Abstract
Background
Studies conducted in Western countries have found a robust association between higher social support and improved cancer outcomes, particularly for breast cancer incidence and prognosis. However, less is known about the influence of social support on cancer among Asian populations where the measures of social support may differ in social relationships. In this prospective cohort study in Japan, we sought to examine the associations between the incidence and mortality of total and site-specific cancer.
Methods
We examined prospectively the association between social support and risk of cancer incidence and mortality within a cohort of 44,152 Japanese men and women, aged 40–69 years, free of prior diagnosis of cancer and cardiovascular disease. Social support was measured by emotional support defined as receipt of confidant support and esteem support from family members or friends and by social isolation. A total of 3,444 cases of newly diagnosed cancer and 1,561 cancer deaths occurred between the baseline questionnaire (1993–1994) and the end of follow-up in January 2004.
Results
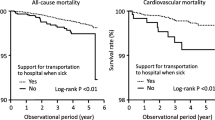
The multivariate hazard ratios (HR) and 95 % confidence intervals for colorectal cancer incidence and mortality in the highest social support versus lowest social support group were 1.48 (1.06–2.05) and 3.07 (1.65–5.69) in men, respectively. Social support was not associated with other site-specific cancer incidence or cancer outcomes in women.
Conclusions
Low social support was associated with higher risk of both colorectal cancer incidence and mortality in men. Social support may affect colorectal cancer onset and prognosis via a range of factors, including healthier lifestyles as well as adherence to therapeutic regimens.
Similar content being viewed by others
References
Garssen B (2004) Psychological factors and cancer development: evidence after 30 years of research. Clin Psychol Rev 24:315–338
Cassileth BR, Walsh WP, Lusk EJ (1988) Psychosocial correlates of cancer survival: a subsequent report 3 to 8 years after cancer diagnosis. J Clin Oncol 6:1753–1759
Pinquart M, Duberstein PR (2009) Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol 13. (Epub ahead of print)
Falagas ME, Zarkadoulia EA, Ioannidou EN, Peppas G, Christodoulou C, Rafailidis PI (2007) The effect of psychosocial factors on breast cancer outcome: a systematic review. Breast Cancer Res 9:R44
Lafayette De Mente B (2004) Japan’s cultural code words. Tuttle Publishing, Tokyo
Tsugane S, Sobue T (2001) Baseline survey of JPHC study-design and participation rate. Japan Public Health Center-Based Prospective Study on Cancer and Cardiovascular Diseases. J Epidemiol 11(suppl):S24–S29
Munakata T (1982) Psycho-social influence on self-care of the hemodialysis patient. Soc Sci Med 6:1253–1264
ENRICHD Investigators (2000) Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. The ENRICHD investigators. Am Heart J 139:1–9
World Health Organization (2000) International classification of diseases for oncology, 3rd edn. WHO, Geneva
Kinney AY, Bloor LE, Dudley WN, Millikan RC, Marshall E, Martin C, Sandler RS (2003) Roles of religious involvement and social support in the risk of colon cancer among Blacks and Whites. Am J Epidemiol 158:1097–1107
Vilhjalmsson R (1993) Life stress, social support and clinical depression: a reanalysis of the literature. Soc Sci Med 37:331–342
Rozanski A, Blumenthal JA, Davidson KW, Saab OG, Kubzansky L (2005) The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice. The emerging field of behavioral cardiology. J Am Coll Cardiol 637–651
Paykel ES (1994) Life events, social support and depression. Acta Psychiatr Scand Suppl 377:50–58
Kroenke CH, Bennett GG, Fuchs C, Giovannucci E, Kawachi I, Schernhammer E, Holmes MD, Kubzansky LD (2005) Depressive symptoms and prospective incidence of colorectal cancer in women. Am J Epidemiol 162:839–848
Godbout JP, Glaser R (2006) Stress-induced immune dysregulation: implications for wound healing, infectious disease and cancer. J Neuroimmune Pharmacol 1:421–427
Ford DE, Erlinger TP (2004) Depression and C-reactive protein in US adults: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 164:1010–1014
Lieb J, Karmali R, Horrobin D (1983) Elevated levels of prostaglandin E2 and thromboxane B2 in depression. Prostaglandins Leukot Med 10:361–367
Lee KJ, Inoue M, Otani T, Iwasaki M, Sasazuki S (2007) Japan Public Health Center-based Prospective Study. Colorectal cancer screening using fecal occult blood test and subsequent risk of colorectal cancer: a prospective cohort study in Japan. Cancer Detect Prev 31:3–11
Foundation for Promotion of Cancer Research (2008) Cancer Statistics in Japan, 2008. (http://ganjoho.ncc.go.jp/public/statistics/backnumber/2008_en.html)
Honda K, Kagawa-Singer M (2006) Cognitive mediators linking social support networks to colorectal cancer screening adherence. J Behav Med 29:449–460
Okamoto K, Tanaka Y (2004) Gender differences in the relationship between social support and subjective health among elderly persons in Japan. Prev Med 38:318–322
Kawachi I, Berkman LF (2001) Social ties and mental health. J Urban Health 78:458–467
Saito-Nakaya K, Nakaya N, Fujimori M, Akizuki N, Yoshikawa E, Kobayakawa M, Nagai K, Nishiwaki Y, Tsubono Y, Uchitomi Y (2006) Marital status, social support and survival after curative resection in non-small-cell lung cancer. Cancer Sci 97:206–213
Kawamura T, Sobue T (2005) Comparison of breast cancer mortality in five countries: France, Italy, Japan, the UK and the USA from the WHO mortality database (1960–2000). Jpn J Clin Oncol 35:758–759
Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, Ederer F (1993) Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med 328:1365–1371
Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O (1996) Randomised study of screening for colorectal cancer with faecal-occult blood test. Lancet 348:1467–1471
Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, James PD, Mangham CM (1996) Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet 348:1472–1477
Keating NL, O’Malley AJ, Murabito JM, Smith KP, Christakis NA (2011) Minimal social network effects evident in cancer screening behavior. Cancer 117:3045–3052
Acknowledgments
This study was supported by Grants-in-aid for Cancer Research and for the Third Term Comprehensive Ten-Year Strategy for Cancer Control from the Ministry of Health, Labor and Welfare of Japan. The authors thank all staff members in each study area and in the central office for their painstaking efforts to conduct the baseline survey and follow-up. Dr. Ai Ikeda was also supported by the postdoctoral fellowship for Research Abroad of Japan Society for the Promotion of Science (Tokyo, Japan).
