Abstract
Purpose
Previous studies estimate translation of research evidence into practice takes 17 years. However, this estimate is not specific to cancer control evidence-based practices (EBPs), nor do these studies evaluate variation in the translational process. We examined the translational pathway of cancer control EBPs.
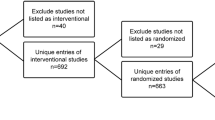
Methods
We selected five cancer control EBPs where data on uptake were readily available. Years from landmark publication to clinical guideline issuance to implementation, defined as 50% uptake, were measured. The translational pathway for each EBP was mapped and an average total time across EBPs was calculated.
Results
Five cancer control EBPs were included: mammography, clinicians’ advice to quit smoking, colorectal cancer screening, HPV co-testing, and HPV vaccination. Time from publication to implementation ranged from 13 to 21 years, averaging 15 years. Time from publication to guideline issuance ranged from 3 to 17 years, and from guideline issuance to implementation, − 4 to 12 years. Clinician’s advice to quit smoking, HPV co-testing, and HPV vaccination were most rapidly implemented; colorectal cancer screening and mammography were slowest to implement.
Conclusion
The average time to implementation was 15 years for the five EBPs we evaluated, a marginal improvement from prior findings. Although newer EBPs such as HPV vaccination and HPV co-testing were faster to implement than other EBPs, continued efforts in implementation science to speed research to practice are needed.


Similar content being viewed by others
References
Balas EA, Boren SA (2000) Managing clinical knowledge for health care improvement. In: Bemmel J, McCray AT (eds) Yearbook of medical informatics 2000: patient-centered systems. Schattauer Verlagsgesellschaft, Stuttgart, Germany, pp 65–70
Grant J, Green L, Mason B (2003) Basic research and health: a reassessment of the scientific basis for the support of biomedical science. Res Eval 12(3):217–224
Morris ZS, Wooding S, Grant J (2011) The answer is 17 years, what is the question: understanding time lags in translational research. J R Soc Med 104(12):510–520. https://doi.org/10.1258/jrsm.2011.110180
U.S. Preventive Services Task Force: Reccomendations for Primary Care Practice. https://www.uspreventiveservicestaskforce.org/Page/Name/recommendations
National Cancer Institute: Cancer Trends Progress Report. https://progressreport.cancer.gov/. https://progressreport.cancer.gov/
MacLaughlin KL, Jacobson RM, Radecki Breitkopf C, Wilson PM, Jacobson DJ, Fan C, St Sauver JL, Rutten LJF (2019) Trends over time in Pap and Pap-HPV cotesting for cervical cancer screening. J Women’s Health 28(2):244–249. https://doi.org/10.1089/jwh.2018.7380
Silver MI, Rositch AF, Phelan-Emrick DF, Gravitt PE (2018) Uptake of HPV testing and extended cervical cancer screening intervals following cytology alone and Pap/HPV cotesting in women aged 30–65 years. Cancer Causes Control 29(1):43–50. https://doi.org/10.1007/s10552-017-0976-x
National Committee for Quality Assurance: The Healthcare Effectiveness Data and Information Set. https://www.ncqa.org/hedis/measures
State Cancer Profiles: Screening and Risk Factors Table. https://statecancerprofiles.cancer.gov/risk/index.php
Centers for Disease Control and Prevention: Morbidity and Mortality Weekly Report. https://www.cdc.gov/mmwr/index.html
Agency for Healthcare Research and Quality: Clinical Guidelines and Reccomendations. https://www.ahrq.gov/professionals/clinicians-providers/guidelines-recommendations/index.html
American Cancer Society: Cancer Screening Guidelines: https://www.cancer.org/healthy/find-cancer-early/cancer-screening-guidelines.html
U.S. Preventive Services Task Force: Breast Cancer: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening1?ds=1&s=mammo
Shapiro S, Strax P, Venet L (1971) Periodic breast cancer screening in reducing mortality from breast cancer. JAMA 215(11):1777–1785
American Cancer Society: History of ACS Recommendations for the Early Detection of Cancer in People Without Symptoms. https://www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/overview/chronological-history-of-acs-recommendations.html
National Cancer Institute: Cancer Trends Progress Report. Breast Cancer Screening. https://progressreport.cancer.gov/detection/breast_cancer#field_data_source
Io M, Council NR (2001) Mammography and beyond: developing technologies for the early detection of breast cancer. The National Academies Press, Washington, DC. https://doi.org/10.17226/10030
