Abstract
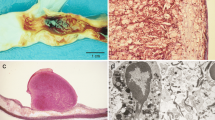
Development of a thrombus at the site of an atherosclerotic plaque initiates abrupt arterial occlusion and is the proximate event responsible for the vast majority of acute ischemic syndromes. In nearly 75% of cases thrombus overlies a disrupted or ruptured plaque whereas the remainder of the thrombi overly an intact plaque with superficial endothelial erosion. Over the past several years, it has been recognized that plaque composition rather than plaque size or stenosis severity is important for plaque rupture and subsequent thrombosis. Ruptured plaques, and by inference, plaques prone to rupture, tend to be large in size with associated expansive arterial remodeling, thin fibrous cap with a thick or large necrotic lipid core with immuno-inflammatory cell infiltration in fibrous cap and adventitia and increased plaque neovascularity and intraplaque hemorrhage. The size of the necrotic lipid core and extent and location of plaque inflammation appear to be key factors in determining plaque instability. Inflammation and immune cell activation appears to play a key role in the loss of collagen in the fibrous cap, a prelude to fibrous cap rupture, through release of collagen degrading enzymes. Furthermore, inflammation may also play a key role in the death of collagen synthesizing smooth muscle cells which further contributes to loss of fibrous cap integrity. Inflammation also is likely a key player in the ensuing thrombosis that follows plaque disruption through the elaboration of the pro-coagulant protein, tissue factor. An improved understanding of the pathophysiology of plaque vulnerability and subsequent athero-thrombosis should provide novel insights into improved prevention of athero-thrombotic cardiovascular events.

Similar content being viewed by others
References
Murray CJ, Lopez AD. Global mortality, disability and contribution of risk factors: Global Bureau of Disease Study. Lancet 1997;349:1436–42.
DeWood MA, Spores J, Notske R, et al. Prevalence of total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med. 1980;303:897–902.
DeWood MA, Stifter WF, Simpson CS, et al. Coronary arteriographic findings soon after non-Q-wave myocardial infarction. N Engl J Med. 1986;315:417–23.
Shah PK. Mechanisms of plaque vulnerability and rupture. J Am Coll Cardiol. 2003;41:15S–22S.
Shah PK. Molecular mechanisms of plaque instability. Curr Opin Lipidol. 2007;18:492–9.
Levin DC, Fallon JT. Significance of the angiographic morphology of localized coronary stenoses: histopathologic correlations. Circulation 1982;66:316–20.
Sherman CT, Litvack F, Grundfest W, et al. Coronary angioscopy in patients with unstable angina pectoris. N Engl J Med. 1986;315:913–9.
Kruskal JB, Commerford PJ, Franks JJ, Kirsch RE. Fibrin and fibrinogen-related antigens in patients with stable and unstable coronary artery disease. N Engl J Med. 1987;317:1361–5.
Falk E. Plaque rupture with severe preexisting stenosis precipitating coronary thrombosis. Characteristics of coronary atherosclerotic plaques underlying fatal occlusive thrombi. Br Heart J. 1983;50:127–34.
Davies MJ, Thomas A. Thrombosis and acute coronary-artery lesions in sudden cardiac ischemic death. N Engl J Med. 1984;310:1137–40.
Ambrose JA, Winters SL, Arora RR, et al. Coronary angiographic morphology in myocardial infarction: a link between the pathogenesis of unstable angina and myocardial infarction. J Am Coll Cardiol. 1985;6:1233–8.
Ambrose JA, Winters SL, Stern A, et al. Angiographic morphology and the pathogenesis of unstable angina pectoris. J Am Coll Cardiol. 1985;5:609–16.
Burke AP, Farb A, Malcom GT, et al. Coronary risk factors and plaque morphology in men with coronary disease who died suddenly. N Engl J Med. 1997;336:1276–82.
