).
In what concerns depression, caregivers from the treatment group progressively improved from preintervention to 6-month follow-up (Cohen's d = 0.49), while the control group did not change across time (Cohen's d = 0.10). Regarding anxiety symptoms, the treatment group gradually decreased anxiety levels from preintervention to 6-month follow-up (Cohen's d = 0.60). In turn, the control group showed a tendency for increasing anxiety from preintervention to 6-month follow-up (Cohen's d = 0.35). These differences corresponded to small to moderate effect sizes.
The Impact of Covid-19 Pandemic
Anxiety related with the Covid-19 outbreak was correlated with outcome variables measured at follow-up assessments, showing significant positive, but weak, associations (all r < 0.40). Exceptions were for stress and compassion satisfaction. At 3-month follow-up, corresponding to the onset of the pandemic and lockdowns, stress and anxiety related to the pandemic achieved a significant and moderate positive correlation (r = 0.406), but this association was not significant anymore at 6-month follow-up, when lockdown measures were relaxed. Compassion satisfaction and anxiety related with the pandemic did not correlate at 3-month follow-up, but showed a significant and weak negative correlation at 6-month follow-up (r = -0.293).
Groups significantly differed at the level of anxiety associated with the pandemic at 3-month follow-up (t (73) = -2.295; p = 0.025; treatment group M = 5.74, SD = 2.72 and control group M = 7.06, SD = 2.14), with controls showing higher levels. Groups did not significantly differ at 6-month follow-up (t (72) = -1.366; p = 0.176; treatment group M = 5.93, SD = 2.47 and control group M = 6.67, SD = 2.10).
Although CMT-Care Homes was not designed to deal with a pandemic, caregivers recognized the program usefulness when dealing with the contingencies associated with the Covid-19 outbreak (3-month follow-up M = 6.81, SD = 2.28; 6-month follow-up M = 6.90, SD = 2.46) and with children and youth during lockdowns (3-month follow-up M = 7.62, SD = 1.83; 6-month follow-up M = 7.48, SD = 2.29).
Discussion
The current study intended to expand the preliminary evidence on the CMT-Care Homes (Santos et al., 2022b) and test its effectiveness on caregivers’ professional quality of life and mental health outcomes, within a cluster randomized trial in a real-world setting. The CMT-Care Homes aims to cultivate a compassionate mindset on caregivers, not only through promoting compassion towards others, which sets the base for any helping profession, but also through promoting self-compassion and the openness to receive compassion from others. This would facilitate feelings of safeness with others and help to improve emotion regulation (Preckel et al., 2018; Vachon, 2016). Alongside the cultivation of compassion (Santos et al., 2022b, 2023b), the CMT-Care Homes was expected to reduce suffering and psychological distress as well. To the best of our knowledge, this is the first compassion-based program delivered to caregivers working in RYC settings.
At baseline, groups did not yield significant differences on demographic and outcome measures. These results may indicate that randomization was effective, allowing for reliable conclusions on the CMT-Care Homes’ effects.
A multivariate analysis of covariance (MANCOVA) was carried out in order to test for intervention effects on professional quality of life and mental health outcomes. When controlling for education degree and self-critical attitude at baseline, MANCOVA revealed statistically significant Time x Group interaction effects of the CMT-Care Homes on burnout, depression, and anxiety, with small to medium effect sizes. Improvements in the treatment group were observed at follow-ups. These findings are in line with previous research, highlighting the beneficial effect of compassionate-based interventions on psychological distress and mental health symptoms (Irons & Heriot-Maitland, 2020; Kirby et al., 2017; Matos et al., 2017). Similar findings were also found using compassion-based interventions in organizations (Andersson et al., 2022), and specifically in caring-focused environments, with caregivers of patients with intellectual disabilities (Sansó et al., 2017) and teachers in school settings (Matos et al., 2022a).
Our findings indicated improvements from baseline to 6-months follow-up for burnout, anxiety, and depression. Research involving compassion-based interventions also revealed the maintenance of changes (Irons & Heriot-Maitland, 2020; Matos et al., 2022a) or continued improvements in depression symptoms at follow-ups (Ferrari et al., 2019). Other programs designed for the RYC setting, using other theoretical frameworks, did not show significant improvements on burnout (Donald, 2015) and mental health (Vallejos et al., 2016). Hence, both the compassion training and its theoretical framework seem a promising approach to counteract burnout, anxiety, and depression on caregivers, helping to improve their functioning and the quality of the care they provide.