Olsen O, Gøtzsche PC (2001) Cochrane review on screening for breast cancer with mammography. The Lancet 358(9290):1340–1342
National Cancer Institute: Cancer Trends Progress Report. Online Summary of Trends in US Cancer Control Measures. Clinicians' Advice to Quit Smoking. https://progressreport.cancer.gov/prevention/clinicians_advice
U.S. Preventive Services Task Force: Archived: Tobacco Use in Adults and Pregnant Women: Counseling and Interventions. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/tobacco-use-in-adults-and-pregnant-women-counseling-and-interventions
Russell MA, Wilson C, Taylor C, Baker CD (1979) Effect of general practitioners’ advice against smoking. BMJ 2(6184):231–235
Kottke TE, Battista RN, DeFriese GH, Brekke ML (1988) Attributes of successful smoking cessation interventions in medical practice. A meta-analysis of 39 controlled trials. JAMA 259(19):2883–2889
Fiore M, United States. Agency for Health Care Policy and Research, Centers for Disease Control and Prevention (U.S.) (1996) Smoking cessation. Clinical practice guideline, vol no 18. U.S. Dept. of Health and Human Services, Public Health Service Centers for Disease Control and Prevention; For sale by the U.S. G.P.O., Supt. of Docs., Rockville, MD, Washington, DC
Stead LF, Bergson G, Lancaster T (2008) Physician advice for smoking cessation. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000165.pub3
Force UPST (2009) Counseling and interventions to prevent tobacco use and tobacco-caused disease in adults and pregnant women: US Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med 150(8):551
Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann‐Boyce J, Lancaster T (2013) Physician advice for smoking cessation. Cochrane Database Syst Rev 2013(5):CD000165
Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, Ederer F (1993) Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota colon cancer control study. N Engl J Med 328(19):1365–1371. https://doi.org/10.1056/nejm199305133281901
Selby JV, Friedman GD, Quesenberry CP Jr, Weiss NS (1992) A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med 326(10):653–657. https://doi.org/10.1056/NEJM199203053261001
U.S. Preventive Services Task Force (1996) Guide to clinical preventive services, 2nd edn. Office of Disease Prevention and Health Promotion, Washington, DC
Centers for Medicare & Medicaid Services. Decision memo for screening immunoassay fecal-occult blood test (CAG-00180N) (2003). https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=87&fromdb=true
Byers T, Levin B, Rothenberger D, Dodd GD, Smith RA (1997) American Cancer Society guidelines for screening and surveillance for early detection of colorectal polyps and cancer: update 1997. American Cancer Society Detection and Treatment Advisory Group on Colorectal Cancer. CA Cancer J Clin 47(3):154–160
National Cancer Institute: Online Summary of Trends in US Cancer Control Measures. Colorectal Cancer Screening. https://progressreport.cancer.gov/detection/colorectal_cancer
Pignone M, Rich M, Teutsch SM, Berg AO, Lohr KN (2002) Screening for colorectal cancer in adults at average risk: a summary of the evidence for the US Preventive Services Task Force. Ann Intern Med 137(2):132–141
Hewitson P, Glasziou P, Watson E, Towler B, Irwig L (2008) Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol 103(6):1541–1549. https://doi.org/10.1111/j.1572-0241.2008.01875.x
U.S. Preventive Services Task Force: Colorectal Cancer: Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening
National Cancer Institute: Cervical Cancer: HPV and Pap Testing. https://www.cancer.gov/types/cervical/pap-hpv-testing-fact-sheet
Liaw KL, Glass AG, Manos MM, Greer CE, Scott DR, Sherman M, Burk RD, Kurman RJ, Wacholder S, Rush BB, Cadell DM, Lawler P, Tabor D, Schiffman M (1999) Detection of human papillomavirus DNA in cytologically normal women and subsequent cervical squamous intraepithelial lesions. J Natl Cancer Inst 91(11):954–960
Cuzick J, Sasieni P, Davies P, Adams J, Normand C, Frater A, van Ballegooijen M, van den Akker-van ME (2000) A systematic review of the role of human papilloma virus (HPV) testing within a cervical screening programme: summary and conclusions. Br J Cancer 83(5):561–565. https://doi.org/10.1054/bjoc.2000.1375
Food and Drug Administration. Digene Hybrid Capture 2 (HC2) High-Risk HPV DNA Test (2003). https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpma/pma.cfm?id=P890064S009