Ambrose JA, Hjemdahl-Monsen C, Borrico S, et al. Quantitative and qualitative effects of intracoronary streptokinase in unstable angina and non-Q wave infarction. J Am Coll Cardiol. 1987;9:1156–65.
Ambrose JA, Winters SL, Arora RR, et al. Angiographic evolution of coronary artery morphology in unstable angina. J Am Coll Cardiol. 1986;7:472–8.
Ambrose JA, Monsen C. Significance of intraluminal filling defects in unstable angina. Am J Cardiol. 1986;57:1003–4.
Little WC, Constantinescu M, Applegate RJ, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation 1988;78:1157–66.
Hackett D, Davies G, Maseri A. Preexisting coronary stenoses in patients with first myocardial infarction are not necessarily severe. Eur Heart J. 1988;9:1317–23.
Giroud D, Li JM, Urban P, et al. Relation of the site of acute myocardial infarction to the most severe coronary arterial stenosis at prior angiography. Am J Cardiol. 1992;69:729–32.
Brown G, Albers JJ, Fisher LD, et al. Regression of coronary artery disease as a result of intensive lipid-lowering therapy in men with high levels of apolipoprotein B. N Engl J Med. 1990;323:1289–98.
Naqvi TZ, Hachamovitch R, Berman D, et al. Does the presence and site of myocardial ischemia on perfusion scintigraphy predict the occurrence and site of future myocardial infarction in patients with stable coronary artery disease? Am J Cardiol. 1997;79:1521–4.
Shah PK. Plaque size, vessel size and plaque vulnerability: bigger may not be better. J Am Coll Cardiol. 1998;32:663–4.
Schoenhagen P, Ziada KM, Kapadia SR, et al. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation 2000;101:598–603.
von Birgelen C, Klinkhart W, Mintz GS, et al. Plaque distribution and vascular remodeling of ruptured and nonruptured coronary plaques in the same vessel: an intravascular ultrasound study in vivo. J Am Coll Cardiol. 2001;37:1864–70.
Takano M, Mizuno K, Okamatsu K, et al. Mechanical and structural characteristics of vulnerable plaques: analysis by coronary angioscopy and intravascular ultrasound. J Am Coll Cardiol. 2001;38:99–104.
Loree HM, Kamm RD, Stringfellow RG, Lee RT. Effects of fibrous cap thickness on peak circumferential stress in model atherosclerotic vessels. Circ Res. 1992;71:850–8.
Varnava AM, Mills PG, Davies MJ. Relationship between coronary artery remodeling and plaque vulnerability. Circulation 2002;105:939–43.
Guyton JR, Klemp KF. Development of the lipid-rich core in human atherosclerosis. Arterioscler Thromb Vasc Biol. 1996;16:4–11.
Richardson PD, Davies MJ, Born GV. Influence of plaque configuration and stress distribution on fissuring of coronary atherosclerotic plaques. Lancet 1989;2:941–4.
Davies MJ, Richardson PD, Woolf N, et al. Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J. 1993;69:377–81.
Felton CV, Crook D, Davies MJ, Oliver MF. Relation of plaque lipid composition and morphology to the stability of human aortic plaques. Arterioscler Thromb Vasc Biol. 1997;17:1337–45.
Burleigh MC, Briggs AD, Lendon CL, et al. Collagen types I and III, collagen content. GAGs and mechanical strength of human atherosclerotic plaque caps: span-wise variations. Atherosclerosis 1992;96:71–81.
Moreno PR, Falk E, Palacios IF, et al. Macrophage infiltration in acute coronary syndromes. Implications for plaque rupture. Circulation 1994;90:775–8.
Moreno PR, Bernardi VH, Lopez-Cuellar J, et al. Macrophages, smooth muscle cells, and tissue factor in unstable angina. Implications for cell-mediated thrombogenicity in acute coronary syndromes. Circulation 1996;94:3090–7.
Lendon CL, Davies MJ, Born GV, Richardson PD. Atherosclerotic plaque caps are locally weakened when macrophages density is increased. Atherosclerosis 1991;87:87–90.
