Abstract
Purpose
Little is known about breast cancer (BC) survivors’ health-related quality of life (HRQoL) > 5 or even > 10 years past diagnosis. It is of interest whether, in the long run, survivors’ HRQoL aligns with that of the general population. Study objectives were to (1) compare disease-free BC survivors’ HRQoL to that of non-cancer controls, and (2) compare long-term survivors (LTS, 5–9 years post-diagnosis), very long-term survivors (VLTS, ≥ 10 years post-diagnosis), and controls with respect to their HRQoL.
Methods
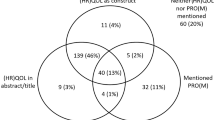
The samples of 2647 disease-free BC survivors (5–16 years post-diagnosis) and 1005 population controls were recruited in German multi-regional population-based studies. HRQoL was assessed by the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire—Core 30 (EORTC QLQ-C30). Differences in HRQoL were assessed with multiple regression, controlling for age and education.
Results
Disease-free BC survivors < 80 years (at survey) reported overall global health status/quality of life comparable to controls, but statistically significant lower physical, role, emotional, social, and cognitive functioning. They also indicated more fatigue, insomnia, dyspnoea, and financial difficulties. However, differences were only of trivial or small clinical relevance. At age 80–89, no differences between BC survivors and controls were observed. Deficits in emotional and cognitive functioning and some symptoms (e.g. insomnia and fatigue) persist, as both LTS and VLTS reported more detriments than controls.
Conclusions
In view of the persistent, small but significant detriments in disease-free BC survivors’ cognitive and emotional functioning and higher symptom burden, possibilities to prevent detriments from becoming chronic should be explored.




Similar content being viewed by others
References
Bericht zum Krebsgeschehen in Deutschland 2016 (2016) Zentrum für Krebsregisterdaten im Robert Koch-Institut (Hrsg). Berlin
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Khan NF, Mant D, Carpenter L, Forman D, Rose PW (2011) Long-term health outcomes in a British cohort of breast, colorectal and prostate cancer survivors: a database study. Br J Cancer 105:S29–S37. https://doi.org/10.1038/bjc.2011.420
Stein KD, Syrjala KL, Andrykowski MA (2008) Physical and psychological long-term and late effects of cancer. Cancer 112(11 Suppl):2577–2592. https://doi.org/10.1002/cncr.23448
Harrington CB, Hansen JA, Moskowitz M, Todd BL, Feuerstein M (2010) It’s not over when it’s over: long-term symptoms in cancer survivors–a systematic review. Int J Psychiatry Med 40(2):163–181. https://doi.org/10.2190/PM.40.2.c
Bantema-Joppe EJ, de Bock GH, Woltman-van Iersel M, Busz DM, Ranchor AV, Langendijk JA, Maduro JH, van den Heuvel ER (2015) The impact of age on changes in quality of life among breast cancer survivors treated with breast-conserving surgery and radiotherapy. Br J Cancer 112(4):636–643. https://doi.org/10.1038/bjc.2014.632
Thong MS, Mols F, Stein KD, Smith T, Coebergh JW, van de Poll-Franse LV (2013) Population-based cancer registries for quality-of-life research: a work-in-progress resource for survivorship studies? Cancer 119(Suppl 11):2109–2123. https://doi.org/10.1002/cncr.28056
Montazeri A (2008) Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res 27(1):32. https://doi.org/10.1186/1756-9966-27-32
Wu HS, Harden JK (2015) Symptom burden and quality of life in survivorship: a review of the literature. Cancer Nurs 38(1):E29–E54. https://doi.org/10.1097/NCC.0000000000000135
Mols F, Vingerhoets AJJM, Coebergh JW, van de Poll-Franse LV (2005) Quality of life among long-term breast cancer survivors: a systematic review. Eur J Cancer 41(17):2613–2619. https://doi.org/10.1016/j.ejca.2005.05.017
Dorval M, Maunsell E, Deschenes L, Brisson J, Masse B (1998) Long-term quality of life after breast cancer: comparison of 8-year survivors with population controls. J Clin Oncol 16(2):487–494. https://doi.org/10.1200/JCO.1998.16.2.487
Hsu T, Ennis M, Hood N, Graham M, Goodwin PJ (2013) Quality of life in long-term breast cancer survivors. J Clin Oncol 31(28):3540–3548. https://doi.org/10.1200/JCO.2012.48.1903
Klein D, Mercier M, Abeilard E, Puyraveau M, Danzon A, Dalstein V, Pozet A, Guizard AV, Henry-Amar M, Velten M (2011) Long-term quality of life after breast cancer: a French registry-based controlled study. Breast Cancer Res Treat 129(1):125–134. https://doi.org/10.1007/s10549-011-1408-3
Helgeson VS, Tomich PL (2005) Surviving cancer: a comparison of 5-year disease-free breast cancer survivors with healthy women. Psycho-Oncol 14(4):307–317. https://doi.org/10.1002/pon.848
Arndt V, Merx H, Sturmer T, Stegmaier C, Ziegler H, Brenner H (2004) Age-specific detriments to quality of life among breast cancer patients one year after diagnosis. Eur J Cancer 40(5):673–680. https://doi.org/10.1016/j.ejca.2003.12.007
Fehlauer F, Tribius S, Mehnert A, Rades D (2005) Health-related quality of life in long term breast cancer survivors treated with breast conserving therapy: impact of age at therapy. Breast Cancer Res Treat 92(3):217–222. https://doi.org/10.1007/s10549-005-2420-2