Previous research suggested that the maintenance and improvements in changes may be related with the practice and the transference of learned techniques and strategies into the daily routine (Maratos et al., 2019). In fact, in the present study, more than 70% of participants having received the CMT-Care Homes reported to have kept practice three months after the program completion and more than 90% reported they were still applying the learnings related with the program during 3-month follow-up assessments. At 6-month follow-up, percentages decreased, but were still over 50%. This might have contributed to the observed improvements in mental health symptoms, even when facing new challenges linked to the pandemic context.
In contrast, and for the control group, burnout and depression levels did not change from baseline to 6-month follow-up, and anxiety symptoms seemed to have gradually increased. This might suggest that, in face of usual demands of this particular care setting, plus the additional challenges of the pandemic, when no training or support is offered, caregivers’ mental health might tend to deteriorate over time, which might have negative implications both for their own quality of life, as for the quality of the care they provide (Sinclair et al., 2021). Also, the level of anxiety related with the pandemic reported on the first follow-up, which co-occurred with the first lockdown at the onset of the COVID 19 pandemic in Portugal, was significantly higher for the control than for the treatment group. Accordingly, participants in the CMT-Care Homes recognized the usefulness of the program in dealing both with the contingencies associated with the pandemic and with children and youth during the lockdowns. Although it has not been designed to deal with the Covid-19, a training of this nature seems to be helpful to cope with stressful events like a pandemic. This is in line with research conducted during the pandemic outbreak, which demonstrated the protective role of compassion on mental health, by buffering the harmful effects of the Covid-19 (Matos et al., 2022b).
Compassion satisfaction, STS, and stress did not reveal significant differences between groups across time. Compassion satisfaction refers to the pleasure derived from being able to provide care to others (Stamm, 2010). It is important to recognize that other organizational factors that are beyond the scope of this program (e.g., work overload, low payment) may have influenced these outcomes. In addition, compassion satisfaction changes have not been found in other studies with caregivers from other care settings (Delaney, 2018; Matos et al., 2022a; Pfaff et al., 2017; Potter et al., 2013). Similarly, a resiliency program including self-care strategies and mindfulness to deal with compassion fatigue in a health care setting did not achieve changes on compassion satisfaction or STS (Pfaff et al., 2017). STS commonly occurs in professionals who deal with traumatized clients, developing their own symptoms of traumatic stress and similar reactions as posttraumatic stress disorder (PTSD, e.g., re-experiencing, avoidance and hyperarousal; Bride et al., 2007). Hence, 12-group sessions may have not been sufficient or even adequate to treat a clinical condition such as STS. It is also important to emphasize that most participants did not report high levels of STS at baseline. Thus, this finding might be attributed to the sample’s apparent floor effect, as it occurred in a former randomized controlled trial of acceptance and commitment therapy for social workers (Brinkborg et al., 2011), which did not find significant effects for professionals with low levels of stress at baseline.
In what concerns stress, stress levels were found to be moderately correlated with perceived threat of COVID-19 reported at the 3-month follow-up. Considering that the pandemic onset and its additional challenges (Carvalho et al., 2022; Ravens-Sieberer et al., 2020; Whitt-Woosley et al., 2022) co-occurred with follow-up assessments, this might have somehow influenced the results. This finding is aligned with research suggesting that the perceived threat of COVID-19 was associated with higher scores in stress (Matos et al., 2022b).
This CRT provides evidence about a new program to support the mental health and the quality of life of professionals working within RYC. The CMT-Care Homes covers the research gaps reported on a recent systematic review (Santos et al., 2023a) and is aligned with international recommendations to protect the RYC staff well-being (Whittaker et al., 2016). It also extends the research regarding compassion-based interventions in helping settings to RYC, showing that a compassion training may have a buffering effect over caregiver’s mental health concerns. Findings also suggested that, when no training is offered, caregivers tend to deteriorate their mental health across time. Considering the personal and organizational costs of caring, organizations should prioritize staff training and support in order to protect caregivers’ well-being and to prevent staff turnover, which is a significant threat to the implementation of new models and evidence-based practices (Steinlin et al., 2017). Additionally, and in order to overcome the continuous changes in staffing as one of the major challenges to maintain effectiveness of trainings over time (Ogden & Fixsen, 2015), it seems essential that RCH psychologists can be trained to deliver the program to future staff members. To do so, training budgets, often viewed as dispensable when organizational cuts are made, must be protected (Hofmeyer et al., 2020).