Depre C, Havaux X, Wijns W. Neovascularization in human coronary atherosclerotic lesions. Cathet Cardiovasc Diagn. 1996;39:215–20.
Tenaglia AN, Peters KG, Sketch MH Jr, Annex BH. Neovascularization in atherectomy specimens from patients with unstable angina: implications for pathogenesis of unstable angina. Am Heart J. 1998;135:10–4.
Feng B, Yao PM, Li Y, et al. The endoplasmic reticulum is the site of cholesterol-induced cytotoxicity in macrophages. Nat Cell Biol. 2003;5:781–92.
Kolodgie FD, Gold HK, Burke AP, et al. Intraplaque hemorrhage and progression of atheroma. N Engl J Med. 2003;349:2316–25.
Cheng GC, Loree HM, Kamm RD, et al. Distribution of circumferential stress in ruptured and stable atherosclerotic lesions. A structural analysis with histopathological correlation. Circulation 1993;87:1179–87.
Loree HM, Tobias BJ, Gibson LJ, et al. Mechanical properties of model atherosclerotic lesion lipid pools. Arterioscler Thromb. 1994;14:230–4.
Huang H, Virmani R, Younis H, et al. The impact of calcification on the biomechanical stability of atherosclerotic plaques. Circulation 2001;103:1051–6.
Vengrenyuk Y, Carlier S, Xanthos S, et al. A hypothesis for vulnerable plaque rupture due to stress-induced debonding around cellular microcalcifications in thin fibrous caps. Proc Natl Acad Sci USA. 2006;103:14678–83.
Faber BC, Cleutjens KB, Niessen RL, et al. Identification of genes potentially involved in rupture of human atherosclerotic plaques. Circ Res. 2001;89:547–54.
Fernandez-Ortiz A, Badimon JJ, Falk E, et al. Characterization of the relative thrombogenicity of atherosclerotic plaque components: implications for consequences of plaque rupture. J Am Coll Cardiol. 1994;23:1562–9.
Toschi V, Gallo R, Lettino M, et al. Tissue factor modulates the thrombogenicity of human atherosclerotic plaques. Circulation 1997;95:594–9.
Mallat Z, Hugel B, Ohan J, et al. Shed membrane microparticles with procoagulant potential in human atherosclerotic plaques: a role for apoptosis in plaque thrombogenicity. Circulation 1999;99:348–53.
Badimon JJ, Lettino M, Toschi V, et al. Local inhibition of tissue factor reduces the thrombogenicity of disrupted human atherosclerotic plaques: effects of tissue factor pathway inhibitor on plaque thrombogenicity under flow conditions. Circulation 1999;99:1780–7.
Essler M, Retzer M, Bauer M, et al. Stimulation of platelets and endothelial cells by mildly oxidized LDL proceeds through activation of lysophosphatidic acid receptors and the Rho/Rho-kinase pathway. Inhibition by lovastatin. Ann N Y Acad Sci. 2000;905:282–6.
Libby P. Inflammation in atherosclerosis. Nature 2002;420:868–74.
Laine P, Kaartinen M, Penttila A, et al. Association between myocardial infarction and the mast cells in the adventitia of the infarct-related coronary artery. Circulation 1999;99:361–9.
Barger AC, Beeuwkes R 3rd, Lainey LL, Silverman KJ. Hypothesis: vasa vasorum and neovascularization of human coronary arteries. A possible role in the pathophysiology of atherosclerosis. N Engl J Med. 1984;310:175–7.
Gojova A, Brun V, Bruno E, et al. Specific abrogation of transforming growth factor beta signaling in T cells alters atherosclerotic lesion size and composition in mice. Blood 2003;102:4052–8.
Robertson AL, Rudling M, Zhore X, et al. Disruption of TGF-beta signaling in T-cells accelerates atherosclerosis. J Clin Invest. 2003;112:1342–50.