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was conducted for the JPHC Study Group.
Appendix: Study group members
Appendix: Study group members
Members of the Japan Public Health Center-based Prospective Study (JPHC Study, principal investigator: S. Tsugane) Group are: S. Tsugane, M. Inoue, T. Sobue, and T. Hanaoka, National Cancer Center, Tokyo; J. Ogata, S. Baba, T. Mannami, A. Okayama, and Y. Kokubo, National Cardiovascular Center, Osaka; K. Miyakawa, F. Saito, A. Koizumi, Y. Sano, I. Hashimoto, and T. Ikuta, Iwate Prefectural Ninohe Public Health Center, Iwate; Y. Miyajima, N. Suzuki, S. Nagasawa, Y. Furusugi, and N. Nagai, Akita Prefectural Yokote Public Health Center, Akita; H. Sanada, Y. Hatayama, F. Kobayashi, H. Uchino, Y. Shirai, T. Kondo, R. Sasaki, Y. Watanabe, Y. Miyagawa, and Y. Kobayashi, Nagano Prefectural Saku Public Health Center, Nagano; Y. Kishimoto, E. Takara, T. Fukuyama, M. Kinjo, M. Irei, and H. Sakiyama, Okinawa Prefectural Chubu Public Health Center, Okinawa; K. Imoto, H. Yazawa, T. Seo, A. Seiko, F. Ito, and F. Shoji, Katsushika Public Health Center, Tokyo; A. Murata, K. Minato, K. Motegi, and T. Fujieda, Ibaraki Prefectural Mito Public Health Center, Ibaraki; K. Matsui, T. Abe, M. Katagiri, and M. Suzuki, Niigata Prefectural Kashiwazaki and Nagaoka Public Health Center, Niigata; M. Doi, A. Terao, Y. Ishikawa, and T. Tagami, Kochi Prefectural Chuo-higashi Public Health Center, Kochi; H. Sueta, H. Doi, M. Urata, N. Okamoto, and F. Ide, Nagasaki Prefectural Kamigoto Public Health Center, Nagasaki; H. Sakiyama, N. Onga, H. Takaesu, and M. Uehara, Okinawa Prefectural Miyako Public Health Center, Okinawa; F. Horii, I. Asano, H. Yamaguchi, K. Aoki, S. Maruyama, M. Ichii, and M. Takano, Osaka Prefectural Suita Public Health Center, Osaka; Y. Tsubono, Tohoku University, Miyagi; K. Suzuki, Research Institute for Brain and Blood Vessels Akita, Akita; Y. Honda, K. Yamagishi, and S. Sakurai, Tsukuba University, Ibaraki; M. Kabuto, National Institute for Environmental Studies, Ibaraki; M. Yamaguchi, Y. Matsumura, S. Sasaki, and S. Watanabe, National Institute of Health and Nutrition, Tokyo; M. Akabane, Tokyo University of Agriculture, Tokyo; T. Kadowaki, Tokyo University, Tokyo; M. Noda, International Medical Center of Japan, Tokyo; Y. Kawaguchi, Tokyo Medical and Dental University, Tokyo; Y. Takashima, Kyorin University, Tokyo; K. Nakamura, Niigata University, Niigata; S. Matsushima and S. Natsukawa, Saku General Hospital, Nagano; H. Shimizu, Sakihae Institute, Gifu; H. Sugimura, Hamamatsu University, Shizuoka; S. Tominaga, Aichi Cancer Center Research Institute, Aichi; H. Iso, Osaka University, Osaka; M. Iida, W. Ajiki, and A. Ioka, Osaka Medical Center for Cancer and Cardiovascular Disease, Osaka; S. Sato, Osaka Medical Center for Health Science and Promotion, Osaka; E. Maruyama, Kobe University, Hyogo; M. Konishi, K. Okada, and I. Saito, Ehime University, Ehime; N. Yasuda, Kochi University, Kochi; S. Kono, Kyushu University, Fukuoka.
Rights and permissions
About this article
Cite this article
Ikeda, A., Kawachi, I., Iso, H. et al. Social support and cancer incidence and mortality: the JPHC study cohort II. Cancer Causes Control 24, 847–860 (2013). https://doi.org/10.1007/s10552-013-0147-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-013-0147-7