Some limitations should be kept in mind when considering the findings of the current study. First, despite using standardized measures, the exclusive reliance on self-report instruments might encompass associated bias. Since psychophysiological measures (e.g., hair or salivary cortisol, heart rate variability) have been used to assess psychophysiological correlates of compassion, emotion regulation, and stress (Schmid et al., 2020; Sousa et al., 2021), future research should resort to such measures as a way to strengthen self-report findings. Second, the sample size prevented resorting to more sophisticated statistics to analyze longitudinal data (e.g., latent growth curve models). Other studies have also reported difficulties in collecting longitudinal data in these settings due to the rotativity of staff linked with turnover (Schmid et al., 2020; Turner, 2017; Vallejos et al., 2016). Nevertheless, future research should replicate this study with larger samples and in another time, in order to investigate the CMT-Care Homes effectiveness outside of pandemic related constraints.
To conclude, findings highlight the utility and relevance of compassion-focused interventions in RYC settings, showing the potential benefits of the CMT-Care Homes in helping caregivers to develop socio-emotional competencies for caring for their own mental health and professional quality of life, while taking care of vulnerable youth.
Availability of Data and Material
The datasets generated and analysed during the current study are available from the corresponding author upon request. The corresponding author takes responsibility for the integrity of the data and the accuracy of the data analysis.
Code Availability
The custom code generated during the current study are available from the corresponding author upon request.
References
Andersson, C., Mellner, C., Lilliengren, P., Einhorn, S., Bergsten, K. L., Stenström, E., & Osika, W. (2022). Cultivating compassion and reducing stress and mental ill-health in employees—A randomized controlled study. Frontiers in Psychology, 12, 1–11. https://doi.org/10.3389/fpsyg.2021.748140
Babenko, O., Mosewich, A., Lee, A., & Koppula, S. (2019). Association of physicians’ self-compassion with work engagement, exhaustion, and professional life satisfaction. Medical Sciences, 7(2), 29. https://doi.org/10.3390/medsci7020029
Barford, S. W., & Whelton, W. J. (2010). Understanding burnout in child and youth care workers. Child and Youth Care Forum, 39(4), 271–287. https://doi.org/10.1007/s10566-010-9104-8
Barnard, L. K., & Curry, J. F. (2011). Self-compassion: Conceptualizations, correlates, & interventions. Review of General Psychology, 15, 289–303. https://doi.org/10.1037/a0025754
Boellinghaus, I., Jones, F. W., & Hutton, J. (2014). The role of mindfulness and loving-kindness meditation in cultivating self-compassion and other-focused concern in health care professionals. Mindfulness, 5, 129–138. https://doi.org/10.1007/s12671-012-0158-6
Bratt, A. S., Svensson, I., & Rusner, M. (2019). Finding confidence and inner trust as a parent: Experiences of group-based compassion-focused therapy for the parents of adolescents with mental health problems. International Journal of Qualitative Studies on Health and Well-Being, 14(1), 1684166. https://doi.org/10.1080/17482631.2019.1684166
Bride, B. E., Radey, M., & Figley, C. R. (2007). Measuring compassion fatigue. Clinical Social Work Journal, 35(3), 155–163. https://doi.org/10.1007/s10615-007-0091-7
Brinkborg, H., Michanek, J., Hesser, H., & Berglund, G. (2011). Acceptance and commitment therapy for the treatment of stress among social workers: A randomized controlled trial. Behaviour Research and Therapy, 49(6–7), 389–398. https://doi.org/10.1016/j.brat.2011.03.009
Bürgin, D., Kind, N., Schröder, M., Clemens, V., Fegert, J. M., Eckert, A., Buchheim, A., O’Donovan, A., Boonmann, C., & Schmid, M. (2020). The stress of caring—Resilience and HPA-Axis activity in hair samples of youth residential caregivers. Frontiers in Psychiatry, 11, 556486. https://doi.org/10.3389/fpsyt.2020.556486
Campbell, M., Piaggio, G., Elbourne, D. R., & Altman, D. (2012). Consort 2010 statement: Extension to cluster randomised trials. BMJ, 345, e5661. https://doi.org/10.1136/bmj.e5661
Carvalho, P. (2011). Estudo da fadiga por compaixão nos cuidados paliativos em Portugal: Tradução e adaptação cultural da Escala Professional Quality of Life-5. [Study of compassionate fatigue in palliative care in Portugal: Translation and cultural adaptation of the Professional Quality of Life-5 Scale.] Unpublished Master Dissertation. Catholic University of Portugal, Porto.