Xu XH, Shah PK, Faure E, et al. Toll-like receptor-4 is expressed by macrophages in murine and human lipid-rich atherosclerotic plaques and upregulated by oxidized LDL. Circulation 2001;104:3103–8.
Michelsen KS, Wong MH, Shah PK, et al. Lack of Toll-like receptor 4 or myeloid differentiation factor 88 reduces atherosclerosis and alters plaque phenotype in mice deficient in apolipoprotein E. Proc Natl Acad Sci USA. 2004;101:10679–84.
Zalewski A, Macphee C. Role of lipoprotein-associated phospholipase A2 in atherosclerosis. Arterioscler Thromb Vasc Biol. 2005;25:923–31.
Serruys PW, Garcia-Garcia HM, Buszman P, et al. Effects of the direct lipoprotein-associated phospholipase A2 inhibitor Darapladip on human coronary atherosclerotic plaque. Circulation 2008;118:1172–82.
Kovanen PT. Mast cells: multipotent local effector cells in atherothrombosis. Immunol Rev. 2007;217:105–22.
Sun J, Sukhova GK, Wolters PJ, et al. Mast cells promote atherosclerosis by releasing pro-inflammatory cytokines. Nat Med. 2007;13:719–24.
Bot I, de Jager SC, Zernecke A, et al. Perivascular mast cells promote atherogenesis and induce plaque destabilization in apolipoprotein E-deficient mice. Circulation 2007;115:2516–25.
Henney AM, Wakeley PR, Davies MJ, et al. Localization of stromelysin gene expression in atherosclerotic plaques by in situ hybridization. Proc Natl Acad Sci USA. 1991;88:8154–8.
Galis ZS, Sukhova GK, Lark MW, Libby P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest. 1994;94:2493–503.
Brown DL, Hibbs MS, Kearney M, et al. Identification of 92-kD gelatinase in human coronary atherosclerotic lesions. Association of active enzyme synthesis with unstable angina. Circulation 1995;91:2125–31.
Nikkari ST, O’Brien KD, Ferguson M, et al. Interstitial collagenase (MMP-1) expression in human carotid atherosclerosis. Circulation 1995;92:1393–8.
Li Z, Li L, Zielke HR, et al. Increased expression of 72-kd type IV collagenase (MMP-2) in human aortic atherosclerotic lesions. Am J Pathol. 1996;148:121–8.
Galis ZS, Sukhova GK, Libby P. Microscopic localization of active proteases by in situ zymography: detection of matrix metalloproteinase activity in vascular tissue. FASEB J. 1995;9:974–80.
Xu XP, Meisel SR, Ong JM, et al. Oxidized low-density lipoprotein regulates matrix metalloproteinase-9 and its tissue inhibitor in human monocyte-derived macrophages. Circulation 1999;99:993–8.
Rajavashisth TB, Xu XP, Jovinge S, et al. Membrane type 1 matrix metalloproteinase expression in human atherosclerotic plaques: evidence for activation by proinflammatory mediators. Circulation 1999;99:3103–9.
Rajavashisth TB, Liao JK, Galis ZS, et al. Inflammatory cytokines and oxidized low density lipoproteins increase endothelial cell expression of membrane type 1-matrix metalloproteinase. J Biol Chem. 1999;274:11924–9.
Herman MP, Sukhova GK, Libby P, et al. Expression of neutrophil collagenase (matrix metalloproteinase-8) in human atheroma: a novel collagenolytic pathway suggested by transcriptional profiling. Circulation 2001;104:1899–904. Ovid.
Shah PK, Falk E, Badimon JJ, et al. Human monocyte-derived macrophages induce collagen breakdown in fibrous caps of atherosclerotic plaques. Potential role of matrix-degrading metalloproteinases and implications for plaque rupture. Circulation 1995;92:1565–9.
Shah PK. Role of inflammation and metalloproteinases in plaque disruption and thrombosis. Vasc Med. 1998;3:199–206.