Koch L, Jansen L, Herrmann A, Stegmaier C, Holleczek B, Singer S, Brenner H, Arndt V (2013) Quality of life in long-term breast cancer survivors—a 10-year longitudinal population-based study. Acta Oncol 52(6):1119–1128. https://doi.org/10.3109/0284186X.2013.774461
Koch L, Bertram H, Eberle A, Holleczek B, Schmid-Höpfner S, Waldmann A, Zeissig SR, Brenner H, Arndt V (2013) Lebensqualität von Langzeitüberlebenden nach Brust-, Darm- und Prostatakrebs. Forum – Deutsche Krebsgesellschaft eV 28(1):43–47. https://doi.org/10.1007/s12312-012-0907-4
Arndt V, Koch-Gallenkamp L, Jansen L, Bertram H, Eberle A, Holleczek B, Schmid-Höpfner S, Waldmann A, Zeissig SR, Brenner H (2017) Quality of life in long-term and very long-term cancer survivors versus population controls in Germany. Acta Oncol 56(2):190–197. https://doi.org/10.1080/0284186X.2016.1266089
Thong MSY, Mols F, Doege D, van de Poll-Franse L, Arndt V (2018) Population-based cancer survivorship research: experiences from Germany and the Netherlands. J Cancer Policy 15:87–91. https://doi.org/10.1016/j.jcpo.2018.02.003
EORTC (2001) EORTC QLQ-C30 Scoring Manual. EORTC, Brussels
Cocks K, King MT, Velikova G, St-James MM, Fayers PM, Brown JM (2011) Evidence-based guidelines for determination of sample size and interpretation of the European organisation for the research and treatment of cancer quality of life questionnaire core 30. J Clin Oncol 29(1):89–96. https://doi.org/10.1200/jco.2010.28.0107
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144. https://doi.org/10.1200/jco.1998.16.1.139
Chu W-o, Dialla PO, Roignot P, Bone-Lepinoy M-C, Poillot M-L, Coutant C, Arveux P, Dabakuyo-Yonli TS (2016) Determinants of quality of life among long-term breast cancer survivors. Qual Life Res 25(8):1981–1990. https://doi.org/10.1007/s11136-016-1248-z
Cimprich B, Ronis DL, Martinez-Ramos G (2002) Age at diagnosis and quality of life in breast cancer survivors. Cancer Practice 10(2):85–93. https://doi.org/10.1046/j.1523-5394.2002.102006.x
Ganz PA, Desmond KA, Leedham B, Rowland JH, Meyerowitz BE, Belin TR (2002) Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer I 94(1):39–49
Schmidt ME, Wiskemann J, Steindorf K (2018) Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual Life Res (27):2077–2086. https://doi.org/10.1007/s11136-018-1866-8
Matthews EE, Berger AM, Schmiege SJ, Cook PF, McCarthy MS, Moore CM, Aloia MS (2014) Cognitive behavioral therapy for insomnia outcomes in women after primary breast cancer treatment: a randomized controlled trial. Oncol Nurs Forum 41(3):241–253. https://doi.org/10.1188/14.ONF.41-03AP
Cohen M, Fried G (2007) Comparing relaxation training and cognitive-behavioral group therapy for women with breast cancer. Res Social Work Practice 17(3):313–323. https://doi.org/10.1177/1049731506293741
Kessels E, Husson O, van der Feltz-Cornelis CM (2018) The effect of exercise on cancer-related fatigue in cancer survivors: a systematic review and meta-analysis. Neuropsychiatr Disease Treat 14. https://doi.org/10.2147/NDT.S150464
Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C (2014) Are exercise programs effective for improving health-related quality of life among cancer survivors? A systematic review and meta-analysis. Oncol Nurs Forum 41(6):638–646. https://doi.org/10.1188/14.ONF.E326-E342
Duijts SFA, Faber MM, Oldenburg HSA, van Beurden M, Aaronson NK (2011) Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors—a meta-analysis. Psycho-Oncol 20(2):115–126. https://doi.org/10.1002/pon.1728
Walker R, Szanton SL, Wenzel J (2015) Working toward normalcy post-treatment: a qualitative study of older adult breast and prostate cancer survivors. Oncol Nurs Forum 42(6):E358–E367. https://doi.org/10.1188/15.onf.e358-e367
Sinding C, Wiernikowski J (2008) Disruption foreclosed: older women’s cancer narratives. Health 12(3):389–411. https://doi.org/10.1177/1363459308090055
Sutin AR, Terracciano A, Milaneschi Y, An Y, Ferrucci L, Zonderman AB (2013) The effect of birth cohort on well-being: the legacy of economic hard times. Psychol Sci 24(3):379–385. https://doi.org/10.1177/0956797612459658
Spuling SM, Wurm S, Tesch-Römer C, Huxhold O (2015) Changing predictors of self-rated health: disentangling age and cohort effects. Psychol Aging 30(2):462–474. https://doi.org/10.1037/a0039111
Funding
This work was supported by two grants from the German Cancer Aid (Nos. 108262 and 110231).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures involving human participants were in accordance with the Helsinki Declaration of 1975, as revised in 1983. Both studies (CAESAR+ and LINDE) were approved by the ethics committee of the medical faculty of the University of Heidelberg and by all local ethics committees accountable for the participating cancer registries.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Doege, D., Thong, M.SY., Koch-Gallenkamp, L. et al. Health-related quality of life in long-term disease-free breast cancer survivors versus female population controls in Germany. Breast Cancer Res Treat 175, 499–510 (2019). https://doi.org/10.1007/s10549-019-05188-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05188-x