Carvalho, H. M., Mota, C. P., Santos, B., Costa, M., & Matos, P. M. (2022). From chaos to normalization and deconfinement: What did the pandemic unveil in youth residential care. Child and Adolescent Social Work Journal. https://doi.org/10.1007/s10560-021-00808-2
Castilho, P., Pinto-Gouveia, J., & Duarte, J. (2015). Evaluating the multifactor structure of the long and short versions of the self-compassion scale in a clinical sample. Journal of Clinical Psychology, 71, 856–870. https://doi.org/10.1002/jclp.22187
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum.
Colton, M., & Roberts, S. (2007). Factors that contribute to high turnover among residential child care staff. Child & Family Social Work, 12(2), 133–142. https://doi.org/10.1111/j.1365-2206.2006.00451.x
Costa, J., Marôco, J., Pinto-Gouveia, J., Ferreira, C., & Castilho, P. (2015). Validation of the psychometric properties of the self-compassion scale. Testing the factorial validity and factorial invariance of the measure among borderline personality disorder, anxiety disorder, eating disorder and general populations. Clinical Psychology and Psychotherapy, 23(5), 460–468. https://doi.org/10.1002/cpp.1974
Del Valle, J. F., López, M., & Bravo, A. (2007). Job stress and burnout in residential child care workers in Spain. Psicothema, 19(4), 610–615.
Delaney, M. C. (2018). Caring for the caregivers: Evaluation of the effect of an eight-week pilot mindful self-compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLoS ONE, 13(11), 1–20. https://doi.org/10.1371/journal.pone.0207261
Donald, E. J. (2015). The effects of child teacher relationships training on residential care workers: A mixed methods study. [Dissertation, The University of North Carolina]. ProQuest Dissertation and Theses database.
Duarte, J., McEwan, K., Barnes, C., Gilbert, P., & Maratos, F. A. (2015). Do therapeutic imagery practices affect physiological and emotional indicators of threat in high self-critics? Psychology and Psychotherapy: Theory, Research and Practice, 88(3), 270–284. https://doi.org/10.1111/papt.12043
Ferrari, M., Hunt, C., Harrysunker, A., Abbott, M. J., Beath, A. P., & Einstein, D. A. (2019). Self-compassion interventions and psychosocial outcomes: A meta-analysis of RCTs. Mindfulness, 10, 1455–1473. https://doi.org/10.1007/s12671-019-01134-6
FICE, IFCO, & SOS Children’s Villages. (2007). Quality4Children Standards for out-of-home children care in Europe. http://quality4children.info/navigation/show.php3?id=2&_language=en.
Field, A. (2018). Discovering statistics using IBM SPSS statistics (5th ed.). SAGE.
Gilbert, P. (2019). Explorations into the nature and function of compassion. Current Opinion in Psychology, 28, 108–114. https://doi.org/10.1016/j.copsyc.2018.12.002
Gilbert, P. (2020). Compassion: From its evolution to a psychotherapy. Frontiers in Psychology, 11, 586161. https://doi.org/10.3389/fpsyg.2020.586161
Gilbert, P., Clarke, M., Hempel, S., Miles, J. N. V., & Irons, C. (2004). Criticizing and reassuring oneself: An exploration of forms, styles and reasons in female students. The British Journal of Clinical Psychology, 43(1), 31–50.