Sukhova GK, Schonbeck U, Rabkin E, et al. Evidence for increased collagenolysis by interstitial collagenases-1 and -3 in vulnerable human atheromatous plaques. Circulation 1999;99:2503–9.
Wallner K, Li C, Shah PK, et al. Tenascin-C is expressed in macrophage-rich human coronary atherosclerotic plaque. Circulation 1999;99:1284–9.
Sukhova GK, Shi GP, Simon DI, et al. Expression of the elastolytic cathepsins S and K in human atheroma and regulation of their production in smooth muscle cells. J Clin Invest. 1998;102:576–83.
Mallat Z, Tedgui A. Apoptosis in the vasculature: mechanisms and functional importance. Br J Pharmacol. 2000;130:947–62.
Rossig L, Dimmeler S, Zeiher AM. Apoptosis in the vascular wall and atherosclerosis. Basic Res Cardiol. 2001;96:11–22.
Kockx MM, Knaapen MW. The role of apoptosis in vascular disease. J Pathol. 2000;190:267–80.
Wallner K, Li C, Shah PK, et al. EGF-Like domain of tenascin-C is proapoptotic for cultured smooth muscle cells. Arterioscler Thromb Vasc Biol. 2004;24:1416–21.
Kolmakova A, Kwiterovich P, Virgil D, et al. Apolipoprotein C-I induces apoptosis in human aortic smooth muscle cells via recruiting neutral sphingomyelinase. Arterioscler Thromb Vasc Biol. 2004;24:264–9.
Durand E, Scoazec A, Lafont A, et al. In vivo induction of endothelial apoptosis leads to vessel thrombosis and endothelial denudation: a clue to the understanding of the mechanisms of thrombotic plaque erosion. Circulation 2004;109:2503–6.
Sugiyama S, Kugiyama K, Aikawa M, et al. Hypochlorous acid, a macrophage product, induces endothelial apoptosis and tissue factor expression: involvement of myeloperoxidase-mediated oxidant in plaque erosion and thrombogenesis. Arterioscler Thromb Vasc Biol. 2004;24:1309–14.
Schwartz SM, Galis ZS, Rosenfeld ME, Falk E. Plaque rupture in humans and mice. Arterioscler Thromb Vasc Biol. 2007;27:705–13.
Abela GS, Picon PD, Friedl SE, et al. Triggering of plaque disruption and arterial thrombosis in an atherosclerotic rabbit model. Circulation 1995;91:776–84.
Rekhter MD, Hicks GW, Brammer DW, et al. Animal model that mimics atherosclerotic plaque rupture. Circ Res. 1998;83:705–13.
Caligiuri G, Levy B, Pernow J, et al. Myocardial infarction mediated by endothelin receptor signaling in hypercholesterolemic mice. Proc Natl Acad Sci USA. 1999;96:6920–4.
Rosenfeld ME, Polinsky P, Virmani R, et al. Advanced atherosclerotic lesions in the innominate artery of the ApoE knockout mouse. Arterioscler Thromb Vasc Biol. 2000;20:2587–92.
Johnson JL, Jackson CL. Atherosclerotic plaque rupture in the apolipoprotein E knockout mouse. Atherosclerosis 2001;154:399–406.
Calara F, Silvestre M, Casanada F, et al. Spontaneous plaque rupture and secondary thrombosis in apolipoprotein E-deficient and LDL receptor-deficient mice. J Pathol. 2001;195:257–63.
von der Thusen JH, van Vlijmen BJ, Hoeben RC, et al. Induction of atherosclerotic plaque rupture in apolipoprotein E-/- mice after adenovirus-mediated transfer of p53. Circulation 2002;105:2064–70.
Lemaitre V, O’Byrne TK, Borczuk AC, et al. ApoE knockout mice expressing human matrix metalloproteinase-1 in macrophages have less advanced atherosclerosis. J Clin Invest. 2001;107:1227–34.