Wright TC Jr, Schiffman M, Solomon D, Cox JT, Garcia F, Goldie S, Hatch K, Noller KL, Roach N, Runowicz C, Saslow D (2004) Interim guidance for the use of human papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet Gynecol 103(2):304–309. https://doi.org/10.1097/01.AOG.0000109426.82624.f8
Cuzick J, Myers O, Hunt WC, Saslow D, Castle PE, Kinney W, Waxman A, Robertson M, Wheeler CM (2015) Human papillomavirus testing 2007–2012: co-testing and triage utilization and impact on subsequent clinical management. Int J Cancer 136(12):2854–2863. https://doi.org/10.1002/ijc.29337
U.S. Preventive Services Task Force: Cervical Cancer Screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening
Watson M, Benard V, King J, Crawford A, Saraiya M (2017) National assessment of HPV and Pap tests: changes in cervical cancer screening, National Health Interview Survey. Prev Med 100:243–247. https://doi.org/10.1016/j.ypmed.2017.05.004
Koutsky LA, Ault KA, Wheeler CM, Brown DR, Barr E, Alvarez FB, Chiacchierini LM, Jansen KU (2002) A controlled trial of a human papillomavirus type 16 vaccine. N Engl J Med 347(21):1645–1651. https://doi.org/10.1056/NEJMoa020586
Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, Centers for Disease C, Prevention, Advisory Committee on Immunization P (2007) Quadrivalent human papillomavirus vaccine: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 56(RR-2):1–24
National Cancer Institute. Cancer Trends Progress Report. HPV Vaccination. https://progressreport.cancer.gov/prevention/hpv_immunization
FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP) (2010). MMWR Morb Mortal Wkly Rep 59(20):630–632
Marra F, Cloutier K, Oteng B, Marra C, Ogilvie G (2009) Effectiveness and cost effectiveness of human papillomavirus vaccine: a systematic review. Pharmacoeconomics 27(2):127–147. https://doi.org/10.2165/00019053-200927020-00004
Meites E, Kempe A, Markowitz LE (2016) Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep 65(49):1405–1408. https://doi.org/10.15585/mmwr.mm6549a5
Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S (2017) National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep 66(33):874–882. https://doi.org/10.15585/mmwr.mm6633a2
Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Fredua B, Singleton JA, Stokley S (2019) National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 Years—United States, 2018. MMWR Morb Mortal Wkly Rep 68(33):718–723. https://doi.org/10.15585/mmwr.mm6833a2
Rimer BK (2018) HPV Vaccination for Cancer Prevention: Progress, Opportunities, and a Renewed Call to Action. A Report to the President of the United States from the Chair of the President’s Cancer Panel. Bethesda, MD
National Cancer Institute: https://grants.nih.gov/grants/guide/rfa-files/RFA-CA-19-005.html
National Cancer Institute: https://grants.nih.gov/grants/guide/rfa-files/rfa-ca-19-006.html
Institute of Medicine (U.S.) Committee on the National Quality Report on Health Care Delivery, Hurtado MP, Swift EK, Corrigan J, United States. Agency for Healthcare Research and Quality (2001) Envisioning the national health care quality report. National Academy Press, Washington, D.C.
Tabak RG, Khoong EC, Chambers DA, Brownson RC (2012) Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 43(3):337–350. https://doi.org/10.1016/j.amepre.2012.05.024
Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, Mandell DS (2017) Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res 44(2):177–194. https://doi.org/10.1007/s11414-015-9475-6
National Cancer Institute: www.nci-sprint.com
Rogers EM (1995) Diffusion of innovations, 4th edn. Free Press, New York
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC (2009) Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 4(1):50. https://doi.org/10.1186/1748-5908-4-50
Acknowledgments
The authors would like to thank Paul Doria-Rose, Kathy Helzlsouer, Hormuz Katki, Sarah Kobrin, and Bob Vollinger. The views expressed in this manuscript reflect those of the authors and not the official statements of the NIH/NCI.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by SK and GN. The first draft of the manuscript was written by SK and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Rights and permissions
About this article
Cite this article
Khan, S., Chambers, D. & Neta, G. Revisiting time to translation: implementation of evidence-based practices (EBPs) in cancer control. Cancer Causes Control 32, 221–230 (2021). https://doi.org/10.1007/s10552-020-01376-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-020-01376-z