Gilbert, P., McEwan, K., Matos, M., & Rivis, A. (2011). Fears of compassion: Development of three self-report measures. Psychology and Psychotherapy: Theory, Research and Practice, 84, 239–255. https://doi.org/10.1348/147608310X526511
Gracia-Gracia, P., & Oliván-Blázquez, B. (2017). Burnout and mindfulness self-compassion in nurses of intensive care units. Holistic Nursing Practice, 31, 225–233. https://doi.org/10.1097/HNP.0000000000000215
Hermanto, N., & Zuroff, D. C. (2016). The social mentality theory of self-compassion and self-reassurance: The interactive effect of care-seeking and caregiving. The Journal of Social Psychology, 156(5), 523–535. https://doi.org/10.1080/00224545.2015.1135779
Hermon, S. R., & Chahla, R. (2019). A longitudinal study of stress and satisfaction among child welfare workers. Journal of Social Work, 19(2), 192–215. https://doi.org/10.1177/1468017318757557
Hidalgo, J., Maravić, M. C., Milet, R. C., & Beck, J. C. (2016). Promoting collaborative relationships in residential care of vulnerable and traumatized youth: A playfulness approach integrated with trauma systems therapy. Journal of Child and Adolescent Trauma, 9(1), 17–28. https://doi.org/10.1007/s40653-015-0076-6
Hofmeyer, A., Kennedy, K., & Taylor, R. (2020). Contesting the term ‘compassion fatigue’: Integrating findings from social neuroscience and self-care research. Collegian, 27(2), 232–237. https://doi.org/10.1016/j.colegn.2019.07.001
Instituto da Social Social [ISS]. (2022). Casa 2021 - Relatório de caracterização anual da situação de acolhimento das crianças e jovens [Annual report on the characterization of children and young people in residential care]. Instituto da Segurança Social, I.P. https://www.seg-social.pt/documents/10152/13200/CASA+2020.pdf/b7f02f58-2569-4165-a5ab-bed9efdb2653.
Irons, C., & Heriot-Maitland, C. (2020). Compassionate mind training: An 8-week group for the general public. Psychology and Psychotherapy: Theory, Research and Practice, 94(3), 443–463. https://doi.org/10.1111/papt.12320
Kirby, J., Tellegen, C., & Steindll, S. (2017). A meta-analysis of compassion-based interventions: Current state of knowledge and future directions. Behavior Therapy, 48(6), 778–792. https://doi.org/10.1016/j.beth.2017.06.003
Kline, R.B. (2005). Principles and practice of structural equation modelling (2nd ed.). Guilford Press.
Korkmaz, S., Goksuluk, D., & Zararsiz, G. (2014). MVN: An R package for assessing multivariate normality. The R Journal, 6(2), 151. https://doi.org/10.32614/rj-2014-031
Larkin, H., Beckos, B. A., & Shields, J. J. (2012). Mobilizing resilience and recovery in response to adverse childhood experiences (ACE): A restorative integral support (RIS) case study. Journal of Prevention & Intervention in the Community, 40(4), 335–346. https://doi.org/10.1080/10852352.2012.707466
Li, J., & Julian, M. M. (2012). Developmental relationships as the active ingredient: A unifying working hypothesis of ‘what works’ across intervention settings. American Journal of Orthopsychiatry, 82(2), 157–166. https://doi.org/10.1111/j.1939-0025.2012.01151.x
Little, R. J. A. (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83, 1198–1202.
Liu, J., & Smith, B. D. (2011). Transferring training to child welfare practice: Individual and collective efforts. Children and Youth Services Review, 33(1), 149–156. https://doi.org/10.1016/j.childyouth.2010.08.027
Lovakov, A., & Agadullina, E. R. (2021). Empirically derived guidelines for effect size interpretation in social psychology. European Journal of Social Psychology, 51(3), 485–504. https://doi.org/10.1002/ejsp.2752
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck depression and anxiety inventories. Behaviour Research and Therapy, 33, 335–343. https://doi.org/10.1016/0005-7967(94)00075-U
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32, 545–552. https://doi.org/10.1016/j.cpr.2012.06.003
Maratos, F. A., Montague, J., Ashra, H., Welford, M., Wood, W., Barnes, C., Sheffield, D., & Gilbert, P. (2019). Evaluation of a compassionate mind training intervention with school teachers and support staff. Mindfulness, 10(11), 2245–2258. https://doi.org/10.1007/s12671-019-01185-9
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job burnout. Annual Review of Psychology, 52, 397–422.