Gough PJ, Gomez IG, Wille PT, Raines EW. Macrophage expression of active MMP-9 induces acute plaque disruption in apoE-deficient mice. J Clin Invest. 2006;116:59–69.
Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation 1989;79:733–43.
Muller JE, Tofler GH. Triggering and hourly variation of onset of arterial thrombosis. Ann Epidemiol. 1992;2:393–405.
Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation 2001;103:2810–5.
Mittleman MA, Lewis RA, Maclure M, et al. Triggering myocardial infarction by marijuana. Circulation 2001;103:2805–9.
Muller JE. Circadian variation and triggering of acute coronary events. Am Heart J. 1999;137:S1–S8.
Muller JE. Triggering of cardiac events by sexual activity: findings from a case- crossover analysis. Am J Cardiol. 2000;86:14F–8F.
Goldstein JA, Demetriou D, Grines CL, et al. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343:915–22.
Matetzky S, Tani S, Kangavari S, et al. Smoking increases tissue factor expression in atherosclerotic plaques: implications for plaque thrombogenicity. Circulation 2000;102:602–4.
Burke AP, Kolodgie FD, Farb A, et al. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression. Circulation 2001;103:934–40.
Farb A, Burke AP, Tang AL, et al. Coronary plaque erosion without rupture into a lipid core. A frequent cause of coronary thrombosis in sudden coronary death. Circulation 1996;93:1354–63.
Rauch U, Bonderman D, Bohrmann B, et al. Transfer of tissue factor from leukocytes to platelets is mediated by CD15 and tissue factor. Blood 2000;96:170–5.
Mallat Z, Benamer H, Hugel B, et al. Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation 2000;101:841–3.
Sugiyama S, Kugiyama K, Aikawa M, et al. Hypochlorous acid, a macrophage product, induces endothelial cell apoptosis: involvement of myeloperoxidase-mediated oxidant in plaque erosion and thrombogenesis. Arterioscler Thromb Vasc Biol. 2004;24:1309–14.
Lindstedt KA, Leskinen MJ, Kovanen PT. Proteolysis of the pericellular matrix: a novel element determining cell survival and death in the pathogenesis of plaque erosion and rupture. Arterioscler Thromb Vasc Biol. 2004;24:1350–8.
Kolodgie FD, Burke AP, Wight TN, Virmani R. The accumulation of specific types of proteoglycans in eroded plaques: a role in coronary thrombosis in the absence of plaque rupture. Curr Opin Lipidol. 2004;15:575–82.
Laszik ZG, Zhou XJ, Ferrell GL, et al. Down-regulation of endothelial expression of endothelial cell protein C receptor and thrombomodulin in coronary atherosclerosis. Am J Pathol. 2001;159:797–802.
Crisby M, Nordin-Fredriksson G, Shah PK, et al. Pravastatin treatment increases collagen content and decreases lipid content, inflammation, metalloproteinases, and cell death in human carotid plaques: implications for plaque stabilization. Circulation 2001;103:926–33.
Shah PK. Emerging HDL-based therapies for atherothrombotic vascular disease. Curr Treat Options Cardiovasc Med. 2007;9:60–70.
Shah PK, Chyu KY, Fredrikson GN, Nilsson J. Immunomodulation of atherosclerosis with a vaccine. Nat Clin Pract Cardiovasc Med. 2005;2:639–46.
Acknowledgements
The author gratefully acknowledges the valuable contributions of many colleagues and collaborators in the Atherosclerosis Research Center at Cedars Sinai Medical Center. The support of the National Institutes of Health, the Heart Foundation, United Hostesses Charities, Corday Foundation, Spielberg-Wunderkinder Foundation and Sam Spaulding Foundation are also appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shah, P.K. Inflammation and Plaque Vulnerability. Cardiovasc Drugs Ther 23, 31–40 (2009). https://doi.org/10.1007/s10557-008-6147-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-008-6147-2