Matos, M., Albuquerque, I., Galhardo, A., Cunha, M., Pedroso Lima, M., Palmeira, L., Petrocchi, N., McEwan, K., Maratos, F. A., & Gilbert, P. (2022a). Nurturing compassion in schools: A randomized controlled trial of the effectiveness of a Compassionate Mind Training program for teachers. PLoS ONE, 17(3), e0263480. https://doi.org/10.1371/journal.pone.0263480
Matos, M., Duarte, C., Duarte, J., Pinto-Gouveia, J., Petrocchi, N., Basran, J., & Gilbert, P. (2017). Psychological and physiological effects of compassionate mind training: A pilot randomised controlled study. Mindfulness, 8(6), 1699–1712. https://doi.org/10.1007/s12671-017-0745-7
Matos, M., Mcewan, K., Kanovsky, M., Halamova, J., Steindl, S.R., Ferreira, N., Linharelhos, M., Rijo, D., Asano, K., Gregório, S., Márquez, M.G., Vilas, S.P., Brito-Pons, G., Lucena-Santos, P., Oliveira, M.S., Souza, E.L., Llobenes, L., Gumiy, N., Costa, M.I., …Gilbert, P. (2022b). Compassion protects mental health and social safeness during the COVID-19 pandemic across 21 countries. Mindfulness, 13, 863–880. https://doi.org/10.1007/s12671-021-01822-2.
McElvaney, R., & Tatlow-Golden, M. (2016). A traumatised and traumatising system: Professionals’ experiences in meeting the mental health needs of young people in the care and youth justice systems in Ireland. Children and Youth Services Review, 65, 62–69. https://doi.org/10.1016/j.childyouth.2016.03.017
Meyers, L., Gamst, G., & Guarino, A. J. (2006). Applied multivariate research: Design and interpretation. Sage.
Neff, K. D. (2003). Development and validation of a scale to measure self-compassion. Self and Identity, 2, 223–250. https://doi.org/10.1080/15298860390209035
Ogden, T., & Fixsen, D. L. (2015). Implementation science. Zeitschrift für Psychologie. https://doi.org/10.1027/2151-2604/a000160.
Pais-Ribeiro, J. L., Honrado, A., & Leal, I. (2004). Contribuição para o estudo da adaptação portuguesa das escalas de ansiedade, depressão, stress de Lovibond e Lovibond [Contribution for the Portuguese validation of depression, anxiety and stress scales of Lovibond and Lovibond]. Psychologica, 36, 235–246.
Peng, C. J., Harwell, M., Liou, S., & Ehman, L. H. (2006). Advances in missing data methods and implications for educational research. In S. S. Sawilowsky (Ed.), Real Data Analysis (pp. 31–78). Information Age Publishing.
Pfaff, K. A., Freeman-Gibb, L., Patrick, L. J., DiBiase, R., & Moretti, O. (2017). Reducing the “cost of caring” in cancer care: Evaluation of a pilot interprofessional compassion fatigue resiliency programme. Journal of Interprofessional Care, 31, 1–8. https://doi.org/10.1080/13561820.2017.1309364
Potter, P., Faan, T. D., Berger, J. A., Clarke, M., Pa, C., Olsen, S., & Chen, L. (2013). Evaluation of a compassion fatigue resiliency programme for oncology nurses. Oncology Nursing Forum, 40(2), 180–187. https://doi.org/10.1188/13.ONF.180-187
Preckel, K., Kanske, P., & Singer, T. (2018). On the interaction of social affect and cognition: Empathy, compassion and theory of mind. Current Opinion in Behavioural Sciences, 19(2), 1–6. https://doi.org/10.1016/j.cobeha.2017.07.010
Raskin, M., Kotake, C., Easterbrooks, M. A., Ebert, M., & Miller, L. C. (2015). Job-related stress and depression in orphanage and preschool caregivers in Ukraine. Journal of Research in Childhood Education, 29(1), 130–145. https://doi.org/10.1080/02568543.2014.978516
Ravens-Sieberer, U., Kaman, A., Otto, C., Adedeji, A., Devine, J., Erhart, M., Napp, A. K., Becker, M., Blanck-Stellmacher, U., Löffler, C., Schlack, R., & Hurrelmann, K. (2020). Mental health and quality of life in children and adolescents during the COVID-19 pandemic—results of the copsy study. Deutsches Arzteblatt International, 117, 828–829. https://doi.org/10.3238/arztebl.2020.0828
Raymond, I. (2020). Intentional practice as a method to reduce the implementation gap between science and practice in the delivery of trauma-informed residential care. Residential Treatment for Children and Youth, 37(1), 20–45. https://doi.org/10.1080/0886571X.2019.1633985
Rodrigues, S., & Barbosa-Ducharne, M. (2017). Residential child and youth care in Portugal: Current challenges and the need for quality care assessment. In T. Islam L. & Fulcher, Residential Child and Youth care in developing world—European Perspectives (Vol. 2, pp. 356–366). CYC-Net Press.
Sansó, N., Galiana, L., Cebolla, A., Oliver, A., Benito, E., & Ekman, E. (2017). Cultivating emotional balance in professional caregivers: A pilot intervention. Mindfulness, 8, 1319–1327. https://doi.org/10.1007/s12671-017-0707-0
Sansó, N., Galiana, L., Oliver, A., Sinclair, S., & Benito, E. (2015). Palliative care professionals’ inner life: Exploring the relationships among awareness, self-care and compassion satisfaction and fatigue, burnout and coping with death. Journal of Pain and Symptom Management, 50(2), 200–207. https://doi.org/10.1016/j.jpainsymman.2015.02.013
Santos, L., Ferreira, A., Ribeiro da Silva, D., Pinheiro, M. R., & Rijo, D. (2022a). Assessing occupational stress in residential youth care settings: Validation of the Stress Questionnaire for Residential Youth Care Professionals. Residential Treatment for Children & Youth. https://doi.org/10.1080/0886571X.2022.2073940
Santos, L., Miguel, R. R., Pinheiro, M. R., & Rijo, D. (2023a). Fostering emotional and mental health in residential youth care facilities: A systematic review of programs targeted to care workers. Children and Youth Services Review, 147C, 106839. https://doi.org/10.1016/j.childyouth.2023.106839
Santos, L., Pinheiro, M. R., & Rijo, D. (2022b). Compassionate mind training for caregivers of residential youth care: Early findings of a cluster randomized trial. Child Abuse & Neglect, 123, 105429. https://doi.org/10.1016/j.chiabu.2021.105429
Santos, L., Pinheiro, M. R., & Rijo, D. (2023b). Fostering an affiliative environment in residential youth care: A cluster randomized trial of a Compassionate Mind Training Program for Caregivers enrolling youth and their caregivers. Child Abuse & Neglect, 139, 106122. https://doi.org/10.1016/j.chiabu.2023.106122
Santos, L., Ribeiro da Silva, D., Pinheiro, M. R., & Rijo, D. (2023c). Impact of early memories and current experiences of warmth and safeness on adolescents’ psychological distress. Journal of Research on Adolescence, 00, 1–12. https://doi.org/10.1111/jora.12843
Schmid, M., Lüdtke, J., Dolitzsch, C., Fischer, S., Eckert, A., & Fegert, J. M. (2020). Effect of trauma-informed care on hair cortisol concentration in youth welfare staff and client physical aggression towards staff: Results of a longitudinal study. BMC Public Health, 20(1), 1–12. https://doi.org/10.1186/s12889-019-8077-2
Silva, I. S., & Gaspar, M. F. (2014). Supporting Portuguese residential child care staff: An exploratory study with the Incredible Years Basic Parent Programme. Psychosocial Intervention, 23(1), 33–41. https://doi.org/10.5093/in2014a4
Sinclair, S., Kondejewski, J., Jaggi, P., Roze, A. L., Kassam, A., Hayden, K. A., Harris, D., & Hack, T. F. (2021). What works for whom in compassion training programs offered to practicing healthcare providers: A realist review. BMC Medical Education, 21, 455. https://doi.org/10.1186/s12909-021-02863-w
Singer, T., & Klimecki, O. M. (2014). Empathy and compassion. Current Biology, 24(18), 875–878. https://doi.org/10.1016/j.cub.2014.06.054
Sousa, R., Petrocchi, N., Gilbert, P., & Rijo, D. (2021). HRV patterns associated with different affect regulation systems: Sex differences in adolescents. International Journal of Psychophysiology, 170, 156–167. https://doi.org/10.1016/j.ijpsycho.2021.10.009
St. Petersburg–USA Orphanage Research Team. (2008). The effects of early social-emotional and relationship experience on the development of young orphanage children. Monographs of the Society for Research in Child Development, 73(3), 1–297.
Stamm, B. H. (2010). The concise ProQOL manual (2nd ed.). ProQual.org.
Steinlin, C., Dölitzsch, C., Kind, N., Fischer, S., Schmeck, K., Fegert, J. M., & Schmid, M. (2017). The influence of sense of coherence, self-care and work satisfaction on secondary traumatic stress and burnout among child and youth residential care workers in Switzerland. Child and Youth Services, 38(2), 159–175. https://doi.org/10.1080/0145935X.2017.1297225
Tabachnick, B., & Fidell, L. (2013). Using Multivariate Statistics (6th ed.). Pearson.
Turner, J. (2017). The effects of biofeedback training on heart rate variability, stress, and burnout in residential childcare workers. [Dissertation, Saybrook University]. ProQuest Dissertation and Theses database.
Vachon, M. L. S. (2016). Attachment, empathy and compassion in the care of the bereaved. Grief Matters: Australian Journal of Grief and Bereavement, 19(1), 20–25.
Vallejos, E. P., Ball, M. J., Brown, P., Crepaz-Keay, D., Haslam-Jones, E., & Crawford, P. (2016). Kundalini yoga as mutual recovery: A feasibility study including children in care and their carers. Journal of Children’s Services, 11(4), 261–282. https://doi.org/10.1108/JCS-11-2015-0034
van Gink, K., Visser, K., Popma, A., Vermeiren, R. R. J. M., van Domburgh, L., van der Stegen, B., & Jansen, L. M. C. (2018). Implementing Non-violent Resistance, a method to cope with aggression in child and adolescent residential care: Exploration of staff members experiences. Archives of Psychiatric Nursing, 32(3), 353–359. https://doi.org/10.1016/j.apnu.2017.11.025
Werner, A. M., Tibubos, A. N., Rohrmann, S., & Reiss, N. (2019). The clinical trait self-criticism and its relation to psychopathology: A systematic review—Update. Journal of Affective Disorders, 246, 530–547. https://doi.org/10.1016/j.jad.2018.12.069
Whittaker, J. K., Holmes, L., Del Valle, J. F., Ainsworth, F., Andreassen, T., Anglin, J., Bellonci, C., Berridge, D., Bravo, A., Canali, C., Courtney, M., Currey, L., Daly, D., Gilligan, R., Grietens, H., Harder, A., Holden, M., James, S., Kendrick, A., … Zeira, A. (2016). Therapeutic residential care for children and youth: A consensus statement of the international work group on therapeutic residential care. Residential Treatment for Children & Youth, 33(2), 89–106. https://doi.org/10.1080/0886571X.2016.1215755
Whitt-Woosley, A., Sprang, G., & Eslinger, J. (2022). Foster care during the COVID-19 pandemic: A qualitative analysis of caregiver and professional experiences. Child Abuse and Neglect, 124, 105444. https://doi.org/10.1016/j.chiabu.2021.105444
Wilson, C. A., Mackintosh, K., Power, K., & Chan, W. Y. S. (2019). Effectiveness of self-compassion related therapies: A systematic review and metaanalysis. Mindfulness, 10, 979–995. https://doi.org/10.1007/s12671-018-1037-6
Acknowledgements
We thank to Sofia Nogueira for helping in the data collection process, and to Professor Nélio Brazão, from the Faculty of Psychology and Educational Sciences of the University of Coimbra, for statistical assistance. We also thank the Portuguese Residential Care facilities and their caregivers that collaborated on this study.
Funding
Open access funding provided by FCT|FCCN (b-on). This work was supported by the Portuguese Foundation for Science and Technology (FCT) under the grants SFRH/BD/132327/2017 and COVID/BD/152441/2022.
Author information
Authors and Affiliations
Contributions
LS: Conceptualization, Methodology, Investigation, Formal analysis, Writing—Original Draft, Review & Editing. MRP: Writing—Review. DR: Conceptualization, Methodology, Writing—Review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics Approval
The Ethics Committee of the Faculty of Psychology and Educational Sciences of the University of Coimbra approved the study (CEDI22.03.2018). All procedures were in compliance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and with APA ethical standards.
Informed Consent
Written informed consent was sought for all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Santos, L., Pinheiro, M. & Rijo, D. The Effects of the Compassionate Mind Training for Caregivers on Professional Quality of Life and Mental Health: Outcomes from a Cluster Randomized Trial in Residential Youth Care Settings. Child Youth Care Forum 53, 195–215 (2024). https://doi.org/10.1007/s10566-023-09749-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-023-09749-6